What is keratosis?
Let's start with the fact that cutaneous keratosis is a collective term that refers to a whole group of non-inflammatory diseases associated with impaired keratinization of the skin. Clinically, the process can manifest itself as slight peeling or the formation of thickened horny layers. There are follicular, seborrheic, and actinic keratoses.
Keratosis follicularis is characterized by the formation of horny plugs at the openings of hair follicles.
Seborrheic keratoses are plaque-like or nodular formations with a warty surface, covered with dry, horny masses that are flesh-colored, brown, or black in people over 50 years of age.
Actinic keratosis appears on exposed areas of the skin, initially appearing as bumpy, rough skin that eventually develops into rough, scaly patches ranging in color from normal skin tone to reddish brown. They are often limited in size and vary in size.
General information
Hyperkeratosis is a pathological process in the epidermis, which is based on accelerated growth and disruption of the desquamation process of the epidermis, manifested by hypertrophy (thickening) of the stratum corneum. Hyperkeratosis is not an independent disease. Disruption of the keratinization process and thickening of the stratum corneum can occur both in healthy people (on the feet, elbows, knees) and in various diseases ( erythroderma , lichen , ichthyosis , etc.). The process of keratinization, depending on the reasons, can occur in different parts of the body; the thickness of the keratinized layer can vary significantly (from a millimeter to 1-2 centimeters).
What is the stratum corneum of the epidermis?
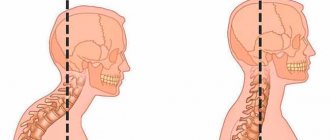
At the base of the stratum corneum of the skin are horny plates containing the protein keratin. In thin skin, the stratum corneum includes 15–20 layers of horny scales, and in thick skin it can contain up to 100 or more layers. The stratum corneum is the final product of the differentiation process of epidermal keratinocytes, which has a specific structure, defined as “brick and cement,” in which horny cells act as “bricks” and intercellular lipids act as “cement.” The leading mechanism of epidermal renewal is the process of desquamation of horny scales and their replacement with new cells. The renewal process begins in the basal layer, producing keratinocytes, which, as they grow older, gradually move (pushed out) to the upper layers, losing the nucleus and organelles, turning into flat scales (corneocytes), forming the stratum corneum (Fig. below).
Thus, the mechanism of cellular renewal is based on the separation (exfoliation) of the upper horn cells, which provokes the activation of dermal cells and the formation of new mother cells of the basal layer. The renewal cycle of epidermal cells averages 21-28 days, but as the body ages, it slows down, amounting to 35-45 days in people over 40 years of age and 56-72 days after 50 years of age. The state and duration of the cellular metabolism cycle also depends on other factors: nutrition/lifestyle, hormonal levels, negative environmental factors.
The renewal process is characteristic not only of the skin epithelium, but also of the mucous membranes of the oral cavity, uterus, and vulva. However, due to differences in the structure of the mucosal epithelium (for the most part, the horny, granular and lucid layers are absent), during the renewal process, incomplete keratinization (parakeratosis) occurs, which is characterized by the appearance of the surface layer of squamous keratin epithelium in the protoplasm of the cells, but nuclei are still present . Parakeratosis is a physiological property of the mucosal epithelium, and is qualified as a pathological process when the morphology of the keratinizing squamous epithelium is disrupted. At the same time, parakeratosis is often combined with hyperkeratosis and acanthosis (increased proliferation of the spinous/basal layers).
Hyperkeratosis is an urgent problem both among men, which is faced by almost 20% of people after 20 years of age, and among women, among whom more than 40% after 20 years of age note this phenomenon on those other areas of the skin that significantly worsen the appearance of the skin (color, structure ). follicular hyperkeratosis occurs predominantly . More often in a child 1-3 years old, the face and hands are affected. In adults, the most common hyperkeratosis of the feet and, in particular, hyperkeratosis of the toenails, subungual hyperkeratosis of the hands, hyperkeratosis of the facial skin and hyperkeratosis of the scalp.
Despite the fact that hyperkeratosis, regardless of its type, is not a potentially life-threatening condition, it requires mandatory treatment, since cosmetic defects/deterioration of the aesthetics of the skin can cause a decrease in self-esteem and contribute to the development of psychological trauma and social maladjustment, especially among women .
For what reasons do acquired keratoses occur?
The main cause of almost all keratoses is said to be chronic exposure to ultraviolet rays. In the literature, all changes associated with sun exposure are often grouped under the term dermatoheliosis. Thus, the damaging effect can affect the epidermis (senile, actinic keratosis), dermis (solar elastosis), blood vessels (telangiectasia), sebaceous glands (porokeratosis) and melanocytes (dyschromia).
The effects of sun damage to the skin gradually accumulate as the total amount of time spent exposed to UV rays increases year after year. This leads to the fact that the peak incidence of this nosology occurs at the age of 50 years and older.
However, nowadays, actinic keratosis has become much more common in young people. As a rule, these are people of the first and second phototypes (with fair skin, blond or red hair, and blue, green or gray eyes). There is a high likelihood of developing keratoses in young people exposed to sunlight for a long time.
The incidence is slightly higher in men because they tend to use little or no sun protection. Clinical studies estimate that about 60 percent of predisposed individuals by the age of forty have at least one element of actinic keratosis. Some experts believe that almost everyone over the age of 80 suffers from some form of keratoses.
In addition, persons whose immune defenses are weakened by chemotherapy, extensive exposure to x-rays or a number of industrial chemicals, patients with AIDS, patients who have undergone organ transplants, patients with disorders of the nervous and endocrine systems, etc. less able to combat the effects of radiation and, therefore, more prone to developing keratoses.
Forecast and prevention of the disease
The prognosis of the disease depends on the time of initiation of treatment. However, in order to avoid relapses, it is necessary to follow certain recommendations.
