Constant nasal congestion, persistent runny nose... We all know how unpleasant and debilitating such a condition can be. Meanwhile, the reason does not always lie in the runny nose or cold itself. One of the factors that provoke constant nasal congestion may be hypertrophy of the nasal turbinates. Symptoms of turbinate hypertrophy are very similar to those of allergic and chronic rhinitis. Treatment of turbinate hypertrophy depends on the cause of the development of this condition, and may include both conservative and surgical methods. We will talk in more detail about the nature, symptoms, as well as methods of treatment and diagnosis of this disease below.
The turbinates are spongy bony structures located in the nasal cavity on the side wall that guide and regulate air flow in the nasal passages. A person has three such paired bony outgrowths on both sides of the nasal septum, which are divided into upper, lower and middle. The turbinates are covered with ciliated epithelium, a special type of mucous membrane that cleans and moisturizes the air passing through the nose. The epithelium also serves as an immunological defense against bacterial and chemical irritants, its cells causing a rapid immune response in the form of an inflammatory reaction to the first signs of microbial or chemical irritation.
SUMMARY
Over the past 130 years, at least 13 surgical techniques have been used to treat inferior turbinate hypertrophy. This article reviews and critically analyzes these methods. Our review of the literature revealed a serious lack of qualified research. There are very few prospective comparative randomized surgical outcome measures. In our opinion, the goal of inferior turbinate surgery should be to reduce complaints while maintaining function. From the above it follows that, apparently, electrocautery, chemical caustic, turbinectomy (subtotal), cryosurgery, and superficial laser surgery should not be used, since these technologies are too destructive. Intraturbinal reduction of conchae (intraturbinal turbinoplasty) seems to be the method of choice.
INTRODUCTION
One of the main causes of chronic nasal congestion is the pathology of the inferior turbinates. However, today there is no agreement on solving this problem. The method of choice is mainly pharmacological treatment. In most cases, nasal topical steroids, antihistamines, and decongestants provide good results. Patients who do not respond to this treatment usually undergo turbinate reduction surgery. Since the last quarter of the 19th century, at least 13 different technologies have been introduced. Some of them have already been abandoned, while others are still in use or have been reintroduced. There is, however, considerable disagreement about the merits of various technologies (Jackson and Koch, 1999).
Some authors consider conchotomy as the most acceptable method of treatment, while others condemn it as too aggressive and irreversibly destructive. Another controversial technology is laser treatment. Although a number of authors have recently advocated this technique, many rhinologists do not approve of it, since the laser destroys the mucous membrane and consequently reduces its functioning. In light of this and other controversies, this article reviews and evaluates publications on the surgical treatment of hypertrophied turbinates.
Vasotomy and correction of the nasal septum
In cases where the cause of breathing problems, in addition to problems with the mucous membrane, is a deviated nasal septum, the surgeon can also perform septoplasty during the operation. This surgical intervention is more complex, is performed only under general anesthesia, and requires the patient to be hospitalized for 1-2 days.
The recovery period after this operation lasts 14-20 days, it may be accompanied by an increase in temperature, separation of mucus and ichor. You must see a doctor at least once during postoperative rehabilitation.
FUNCTIONS OF THE NASAL TUNCHANTS
To critically evaluate the various methods of turbinate reduction, we must first understand the function of the turbinates. We will then define the criteria that surgical techniques must meet to be considered acceptable.
The nasal turbinates, especially the inferior ones, perform several important functions. First, they contribute to inspiratory resistance, which is necessary for normal breathing. The greater the nasal resistance, the greater the negative intrathoracic pressure required for inspiration. The large negative pressure, in turn, increases pulmonary ventilation and venous return to the lungs and heart (Butler, 1960; Haight and Cole, 1983). This is what we would call the "resistive function" of the turbinates. Second, as part of the nasal valve, the inferior turbinate helps convert inspiratory airflow from laminar to turbulent. Turbulence in the outer layers of air increases the interaction between the air and the nasal mucosa. This improves humidification, warming and air purification. Due to the large surface of the mucous membrane and extensive blood supply, the inferior conchae play a large role in this process. This role can be called the "diffuser function" of the inferior turbinates. Finally, they are important in the nasal defense system (mucociliary transport, humoral and cellular defense). All of these functions require large amounts of normally functioning mucosa, submucosa, and turbinate parenchyma.
CRITERIA FOR EVALUATING METHODS FOR REDUCING THE VOLUME OF NASAL TURNACLES
All methods must be assessed according to two main criteria:
- The effectiveness of the technology to reduce difficulty breathing, hypersecretion, sneezing and headaches;
- Side effects that occur in the immediate and long term. In other words, the extent to which the functional tasks of the nose are respected and preserved. It would be a mistake to focus solely on the degree of dilation of the nasal passages based on endoscopic findings, rhinomanometry, and acoustic rhinometry. A wider nasal cavity does not necessarily mean that the nose works better. The goal of surgical treatment should be “elimination of complaints while maintaining function” and “optimal amount of reduction while maintaining function” (Huizing, 1998). Taking this concept as a basis, this review evaluates various inferior turbinate reduction techniques used in the past or currently in use. They are described briefly and critically assessed in chronological order. A basic overview of the sources is presented in Table 1.
Table 1. Various treatments for inferior turbinate hypertrophy
| Method | Year of implementation | Used | Left |
| Thermal coagulation, electrocautery | 1845–1880 | + | |
| Chemical coagulation, chemocaustics | 1869–1890 | + | |
| Turbinectomy | 1882 | + | |
| Lateralization, lateropexy | 1904 | + | |
| Submucosal bone resection | 1906–1911 | + | |
| Crush+flatten, partial resection | 1930–1953 | + | |
| Corticosteroid injections | 1952 | + | |
| Injections of sclerosing drugs | 1953 | + | |
| Videoneurectomy | 1961 | + | |
| Cryosurgery | 1970 | + | |
| Turbinoplasty | 1982 | + | |
| Laser surgery | 1977 | + | |
| Power tools | 1994 | + |
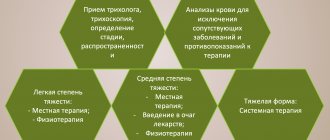
METHODS FOR DIAGNOSIS OF HYPERTROPHY OF THE NASAL TUNCENTS
- History taking and physical examination. During the examination, complaints are clarified and the nose is examined using a rhinoscope - a special dilator.
