An irreversible phenomenon during which cells, tissues, and organs cease their vital activity is called necrosis. It can be triggered by pathogenic microbes, mechanical, thermal, chemical, infectious and toxic agents that contribute to tissue destruction. In addition, necrosis can occur as a result of allergies or impaired blood circulation. Taking into account the state of the body and unfavorable local factors, it is possible to determine the pronounced degree of cell necrosis.
The provoking factors for the occurrence of necrosis are pathogenic microorganisms, fungi, and viruses. If blood circulation is impaired and there is hypothermia in this part of the body, vascular spasm will increase and severe disruption of blood circulation will occur. With excessive overheating, metabolism increases, and if blood circulation is impaired, the risk of developing a necrotic process increases.
How does necrosis manifest itself?
If we talk about the first symptoms of necrosis, they are presented in the form of numbness and lack of sensitivity. In such a situation, you must immediately visit an experienced and qualified doctor at a medical center. In addition, the skin becomes pale. This happens because blood circulation is impaired. Over time, the skin will acquire a bluish tint, then turn black or dark green. In the presence of necrosis in the lower extremity, a person notices rapid fatigue while walking, a feeling of coldness, cramps appear, as well as lameness, as a result of which non-healing trophic ulcers will form, which will necrotize over time.
Due to the fact that the respiratory and central nervous systems, kidneys, and liver cease to function normally, blood circulation is disrupted, and a person’s general condition of the entire body deteriorates. In addition, the immune system decreases, as concomitant blood diseases, anemia appear, and metabolic processes are disrupted, the body is depleted, hypovitaminosis and fatigue are observed.
Signs
The onset of necrotic processes is characterized by loss of sensitivity in the affected area, numbness of the limbs, and a tingling sensation. The deterioration of blood trophism is indicated by pallor of the skin. The cessation of blood supply to the damaged organ causes the skin color to become bluish and then acquire a dark green or black tint. General intoxication of the body manifests itself in deterioration of well-being, rapid fatigue, and exhaustion of the nervous system. The main symptoms of necrosis are:
- loss of sensation;
- numbness;
- convulsions;
- swelling;
- hyperemia of the skin;
- feeling of coldness in the extremities;
- dysfunction of the respiratory system (shortness of breath, changes in breathing rhythm);
- increased heart rate;
- permanent increase in body temperature.
Microscopic signs of necrosis
The branch of histology devoted to the microscopic study of affected tissues is called pathohistology. Specialists in this field examine sections of organs to identify signs of necrotic damage. Necrosis is characterized by the following changes occurring in cells and intercellular fluid:
- loss of the ability of cells to selectively stain;
- core conversion;
- discomplexation of cells as a result of changes in the properties of the cytoplasm;
- dissolution, disintegration of the interstitial substance.
Loss of the ability of cells to selectively stain, under a microscope looks like a pale, structureless mass, without a clearly defined nucleus. Transformation of the nuclei of cells that have undergone necrotic changes develops in the following directions:
- karyopyknosis - shrinkage of the cell nucleus, which occurs as a result of activation of acid hydrolases and an increase in the concentration of chromatin (the main substance of the cell nucleus);
- hyperchromatosis – redistribution of chromatin clumps occurs and their alignment along the inner shell of the nucleus;
- karyorrhexis - complete rupture of the nucleus, dark blue chromatin clumps are arranged in random order;
- karyolysis – disruption of the chromatin structure of the nucleus, its dissolution;
- vacuolization - vesicles containing clear liquid form in the cell nucleus.
The morphology of leukocytes has a high prognostic value in skin necrosis of infectious origin, for the study of which microscopic studies of the cytoplasm of the affected cells are carried out. Signs characterizing necrotic processes may include the following changes in the cytoplasm:
- plasmolysis – melting of the cytoplasm;
- plasmorrhexis - disintegration of the cell contents into protein clumps; when filled with xanthene dye, the fragment under study turns pink;
- plasmopyknosis – shrinkage of the internal cellular environment;
- hyalinization - compaction of the cytoplasm, its acquisition of homogeneity and glassiness;
- plasma coagulation - as a result of denaturation and coagulation, the rigid structure of protein molecules disintegrates and their natural properties are lost.
As a result of necrotic processes, connective tissue (intermediate substance) undergoes gradual dissolution, liquefaction and decay. Changes observed during histological studies occur in the following order:
- mucoid swelling of collagen fibers – the fibrillar structure is erased due to the accumulation of acidic mucopolysaccharides, which leads to impaired permeability of vascular tissue structures;
- fibrinoid swelling - complete loss of fibrillar striations, atrophy of cells of the interstitial substance;
- fibrinoid necrosis - splitting of the reticular and elastic fibers of the matrix, development of structureless connective tissue.