The following measures can be taken as prevention:
- use moisturizing creams;
- eat well so that food provides the skin with all the necessary “building” elements;
- limit exposure to direct sunlight to reduce exposure to ultraviolet radiation;
- when in the sun, use sunscreens (ointments and creams) with a high SPF level;
- When working with chemicals, you must use appropriate skin protection.
Keratosis is a skin condition that requires constant monitoring. In addition to an aesthetic defect, sometimes formations can develop into malignant tumors. And to prevent this, it is necessary to undergo regular examinations and monitor changes in the skin.
What are the symptoms of this disease? In what areas do they appear most often?
The patient, as a rule, may miss the onset of the disease and not pay attention to small irregularities, roughness, sometimes invisible to the eye, on the skin of the cheeks, bridge of the nose, ears, forearms, upper arms and forearms, back of the hands, back of the neck, upper chest, even on the scalp. Moreover, actinic keratosis can also develop on closed areas of the body that have been repeatedly exposed to the sun.
Developed actinic keratosis is represented by neoplasms from 0.1 cm to 2 cm or more. Over time, the spots become red or brownish in color and flake, and may rise above the skin in the form of growths. We most often see such patients at clinic appointments. Actinic keratosis usually develops very slowly and usually does not cause any discomfort other than aesthetic ones. Itching or burning in the affected area usually occurs in areas of long-term and severe keratinization. Most often, elements of skin keratosis develop slowly, but can disappear and reappear with repeated exposures that damage the skin. They can become inflamed and, in rare cases, even bleed.
Subcutaneous fat
Subcutaneous fat, or hypodermis, is the lowest layer of skin, located under the dermis. It consists of fat lobules separated from each other by connective tissue septa containing collagen and penetrated by large vessels. The main cells of fat lobules are adipocytes, the number of which varies in different areas of the body. Currently, PFA is considered not only as an energy depot, but also as an endocrine organ, the adipocytes of which are involved in the production of a number of hormones (leptin, adiponectin, resistin), cytokines and mediators that affect metabolism, insulin sensitivity, reproductive and immune functional activity. systems
Are there any new developments in this direction on the world market?
Well, for example, from 1998 to the present, the Australian biopharmaceutical company Peplin has been studying the topical treatment of actinic keratosis with the drug Ingenol Mebutate, which is the first in a new class of formulations and is derived from milkweed juice. This ingredient has a long history of traditional use for a variety of skin conditions, including the topical treatment of skin cancer and precancerous skin lesions. The company plans to enter the third phase of the trial soon.
Diagnostics
An appointment with a dermatologist begins with taking an anamnesis. The doctor clarifies how long ago the formation was, asks the patient about sensations - painful manifestations, itching, and studies the symptoms. Next, the skin is examined to determine the size and location of the keratoma. The instrumental method - dermatoscopy - allows you to clarify the diagnosis and exclude other skin diseases.
A special device allows you to identify the formation, examine the structure of its tissues, and the depth of its occurrence. The dermatoscope magnifies the image many times, so errors are excluded. And if there is a risk of the keratoma degenerating into a tumor, the doctor will determine this. In some cases, histology is recommended - the formation is sent to the laboratory to determine the cellular composition.
What are destructive (ablative) methods?
All skin tumors must be examined by a dermatologist before removal due to the risk of skin cancer. Treatment performed in a timely manner will help prevent the development of basal cell carcinoma (BCC) or squamous cell carcinoma of the skin (SCC).
- Cryosurgery using liquid nitrogen is the most common method for treating keratoses, but is not suitable for hyperkeratotic lesions. Liquid nitrogen is sprayed directly onto the affected areas of the skin using a cryodestructor or applied using the “reed” method (application with a cotton swab on a wooden stick). Cryosurgery is easily performed on an outpatient basis, shows excellent cosmetic results and is well tolerated.
- Radio wave, electro- and diathermo-laser destruction.
- Photodynamic therapy involves the application of a photosensitizing agent, methyl aminolevulinate, and then exposure to light of a specific wavelength, which leads to tissue necrosis. Photodynamic therapy is well tolerated and has excellent cosmetic results.
- Surgical removal . The surface of the skin is cleaned with a special instrument (curette).
- Chemical peeling:
- Jessner's solution (resorcinol, lactic and salicylic acids in ethanol);
- trichloroacetic acid solution 35%.
- Dermabrasion . The affected areas of skin are removed using a fast-moving abrasive brush.
- Phototherapy (IPL) and fractional photothermolysis - coagulation of keratosis elements using light energy. Suitable for the initial manifestations of actinic keratosis.
Keratoma: how to treat?
To help the patient get rid of keratoma or actinic keratosis, the doctor prescribes a conservative or surgical treatment method. If drug therapy does not produce results, if the location of the formation is unsuccessful, if it is perceived as a cosmetic defect, surgery to remove the keratoma is prescribed.
Drug therapy
Drug treatment involves the use of various ointments, solutions or emulsions with active substances. It is immediately important to note that such methods are effective in the initial stages, when the stain has just appeared. Therapy must be prescribed by a doctor. Self-medication is strictly not recommended, as it can cause complications in the form of damage to surrounding healthy tissue.
Keratoma: how to remove surgically?
The keratoma is surgically removed using one of the following methods:
- laser method;
- cryodestruction;
- radiosurgery method.
The leader of choice is laser removal, since it minimizes the risks of negative consequences, bleeding, wound infection, and relapses. In a few minutes the formation is completely removed. And the wound heals within a few days.
Possible risks
Attempts to remove the keratoma yourself by tying it with thread or cauterizing it with aggressive media are strictly prohibited. This can lead to serious consequences, including the degeneration of a benign tumor into cancer.