- Nasal endoscopy. Nasal endoscopy is a minimally invasive medical procedure performed to diagnose nasal diseases. It helps to examine the inner lining of the nose and visualize its cavity, which is impossible to do with a regular examination. The procedure is performed using a nasal endoscope, which consists of a thin, flexible tube with fiber optics to illuminate the nasal cavity. The endoscope is connected to a light source and a video camera, which sends images to a monitor. During an endoscopy, pictures may be taken or recorded for further examination.
THERMAL COAGULATION - ELECTROCAUSTIC
The first method for treating hypertrophied inferior turbinates was electrocautery. Already in 1845, its use was supported by Heider from Vienna and Krusel from St. Petersburg. After the dissertation of Middeldorpff (1854) and the work of Bruns and Voltolini (1871), this method gradually gained popularity. It eventually gained widespread use following the introduction of cocaine as a local anesthetic (Koller, 1884) and adrenaline (epinephrine) as a vasoconstrictor (1897). In the 1880s, electrocautery of the nasal mucosa was used not only to treat nasal diseases, but also to treat other ailments such as dysmenorrhea, abortion, gastralgia, etc. In those days, "nasal reflex neurosis" (Fliess, 1893) was a common superstition. Electrocautery has increasingly been criticized for its need for repetition and because it leads to serious complications such as synechiae and stenosis. In 1890, at the World Congress in Berlin, this procedure became the target of ridicule: “And then the nose is burned out, because, as we know, this always helps!”
Surface electrocaustics. The first method was galvanocaustics using a galvanic apparatus (Voltolini, 1871). The standard technique consists of coagulation from back to front with two parallel grooves along the medial surface of the concha. High temperature coagulates the tissue, causing necrosis, which leads to fibrosis and shrinkage of the shell (Figure 1). While bleeding is rare, temporary complaints of crusting are noted. Over time, various types of electroplating tools have been developed. Later, high-frequency surface diathermy was introduced (e.g., Bourgeois and Poyet, 1922; Castex, 1929; Sinskey, 1932; Jaros, 1933). This technology has been used for both zonal tissue destruction and linear coagulation.
Figure 1. Surface electrocautery technique (from the textbook Laurens, 1924)
Surface electrocautery is a clearly destructive procedure. It causes mucosal atrophy, metaplasia, loss of cilia and decreased mucociliary transport. Permanent crusts and synechiae may form between the nasal septum and the turbinates. Although these undesirable effects are known, it remains one of the most commonly used methods in practice.
Coblation (“controlled ablation”) is a very recently introduced method of high-frequency bipolar diathermy. Because the results are achieved at low temperatures, damage to surrounding tissue is minimized (Smith et al., 1999).
Intraturbinal coagulation. Since superficial electrocautery causes significant damage to the mucous membrane, intraturbinal thermocoagulation was introduced. Neres (1907) introduced a gold needle during this procedure and then passed a galvanic current for several seconds. Horn in 1908 described a similar submucosal technology. Later, high-frequency diathermy was introduced. Beck in 1930 was apparently the first to describe the use of a monopolar electrode for submucosal linear burning. Hurd first reported bipolar intraturbinal diathermy in 1931. Two parallel wires were inserted through the anterior incision into the depth of the shell (Figure 2). Then horizontal parallel grooves 2-4 mm deep are burned into the shell tissue in the direction from back to front. After World War 2, Richardson (1948) and Shahinian (1953) again reported submucosal diathermy. Like the Hurd, they both used a bipolar electrode to ensure precise current delivery. Simpson and Grooves (1958) advocated the use of a monopolar electrode because a single wire is easier to position. The effect of submucosal diathermy is achieved by coagulation of the venous sinuses within the concha, resulting in submucosal fibrosis (Woodhead et al., 1989). This method has several disadvantages. Firstly, it is difficult to dose the volume of tissue treated in depth (Wengraf et al., 1986). Second, the results are often temporary, requiring the procedure to be repeated (Jones and Lancer, 1987; Meredith, 1988). The most common complications are late bleeding, prolonged nasal discharge and crusting (Meredith, 1988; Williams et al., 1991). Despite these disadvantages, submucosal diathermy remains the treatment of choice for most ENT physicians, simply because of its ease of performance and relatively rare complications.
Figure 2. Bipolar intraturbinal coagulator (after Hurd, 1931)
Radiofrequency turbinate reduction (RTR)
During this procedure, the doctor performs local anesthesia of the nasal cavity, after which the patient is positioned on the treatment table and the doctor performs radiofrequency reduction of the nasal turbinates using a special electrode. The principle of operation of RTR is based on short-term heating of the tissues of the nasal concha with an electrode, which leads to their compression and expansion of the respiratory passages.
What a patient should expect when undergoing the procedure in Singapore:
- Preparing for RTR only takes 15-20 minutes;
- The procedure is mostly painless and minimally uncomfortable;
- Immediately after the procedure, the patient may not experience significant relief from congestion due to slight swelling and crusting. However, immediately after the cleaning (which is performed by the doctor a few days after the procedure), the patient will be able to experience the full benefits of radiofrequency turbinate reduction;
- The procedure does not require hospitalization - the doctor performs it on an outpatient basis in the clinic. Immediately upon completion, the patient can return to his daily activities;
- The period of complete recovery and healing takes about 4-6 weeks;
- During the first few days after the procedure, patients are not recommended to swim in the pool.
CHEMICAL COAGULATION - CHEMOCAUSTICS
The use of chemical coagulation of the surface of shells in order to reduce their size also came into practice in the last decades of the 19th century. First, a saturated solution of trichloroacetic acid (TCA) was used, which was applied to the mucous membrane (eg, von Stein, 1889); later, chromic acid melted to form a pearl was also used (Figure 3). As early as 1903, doubts arose about the merits of chemical coagulation. In most clinics the results were described as positive, but microscopic examination revealed severe necrosis of the mucous membrane (Meyer, 1903). This author recommended intensive application of TCA, with the assumption that the epithelium would recover better as new epithelium outgrew the necrotic tissue.