Varieties
Given the changes that occur in the tissue, there are some forms of necrosis. Namely:
- The cause of coagulation or dry necrosis is the folding, compaction, drying of tissue protein, which then becomes a curdled mass. This is the result of the fact that blood has stopped flowing and moisture has evaporated. Areas of tissue become dry, brittle, and also acquire a dark brown or yellowish gray tint with clear demarcation lines. In the place where the dead tissue was rejected, ulcers will appear, a purulent process will develop, and an abscess will form. The localization of dry necrosis is the spleen, kidneys, and umbilical cord stump in a newborn child.
- With colliculative or wet necrosis, swelling, softening and liquefaction of dead tissue occurs, and a mass with a gray tint is formed and a putrid odor appears.
There are some types of necrosis
1. If the blood supply to a tissue or organ suddenly stops, a heart attack occurs. The term ischemic necrosis refers to the death of any part of a vital organ (brain, heart, intestines, lungs, kidneys, spleen). If the infarction is small, autolytic melting or resorption is observed, followed by tissue restoration. A heart attack can result in impaired tissue functioning, various complications, and even death.
2. If necrosis of a section of bone tissue occurs, the localization of which is the sequestral cavity, this is called sequestration. In such a situation, this area will separate from healthy tissue. The reason for this is a purulent process.
3. Death of the skin, mucous surface, and muscle tissue is called gangrene. The cause of gangrene is tissue necrosis.
4. The presence of bedsores is observed in a person who is completely immobilized. This is explained by prolonged compression of the tissue and damage to the skin. As a result, deep purulent ulcers form.
Stages of the disease
There are several stages of development of this disease. The first stage is characterized by a slight change in bone tissue, when the hip joint maintains functionality, and painful sensations are periodic. At the second stage, cracks begin to form on the surface of the joint, its mobility is impaired, and the person experiences constant pain. The third stage is called secondary arthrosis, when the acetabulum is involved in the process. There is a significant decrease in joint mobility. This stage is manifested by constant and severe pain. At the fourth stage, the bone begins to deteriorate, the muscles atrophy, and the pain is not eliminated by medications.
Symptoms of the disease
Signs of the disease differ depending on the stage.
Early.
The tissues are slightly affected, darkening of the enamel and pale gums may be observed.
Average
. Swelling of the interdental papillae, a gray coating forms on the mucous membrane, and bad breath appears.
Heavy.
Swelling of the gum tissue - it turns black and ulcers appear on it. Appetite disappears, body temperature rises to 39 C°.
Last
. The epithelium dies, severe pain is felt in the gums, the necks of the teeth are exposed, and the dental units become loose.
What is aseptic necrosis of the femoral head
The head of the femur is considered a problem area where there is an increased risk of arterial blockage and cumulative damage caused by overload and household injuries. The presence of various pathological processes can provoke aseptic necrosis of the thigh.
The main reasons include long-term use of hormonal drugs and antibacterial agents. And also, if a person abuses alcohol, he is often in a stressful state. The provoking factor may be the presence of congenital hip dislocation, osteopenia, osteoporosis, systemic lupus erythematosus, ankylosing spondylitis, rheumatoid arthritis.
The majority of cases have a disappointing orthopedic prognosis and the presence of severe deforming arthrosis. In such a situation, the patient is prescribed endoprosthetics, joint arthrodesis or corrective osteotomy. If magnetic resonance imaging is performed in a timely manner, the disease can be detected at an early stage, which can be treated using conservative methods.
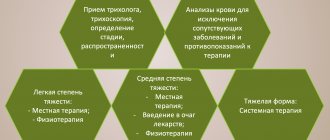
Treatment
Treatment of any type of necrosis will be successful if the disease is detected at an early stage. There are many methods of conservative, gentle and functional treatment; only a highly qualified specialist can determine which one is best suited for the most effective result.
Author of the article:
Mochalov Pavel Alexandrovich |
Doctor of Medical Sciences therapist Education: Moscow Medical Institute named after. I. M. Sechenov, specialty - “General Medicine” in 1991, in 1993 “Occupational diseases”, in 1996 “Therapy”. Our authors
What is necrosis of the hip and knee joints
The hip joint includes the acetabulum and the head of the femur. The hip joint is the largest ball-and-socket joint in the human body. It is supplied by a single artery passing through the neck of the femur.