Figure 3. Melting chromic acid into a pearl for chemocaustics of the mucosal surface (from the textbook Seiffert, 1936)
This method is becoming less and less popular. Due to its limited effect on the volume of the turbinates, this procedure requires repetition several times. Secondly, this technique leads to serious damage to the nasal mucosa with characteristic symptoms of atrophic rhinitis.
Taking into account the “optimal amount of reduction while preserving function”, this technology should be strictly prohibited. This technique is the worst thing imaginable: while the shells are only slightly reduced, it causes massive destruction of the functional structures of the mucous membrane, cilia and glands. It is noteworthy that this method has recently been advocated as safe and effective in reducing hypersecretion in patients with nasal hyperreactivity and allergies (Yao et al., 1988, 1995).
What are the dangers of nasal turbinate pathologies?
A dangerous feature of any changes in the structure of the turbinate mucosa is that, due to difficulty in nasal breathing, the affected person is constantly forced to use vasoconstrictor sprays and drops. The use of such drugs, which continues for a long time, can cause a number of complications:
- chronic hypoxia;
- the formation of dry rhinitis in a chronic form, when crusts form in the nasal cavity, and fluid with ichor is separated from the nose;
- damage to the ciliated epithelium;
- chronic nasal spasm, due to which a person develops hypertension;
- obstructed patency of the auditory tubes and pathological processes in the paranasal sinuses and structures of the middle ear.
CONCHOTOMY
Resection and surgical reduction of turbinates has been known since the last decades of the 19th century. To our knowledge, Jarvis (1882) was the first to describe resection of parts of the inferior concha using a wire loop. Then in the 1890s, Hartmann described his experience with operations on the inferior conchae (cited in Mabry, 1988). Later, Jones (1895) and Holmes (1900) proposed total conchotomy. This method of irreversible resection was soon criticized. Spielberg (1924), for example, warned fanatical rhinologists who would not rest until they had removed, resected, or cauterized every mass they found in the nasal cavity. The disadvantages of conchotomy were obvious. Some patients suffered from atrophic rhinitis or what is known as secondary ozena with symptoms of nasal dryness, crusting, bleeding, soreness and headache (eg Dutrow, 1935; Harris, 1936; House, 1951; Tremble, 1960). Conchotomy was discredited; many surgeons have opted for more conservative techniques such as lateralization and submucosal resection. However, total conchotomy was again recommended by several authors in the 1970s and 1980s (Fry, 1973; Courtiss et al., 1978; Martinez et al., 1983; Pollock and Rohrich, 1984; Ophir et al., 1985; Odetoyinbo, 1987; Thompson, 1989; Wight et al., 1990). Some of these authors disputed the claim that conchotomy leads to post-turbinectomy syndrome, or “empty nose” syndrome as it has recently been called (Stenquist and Kern, 1997). The rationale was that this undesirable postoperative effect was never reported by Courtiss and Goldwyn (1990), who wrote: “The fear of dry nose syndrome is unfounded.” Others disagree, reporting long-lasting signs and symptoms of crusting, dryness, and pain in some patients (Moore et al., 1985; Salam and Wengraf, 1993; Garth et al., 1995; Neves-Pinto, 1995; Berenholz et al. , 1998). An overview of controversial reports is presented in Table 2.
Table 2. Development of dryness and crusting after (sub)total resection of the inferior turbinates according to recent studies
| Author | Dryness and crusts |
| Courtiss and Goldwyn '83, '90 | NO |
| Martinez et al. '83 | NO |
| Moore et al. '85 | YES |
| Ophir '85, '90 | NO |
| Odetoyinbo '87 | NO |
| Thompson '89 | NO |
| White '90 | YES |
| Salam and Wengraf '93 | YES |
| Carrie et al. '96 | YES |
| Berenholz '98 | YES |
Recurrent nasal congestion has already been reported (Otsuka et al., 1988; Wight et al., 1990; Carrie et al., 1996). In addition to long-term consequences, early complications, especially severe bleeding, must be taken into account (Fry, 1973; Dawes, 1987).
In our opinion, in patients with hypertrophy of the inferior turbinates, total or subtotal conchotomy is not justified. Conchotomy is incompatible with the “preservation of function” task. Conchotomy is irreversible and deprives the nose of one of its important organs. Thus, there is no place for this technology in modern functional nasal surgery. To achieve the desired effect, there are more conservative surgical methods. This view was recently confirmed in a comparative randomized trial by Passali et al. (1999). These authors compared the long-term results of six different technologies using patient symptom severity scores, rhinomanometry, acoustic rhinometry, mucociliary clearance measurements, and secretory IgA measurements before and after surgery. The topic of turbinectomy is closed, since this is the most traumatic technology (Table 3).
Table 3. Main results of a prospective randomized study of six different methods of reduction of the inferior turbinates, as concluded by Passali et al., (1999)
| Technology | Effect on nasal congestion | Recurrence of nasal congestion | Effect on function | Complications |
| Electrocaustics | + | + | – | + |
| Cryosurgery | + | + | – | + |
| Laser surgery | + | + | = | + |
| Submucosal reduction | + | + | = | + |
| The same + lateralization | + | – | = | 0 |
| Turbinectomy | + | – | – | 0 |
Operation conchotomy of the nasal cavities
Preparation
Before conchotomy, the nasal mucosa is pre-treated with a solution of lidocaine and adrenaline, and infiltration anesthesia is performed. During the intervention, the patient is usually in a lying position on the operating table, with the head slightly elevated, or in a sitting position in a chair. The skin of the nasal vestibule is wiped with alcohol or other antiseptics. The operated area is limited to sterile drapes.
Manipulation options
The surgeon’s manipulations are limited to removing fibrous and polypous areas, while healthy tissue remains, as far as possible, unchanged. Such gentle resection is carried out using surgical scissors and forceps. Begin by removing the free edge of the shell along its entire length. Then carefully grab the hypertrophied part with a loop and cut it off. The doctor takes special care when working with forceps, since rough tears of the mucous membrane can lead to bleeding and poor postoperative wound healing.