If blood circulation is disrupted, the blood supply to the area will be disrupted, and oxygen and nutrients will not be supplied, and bone tissue will lose its properties. The recovery process will become impossible, osteoarthritis will appear, which is accompanied by severe pain.
After some time, necrosis of the hip joint develops. In such a situation, the patient needs to replace the damaged joint. For this, an artificial analogue is used. The procedure is called endoprosthetics, when motor activity is completely restored.
Destructive processes in the knee joint occur as a result of injury and loss of blood supply. The joints lose their functions, and the person may become disabled. With aseptic necrosis of the knee joint, a person experiences severe pain and observes that the motor ability of the knee has decreased. Magnetic resonance imaging and bone scanning can detect early changes, thereby preventing further bone loss.
Using non-steroidal anti-inflammatory drugs can get rid of pain and reduce inflammation. If a person is indicated for surgery, a bone transplant will be performed.
Causes
The cessation of the vital activity of cells occurs under the influence of changed external conditions of the organism’s existence or as a result of pathological processes occurring within it. The causative factors for the occurrence of necrosis are classified in terms of their exogenous and endogenous nature. Endogenous reasons why tissue can die include:
- vascular – disturbances in the functioning of the cardiovascular system, which led to disruption of the blood supply to tissues, deterioration of blood circulation;
- trophic - changes in the mechanism of cellular nutrition, disruption of the process of ensuring the preservation of the structure and functionality of cells (for example, skin necrosis after surgery, long-term non-healing ulcers);
- metabolic – disruption of metabolic processes due to the absence or insufficient production of certain enzymes, changes in general metabolism;
- allergic – a highly intense reaction of the body to conditionally safe substances, the result of which is irreversible intracellular processes.
Exogenous pathogenic factors are caused by the impact on the body of external causes, such as:
- mechanical – damage to tissue integrity (wound, trauma);
- physical – impairment of functionality due to exposure to physical phenomena (electric current, radiation, ionizing radiation, very high or low temperature – frostbite, burn);
- chemical – irritation by chemical compounds;
- toxic - damage by acids, alkalis, salts of heavy metals, drugs;
- biological – destruction of cells under the influence of pathogenic microorganisms (bacteria, viruses, fungi) and the toxins they secrete.
What is necrosis of the talus and humerus?
With this disease, painful sensations appear in the shoulder joint, its movement is limited, as a result of which the risk of atrophy increases. A rare phenomenon includes an altered structure of the humerus. As the disease progresses, the patient is prescribed surgical intervention, which is called endoprosthetics. In this situation, this is the only way to restore lost functions of the upper limbs.
Necrosis of the talus occurs spontaneously and rapidly progresses. With degenerative changes in the ankle joint, deforming arthrosis develops. Thanks to modern diagnostic methods used in the medical center, it is possible to determine the early stage of changes in the ankle joint. In such a situation, mosaic osteochondroplasty is used, as a result of which the anatomy of the joint is restored.
Diagnostic measures
If necrosis is suspected, the patient may be sent for an X-ray examination. However, it should be taken into account that this method does not detect pathology at the initial stage of development. An X-ray can reveal pathology if it has progressed to the second or third stage. During the study of this disease, taking a blood test will also not bring an effective result. Thanks to modern devices that are used for magnetic resonance and computed tomography, it is possible to detect changes in tissue structure in a timely manner and with maximum accuracy.
How does necrosis end?
A favorable outcome of the pathology will be with enzymatic melting of tissues, germination of connective tissues into the remaining dead tissue, followed by the formation of a scar. The area of necrosis can become overgrown with connective tissue, resulting in the formation of a capsule. In addition, bone can form in the dead area. This phenomenon is called ossification.
An unfavorable outcome of the pathological condition is characterized by purulent melting, as a result of which the risk of bleeding and spread of the lesion increases. This is how sepsis will develop.
With ischemic stroke, myocardial infarction, necrosis of the kidney or pancreas, that is, when vital organs are affected, there is a high probability of death.
Preventive measures
Knowing the fundamental risk factors for the occurrence of necrotic processes, preventive measures should be taken to prevent the development of pathology. Along with the recommended measures, it is necessary to regularly diagnose the condition of organs and systems, and if suspicious signs are detected, seek advice from a specialist. Prevention of pathological cellular changes is:
- reducing the risk of injury;
- strengthening the vascular system;
- increasing the body's defenses;
- timely treatment of infectious diseases, acute respiratory viral infection (ARVI), chronic diseases.