In some cases, they resort to submucosal conchotomy. The technique involves preliminary performing a vertical approach, going from the anterior edge of the shell to the bone part. After separation of the mucous membrane using a conchotome, the bone is removed and then the mucous membrane is put back in its original place.
| a - resection of the inferior concha b - resection of the anterior end of the middle concha |
If, according to indications, it is necessary to remove the front end of the shell, then use scissors in the form of an arc with curved ends. A loop is inserted into the incision, which then cuts off the hypertrophied part of the shell. If there is a history of pneumatic cells, they are surgically removed. For this purpose, a conchot is usually used, which can be replaced with forceps.
LATERALIZATION, LATEROPEXY
In response to the side effects of conchotomy, Killian proposed lateralization of the inferior turbinate in 1904. The concha was broken and displaced laterally by a flat elevator or nasal planum with long branches. This procedure is simple and does not have any particular risks or complications (Salam and Wengraf, 1993). On the other hand, it does not seem particularly effective. Lateralization is performed well when the inferior meatus is wide enough to move the inferior concha. Otherwise, she tends to take her previous position (Goode, 1978). Lateralization is an acceptable technique in terms of preserving function. Since its effect is limited, it can be used as an additional procedure, for example, in combination with septal surgery.
Lateropexy (or conchopexy) involves moving the fractured concha into the maxillary sinus after removing part of the lateral wall of the nose (Fateen, 1967; Legler, 1974, 1976). It is quite clear that this method has not gained much popularity.
Recovery after the procedure
After the operation, there is no need to frequently change tampons since the risk of bleeding after vasotomy is minimal. It is possible to rinse the nasal passages with a small amount of warm water, and inhalations can be taken to improve healing. It is recommended to postpone fitness classes, jogging, physical stress, going to the bathhouse and sauna, swimming in a hot bath, taking sun treatments, and drinking alcoholic beverages for a while. This may cause bleeding. It is also not advisable to vigorously blow your nose and clear your nasal passages using force.
SUBMUCOUS RESECTION OF THE BONE OF THE INNER TUNALE
Complications after conchotomy have forced a number of surgeons to look for more conservative surgical methods to reduce the size of the inferior turbinate. The first surgical alternative presented was submucosal resection of the inferior turbinate bone (Low, 1906; Linhart, 1908; Würdemann, 1908; Zarniko, 1910). Würdemann stated that he was “irritated by almost every case of complete removal of the turbinate” and wanted to “prevent disastrous results.” A milder version of this new concept was described by Freer in 1911: “to submucosally elevate the membrane of the inferior turbinate with a sharp elevator, a fairly small vertical incision is made, and further exposed with a sharp raspator, this approach permits a longitudinal resection of the inferior turbinate” (Figure 4). Although convincing, this technique received only limited use (Strandberg, 1924; Odeneal, 1930; Harris, 1936). In 1951, Howard House revived this method. Good results were later reported by Loibl and Pfretzschner (1972) and Tolsdorff (1981), who combined this method with lateral displacement. Mabry (1982, 1984) refined this technique and coined the term “turbinoplasty.” Observing patients after surgery for a year, he found that the size and function of the shells remained normal. In a study conducted by Passali et al. (1999), submucosal bone resection combined with lateral displacement was rated as the best method in terms of effectiveness and preservation of function.
Figure 4. Intraturbinal resection of the bone and parenchyma of the inferior turbinate through a vertical incision (a) of the head of the concha (after Freer, 1911)
CORTICOSTEROID INJECTION
In 1952, injections of long-acting corticosteroid solutions were introduced as a new technique for reducing hypertrophied turbinates (Semenov, 1952). A number of authors have reported that corticosteroid injections are effective in eliminating nasal hyperresponsiveness, regardless of etiology (Semenov, 1952; Simmons, 1960, 1964; Baker and Strauss, 1963). Corticosteroid injections are minimally invasive, but the subjective improvement in nasal breathing is short-lived. This procedure successfully reduces turbinate swelling for only 3 to 6 weeks (Mabry, 1979, 1981). Later, most authors rejected concha injections because they can cause acute homolateral blindness (Baker, 1979; Byers, 1979; Evans et al., 1980; Mabry, 1982; Saunders, 1982; Rettinger and Christ, 1989).
The essence of the vascular vasotomy procedure, indications and contraindications for its use
Submucosal vasotomy is a process of surgical intervention on the vascular connections lining the cavities of the nasal turbinates. Thanks to its implementation, it is possible to significantly reduce the size of the mucous membrane, thereby facilitating the process of nasal breathing for the person being operated on.
Indications for vasotomy are:
- chronic rhinitis in cases where the variant of its allergic etiology is excluded;
- diagnosed hypertrophy of the nasal mucosa;
- deviated nasal septum;
- dependence on vasoconstrictor drugs.
In what cases is the operation impossible? Doctors identify the following contraindications to vasotomy:
- blood clotting disorders that cannot be corrected;
- acute infectious lesions;
- atrophic and ulcerative lesions of the nasal mucosa;
- cardiac, hepatic, renal failure in the stage of decompensation;
- diabetes;
- period of menstrual flow in women.
NEUROECTOMY OF THE VIDIAN NERVE
In 1961, Golding-Wood took a fundamentally new approach to solving the problem. He proposed cutting the parasympathetic nerve fibers in the Vidian canal to reduce the parasympathetic tone of the nasal mucosa. In this way he hoped to reduce the symptoms of hypersecretion and nasal congestion. This technology was developed in an era when drug treatment for hypersecretion was still very limited. Subsequently, various approaches to the Vidian Canal were developed. Initially, the transantral approach was used (Golding-Wood, 1973; Ogale et al., 1988), later supplemented by the endonasal method with ganglion coagulation (Portmann et al., 1982). Neuroectomy of the Vidian nerve has been widely used, but its effect has been limited (Krant et al., 1979; Krajina, 1989). Hypersecretion was reduced, but not nasal congestion (Principato, 1979). For these reasons, this technology was abandoned in the early 1980s.
CRYOSURGERY
Cryosurgery was introduced in the 1970s by Ozenberger (1970). This method involves freezing the shell under local anesthesia with a cryoprobe using nitrous oxide or liquid nitrogen as a cooling agent. Necrosis after freezing was found to be different from that after caustic. It was assumed that the necrotic tissue would be replaced by new respiratory epithelium. Although the method has become widespread, published results have varied (Grache and Holopainen, 1971; Puhakka and Rantanen, 1977; Principato, 1979; Bumstead, 1984; Chiossone et al., 1990, Hartley and Willatt, 1995). The immediate results were largely satisfactory, but the outcome was not durable (Warwick-Brown and Marks, 1987; Haight and Gardiner, 1989; Rakover and Rosen, 1996). According to Puhakka and Rantanen (1977), performance improves after repeated applications.
Other than transient headache, no postoperative sequelae have been reported (Moore and Bicknell, 1980). One month after surgery, there is a marked reduction in the orifices of the glands, scar tissue has formed, and the ciliated epithelium appears normal (Principato, 1979; Keller-hans and Schlageter, 1988). However, in some studies, mucociliary clearance did not return to normal (Wengraf et al., 1986; Elwany and Harrison, 1990). According to some authors, cryosurgery would be more effective for allergic rhinitis than for non-allergic turbinate hypertrophy, since it is particularly effective in controlling rhinorrhea (Principato, 1979; Rakover and Rosen, 1996).
Cryosurgery was gradually abandoned for a number of reasons. It is difficult to predict the amount of tissue removed. Moreover, compared with other methods, long-term results are disappointing, as recently confirmed by studies by Passali et al. (1999).
CRUSHING AND LEVELING - PARTIAL RESECTION
The long-term complications of total turbinectomy have convinced most rhinosurgeons that partial resection of the inferior turbinate would be the best choice. Several technologies have been proposed - trimming, horizontal and diagonal resection of the lower edge; resection of the posterior part and resection of the anterior part.
In 1930, Kressner introduced crushing of the shell with specially designed blunt forceps and then straightening it. Since then, this method has been used by several surgeons. This technology was successfully used in our department (Huizing, 1988).
Resection of the posterior end of the concha was proposed, among others, by Proetz (1953), since he believed that in most cases it is the posterior half of the inferior turbinate that causes difficulty in nasal breathing.
Goode (1978), Pollock and Rohrich (1984), Fanous (1986), and many others have advocated resection of the anterior portion of the inferior turbinate. Unlike Proetz, they considered the head of the inferior turbinate as the most common obstruction to breathing.
Horizontal inferior resection of the inferior margin was recommended by Courtiss and Goldwyn (1990), Dessi et al. (1992), Ophir et al. (1992), Percodani et al. (1996). This method avoids the risk of bleeding from the pterygopalatine artery (Garth et al., 1995). Some authors argue that it only partially solves the problem because symptoms return (often due to new hyperplasia) and the outcome worsens over time (Courtiss and Goldwyn, 1983, 1990; Warwick-Brown and Marks, 1987; Wight et al ., 1990; Schmelzer et al., 1999).
Spector (1982) proposed diagonal resection of most of the turbinate. With this method, the functionally important head of the inferior turbinate is preserved. Severe bleeding from the posterior nasal cavity may occur as this technique cuts off a large source of blood supply to the turbinate (Padgham and Vaughan-Jones, 1991).
From a function preservation perspective, all of the partial turbinectomy options discussed above appear acceptable if performed in a gentle manner. We particularly prefer shell crushing followed by horizontal leveling, as this technique seems to be the best compromise between the desired result and side effects. In our opinion, resection of the head of the concha appears to be too destructive. It can relieve anterior obstruction, but partially deprives the nose of its resistive and diffuser functions. Resection of part of the posterior end of the concha appears functionally acceptable, but is effective only in patients with pathology limited to the tail of the concha.
In the first part of the work, we talked about the anatomy, physiology and biomechanics of the nasal valve (NV), as well as the diagnosis of its problems. The presented section of the work is devoted to the treatment of NK deficiency.
Conservative treatment of nasal valve dysfunction
Several attempts have been made to influence the condition of the nasal valve (NV) without surgery. At one time, M. Vaiman et al. [1], using intranasal electromyography, came to the conclusion that the functional activity of the nasal muscles affects the functioning of the NC. People with developed nasal muscles have better nasal breathing compared to those whose nasal muscles are in a rudimentary state. Based on this principle, a method of training the nasal muscles using the principle of “biological feedback” was proposed, and even encouraging results were obtained. However, no other evidence of the effectiveness of the method has yet been reported.
M. Friedman et al. [2] used the method of NK correction using Breath-right dilator strips, also using them to determine indications for surgery. The strips significantly improved nasal breathing, but were not as effective as subsequent surgery. L. Hoyvol et al. [3] compared the effect of dilator strips on nasal breathing with xylometazoline spray and found that both methods equally improved nasal breathing. Due to the large number of side effects from the use of vasoconstrictor drops, mechanical NK dilators are recommended to be used as an alternative to decongestants.
H. Riechelman et al. [4] conducted a prospective controlled study of the effectiveness of a nasal dilator (Nasanita) in healthy volunteers and patients with external NA failure. As a result, it was found that the nasal dilator effectively expands the external nasal passages and improves nasal breathing.
One of the methods of non-surgical correction for NK deficiency is the introduction of a so-called “filler” - a special biocompatible gel based on hyaluronic acid [5]. 0.2 ml of gel is injected into the NK area on each side, while its angle changes and expands. The procedure is repeated after 10-15 days. The authors do not provide any data on the effectiveness of the method. The main disadvantage of this method is its temporary effect - hyaluronic acid is completely absorbed after 12-18 months. Complications include the development of subcutaneous hemorrhage, swelling of the nasal tip and, in rare cases, erythema of the external nose [5].
It is clear that both fillers and mechanical expanders can only temporarily alleviate the patient’s condition, but do not completely solve the problem. They should be considered only as an alternative to surgery when it is impossible for some reason. The main method of treating NK failure is surgical, which will be discussed below.
Surgical treatment of nasal valve dysfunction
Surgical treatment methods depend on the location of the obstruction area - external or internal NK. Correction of the external nasal valve is less of a problem.
A generally accepted method of strengthening a weakened nasal wing is the introduction of autocartilaginous strips, most often called batton grafts. As a rule, surgeons use access from an incision inside the nostril in the projection of the problem area, or a marginal incision [6, 7].
According to R. Troell et al. [8], the use of short (not touching the edge of the pyriform foramen) slatted grafts improves nasal breathing in 85% of patients, and long ones (extending beyond the edge of the piriform opening) - in 94%.
G. Nolst Trenite [9] recognized the installation of “rack” grafts as a simple and reliable method for correcting respiratory failure at the level of the nasal vestibule.
An alternative technique for reinforcing the nasal wing with a strengthening graft from an external incision in the area of the supraala sulcus was proposed by A. Deroee et al. [10]. The authors, having treated 12 patients in this way, obtained results identical to the classical technique, but note the simplicity of the operation. We believe that it is not entirely correct to make external incisions on the face, simplifying an already simple technique.
Other methods are used less frequently. Thus, C. Woodhead [11] mentioned excision of the lower part of the medial crura of the alar cartilages during septoplasty to expand the external NK. According to J. Gunter et al. [7], external valve weakness usually occurs when narrow nostrils are combined with a hyperprojection of the nasal tip. In this situation, surgical correction involves drooping of the tip of the nose, after which the nostrils take on a more oval shape. In addition, to increase the rigidity of the wing, it is recommended to introduce reinforcing grafts into the area of the alar groove.
Among the surgical interventions that eliminate the insufficiency of the external NK are also called repositioning the lateral legs of the alar cartilages and deploying a flap from the lateral cartilages. The surgeon’s task remains to choose an adequate method for a particular case [5, 7, 12].
In general, strengthening the nasal ala at the level of the external valve is not a serious surgical problem, unlike correcting the insufficiency of the internal nasal valve.
M. Constantian convincingly demonstrates the need for surgical correction of NK, presenting in the monograph “Rhinoplasty: craft and magic” [12] the results of an examination of 600 (!) patients who underwent various rhinological interventions. According to the author, correction of the nasal septum does not lead to a statistically significant improvement in nasal breathing compared to preoperative. Strengthening the external NK has a slightly more noticeable effect on nasal breathing. A significant improvement in nasal breathing is manifested only with correction of the internal NK, and the greatest effect is obtained with a combination of septoplasty, expansion of the internal valve and strengthening of the wings of the nose. In these patients, there was an increase in volumetric flow by an average of 4 (!) times in the group.
According to R. Andre et al. [13], among the large number of operations proposed to correct NK function, the most common among surgeons is the installation of so-called “spreader grafts” between the upper edges of the triangular cartilages and the cartilage of the nasal septum. The technique was first described by J. Sheen in 1984 and was originally intended to support the cartilaginous vault of the nose when the nasal bones are too short. The author began to use this technique when removing the osteochondral hump of the nose to prevent slipping of the triangular cartilages [14]. The method is widespread among surgeons and is used both to correct aesthetic problems in the middle third of the nose and to improve nasal breathing.
N. Fuleiham [15] recognizes Sheen's expanding grafts as the best method for increasing the NK angle. In difficult cases, he recommends supplementing them with cartilage strips installed between the edge of the pyriform opening and the back of the nose. This technique is especially indicated when the triangular cartilages are displaced posteriorly due to too aggressive lateral osteotomy. In addition, the author proposes to carry out preventive installation of expansion grafts during aesthetic rhinoplasty.
Several studies show the effectiveness of this method in both subjective and objective assessments [12, 13, 16]. Widening the valve angle has been shown to reduce nasal resistance [17]. The use of expansion grafts provides opportunities both to solve aesthetic problems and to improve the physiology of the NK [12].
Most authors place expansion grafts through an open approach. The advantage of this approach is the ability to accurately visualize the problem area and correctly install grafts [12].
However, the presented technique cannot eliminate the narrowing of the posterior sections of the NK, and the functional result from the use of expanding grafts is often inferior to the aesthetic one [18]. The operation does not lead to strengthening of the lateral wall of the NK and does not eliminate the dynamic component [19].
According to L. O'Halloran [20], the technique using Sheen valve angle-expanding grafts does not increase the rigidity of the movable part of the valve. In addition, the operation requires an open rhinoplasty approach. Among the disadvantages of traditional expanding grafts are R. Andre et al. [13] name the large volume of the operation, the formation of a postoperative scar on the collumella and, most importantly, the risk of disruption of the anatomy and physiology of the cartilaginous vault of the nose. The fact that the most popular technique for installing expansion grafts is the technique of cutting off triangular cartilages is especially surprising, since Sheen initially proposed a method specifically for preserving the architecture of the cartilaginous vault. Trying to eliminate the shortcomings, the authors propose installing expansion grafts endonasally, without cutting off the triangular cartilages. They provide an anatomical basis for their technique, during which high submucoperichondrial tunneling of the nasal septum is performed. The cartilage insert is installed in the area of the nasal angle valve and fixed with a suture on the back of the nose or biological glue. Using the described technique, 120 cartilage inserts were installed. The criterion for assessing effectiveness was the subjective opinion of patients. A positive result was detected in 88% of cases, and 1 patient noted worsening nasal breathing.
C. Huang et al. [21] wrote about the high morbidity of open access for installing expansion grafts. In their opinion, the endonasal technique proposed by R. Andre et al. [13], is a much less invasive procedure. At the same time, the disadvantage of this technique is poor visualization of the surgical field in a narrow area of the NK. As an alternative, the installation of expansion grafts under endoscopic control is proposed. The advantage of this method is excellent illumination and visibility of the surgical field. The operation was performed on 8 cadaveric heads, and the expanding graft was installed in one half of the nose, the other side served as a control. The study was essentially a blinded, randomized, placebo-controlled study with only a very small sample size. As a result, an objective, reliable, statistically significant improvement in NK function on the operated side was obtained. The cross-sectional area of the nasal cavity at the level of the nasal cavity increased to 0.28 cm2. At the same time, no clinical study of the effectiveness of the method has been conducted; the authors probably plan to do this later.
RP Gruber et al. [22] proposed the method of expansion flaps, the principle of which is similar to Sheen’s expansion grafts. In this case, the severed dorsal edges of the lateral cartilages curl inward, widening the angle of the nasal valve. The technique is applicable only when there is excess height of the triangular cartilages after lowering the profile of the cartilaginous dorsum of the nose and has disadvantages characteristic of the use of expanding grafts. S. Rizvi and M. Gauthier [23] believe that expansion grafts are useless without expansion sutures. Another disadvantage is the need to harvest cartilage and, as a result, additional intervention.
E. Tastan et al. [24] argued that the effectiveness of expansion grafts is limited by the width of the septal cartilage used to construct them. The authors proposed installing an autograft cut from the nasal septum in the shape of the letter H into the NK area. After cutting off the triangular cartilages from the septum, the liner is installed perpendicular to the septum, expanding the back and the angle of the valve. In 19 patients, the authors obtained a significant positive result on the subjective scale. However, it is difficult to imagine that such a significant expansion of the middle third of the external nose does not lead to aesthetic deterioration.
Widening the valve angle, which is the goal of most surgeons, does not correct the collapse of the lateral wall of the nasal cavity, so the results of operations are often disappointing [20, 25]. It is clear that surgeons are forced to look for alternative ways to correct NK.
One of them is the method of expanding the valve using a “splay” graft according to B. Guyuron et al. [18]. The technique is implemented by introducing an elastic, springy fragment of cartilage under triangular cartilages cut off from the septum. The method improves nasal breathing, but may widen the bridge of the nose too much. Even the authors, paying attention to its functional effectiveness, acknowledge the possible negative cosmetic result [18]. A. Islam et al. [26] tried to improve the operation by installing a “splay graft” endonasally.
The butterfly graft proposed by J. Clark and T. Cook [27] has a similar shape, which is inserted on top of the triangular cartilages, which is technically simpler. This technique also results in excessive expansion of the supratip region, compromising the aesthetic outcome. In addition, the shape and size of the “butterfly cartilage” do not allow expansion of the proximal nasal valve [28].
C. Sen and D. Iscen [29] developed the idea of “butterfly cartilage” and proposed a so-called “spring” graft from the resected cephalic part of the wing cartilage. The base of the insert was placed on the caudal edge of the septum, and its “wings” were immersed under the cut triangular cartilages. By unbending, elastic cartilage expands the angle of the NK. The authors talk about the effectiveness of the method, without, however, providing statistical calculations. The use of this technique is possible only during aesthetic rhinoplasty with resection of the alar cartilages. S. Rizvi and M. Gauthier [23] also fear expansion of the dorsum when using this method and indicate the need for additional cartilage harvesting.
Another popular method for correcting the collapse of triangular cartilages is the introduction of strengthening cartilage grafts (batten graft) into the weakened area, by analogy with plastic surgery of the external NK [8, 15]. Such transplants were actively used by D. Toriumi et al. [19], considering them useful for dynamic valve collapse, but not for expanding its angle.
L. O'Halloran [20] believed that the technique of strengthening the nasal wing with cartilaginous strips, described by D. Toriumi et al. [19] and R. Troell et al. [8], is theoretically correct and minimally invasive. At the same time, the cartilaginous strips make the wing of the nose heavier and thicker, which can lead to a deterioration in the function of the nasal cavity.
The disadvantage of using slatted grafts is their influence on the shape of the external nose and projection in the form of small elevations. A. Belousov [6], after 80 operations using long slatted grafts in 62 (77.5%) patients, noted their visualization during external examination. A third of the patients developed asymmetry of the contours of the suprawing zones.
A group of methods for expanding the nasal valve using sutures deserves attention. For the first time, the technique of suture support or “suspension” of the nasal valve was proposed by R. Paniello [30]. The essence of the operation is to suture a fragment of the upper triangular cartilages and pull it upward and laterally with fixation to the edge of the orbit. The valve expands as in the Cottle test. The thread is passed subcutaneously, and the lateral cartilage and orbital margin are accessed through separate microincisions. The operation reduces the resistance of the nasal cavity [2, 30]. According to L. O'Halloran [20], R. Paniello's technique [30] is logical and allows to move the lateral wall of the nasal cavity away from the septum, but is associated with the risk of damage to the eye, lacrimal ducts and infraorbital nerve.
M. Friedman et al. [2], recognizing that the described technique leads to an improvement in NK function in some patients, draw attention to its complexity, significant time investment and long healing time. The authors were technically unable to perform an alternative version of the R. Paniello technique [30] with fixation of the tension thread to the orbital periosteum.
Taking into account the described shortcomings, M. Fridman et al. [2] proposed a modified NC suture support method. The stages of the operation include percutaneous or transconjunctival exposure of the orbital edge and the placement of a burr hole in it for a “bone anchor”. A thread is fixed to the anchor, the ends of which are passed under the skin into the NK area, capturing the caudal edge of the triangular and cephalic edge of the alar cartilage. When the thread is tightened, the NK expands due to upward and lateral displacement. Most of the 86 patients experienced subjective improvement in nasal breathing. At the same time, in 5 patients the problem persisted and in 2 patients reoperation was required. In one observation, a subcutaneous abscess developed. In our opinion, additional intervention in the orbit and additional equipment (drill, bone “anchor”) complicate the method. In addition, the authors note that almost all patients experienced changes in the shape of the nose.
S. Rizvi and M. Gauthier [23] tried to further simplify the method of R. Paniello [30]. Speaking about the ineffectiveness or invasiveness of most previously described methods of NK correction, they proposed their own version of suture valve tension. The suture, involving the caudal edge of the triangular cartilage, was carried out under the skin with a flap not in the area of the orbital edge, as in R. Paniello [30] or M. Fridman et al. [2], and into a small transverse incision of the skin of the nose, made below and anterior to the medial canthus. When tying, the valve was pulled back, and the knot was immersed in the wound.
At the same time, C. Hurbis [31] provides data on ambiguous long-term results with this method of NK correction. Later, R. Andre and H. Vuyk [32] presented their negative experience with the use of suture expansion of NK. In 21% of cases there was no improvement in nasal breathing, in 52% the improvement was insignificant. In 25% of cases, the development of suborbital edema was noted, which required revision in 3 patients. The authors strongly do not recommend this technique for the treatment of NK failure.
Another well-known technique for expanding the NC using sutures is the technique developed by S. Park [33]. The idea is to pass the thread across the triangular cartilage of one side and pass through the dorsum to the opposite side. The operation is performed from open access. Tightening the suture causes the middle portion of the lateral cartilages to rise upward. The method complements expanding grafts, is quite invasive and does not have serious independent significance. The capabilities of the method are limited by the tight connection of the upper triangular cartilages with the nasal bones, which prevents their lateral displacement [20].
Competing with suture retraction methods are various options for expanding the valve due to plastic surgery with local tissues when stretching or moving nasal wing flaps. Thus, C. Woodhead [11] developed a method for correcting NK, which consists of removing part of the edge of the pyriform opening with plastic surgery using a Z-shaped mucocutaneous flap. The author does not provide convincing data indicating the effectiveness of the method.
Following his theory of the development of valve problems, L. O'Halloran [20] developed a method of surgical correction of NK insufficiency by tightening a skin-cartilaginous flap shaped like the letter J. An incision in the skin of the nasal vestibule was made along the caudal edge of the alar cartilage, which was then turned posteriorly . Wing cartilage was isolated in the subperichondrial layer. The resulting cartilage-cutaneous flap, including the lateral crus of the alar cartilage and skin, was pulled forward and downward. Excess tissue along the edges of the flap was excised with two strips, after which the wound was sutured. As a result, tension and strengthening of the lateral wall of the nasal cavity occurred. The effectiveness of the method was 89% with a follow-up period of 257 days. When familiarizing yourself with the surgical technique, it is confusing that the displacement of the tissue forward and downward could potentially narrow the angle of the valve, whose role in nasal breathing is considered proven.
J. Dutton and M. Neidich [34] used a technique for correcting NK using Z-plasty. Only 12 patients were operated on, and in 11 of them a satisfactory functional result was obtained. The authors conclude that the method is safe, effective and relatively non-invasive.
E. Kern [35] wrote that a significant and main drawback of all techniques aimed at increasing the angle of the nasal cavity is the postoperative expansion of the cartilaginous portion of the dorsum and tip of the nose. As an alternative, the author proposes the method of M-plasty of the NK, which can be performed in one stage with plastic surgery of the external nose and septoplasty. The results of acoustic rhinometry showed the effectiveness of the proposed technique.
An interesting option for internal NK plastic surgery using local cartilaginous and soft tissues was proposed by G. Nolst Trenite [9]. A Z-shaped incision is made inside the nasal vestibule and a mucocartilaginous flap is cut out, including a cephalic fragment of the alar cartilage. At the same time, the triangular cartilage is cut away from the dorsal edge of the septum. Next, a counter movement of the flap occurs [36] and a wedge-shaped fragment is installed between the severed alar cartilage and the septum. The main problem, in our opinion, is fixation of the displaced flap. The author suggests doing this with one thread drawn through the tissue to the back of the nose. The unreliability of such fixation is obvious and, as a result, there is a high risk of displacement of the valve-expanding flap.
An indirect method for correcting NK is taking into account the biomechanics of the valve when performing aesthetic rhinoplasty. If aesthetic surgery to reduce the length and projection of the nose is performed physiologically correctly, then one can expect improvement in nasal breathing due to the fact that the valve becomes “more oval” and its angle expands [11].
It is obvious that despite the many proposed techniques for correcting NK, there is no sufficiently effective method that would equally successfully solve both the functional and aesthetic aspects of the problem [20]. Without counting on the reliability of any one method of NK plastic surgery, some surgeons try to combine various techniques.
N. Fuleiham [15] recommends using batten grafts to improve the function of the external NA and combining them with other types of grafts that widen and strengthen the nasal ala. If there is deviation of the dorsal edge of the nasal septum cartilage, which is the cause of valve insufficiency, the author recommends septoplasty. However, he believes that due to the memory of the shape of the nasal septum, simply releasing the cartilage will lead to a relapse of the disease. To solve the problem, it is recommended to use two strut grafts that straighten the nasal septum.
R. Schlosser and S. Park [16], realizing the inconsistency of existing publications on the results of surgical correction of NK, conducted their own study on 6 cadaveric heads and 34 patients. A comparative assessment of the effectiveness of expansion grafts using the original Sheen technique and valve expansion using sutures (flaring suture), proposed by S. Park in 1999, was carried out [33]. The result revealed the low effectiveness of both methods. Expansion grafts increased the cross-section by only 5.4% (p>0.5), suture expansion - by 9.1% (p>0.5), and only a combination of these methods made it possible to obtain a statistically significant improvement (18.7% , p<0.5).
J. Gunter et al. [7] to eliminate problems of internal NK, expanding and strengthening grafts are used together. S. Rizvi and M. Gauthier [23] believe that expansion grafts will be effective only when combined with the application of expansion sutures.
For age-related, postoperative or traumatic stenoses of the internal valve, A. Belousov [6] recommends surgical intervention, which he calls “valvuloplasty”. The operation is performed through an open approach with exposure of the nasal valve area. The surgeon then evaluates the problem and corrects it using slatted autografts or expansion grafts. Essentially, the intervention comes down to a combination of these two traditional methods.
The methods of surgical correction of NK using various biocompatible allogeneic materials stand apart. Thus, CG Hurbis [31] used a “butterfly”-shaped expanding implant made of polytetrafluoroethylene to correct NK failure. S. Rizvi and M. Gauthier [23] actively criticize this technique, drawing attention to the short period of postoperative observation (4 weeks) and the possibility of deformation of the titanium prosthesis after surgery, which has to be readapted directly through the soft tissue.
Trying to immediately influence two links in the pathogenesis of NK failure, M. Mendelsohn and K. Golchin [37] developed a technique for “expansion and reinforcement” of NK using sutures and porous ethylene. D. a'Wengen and U. Steinhart [38] are trying to popularize the technique of expanding the NK with “breathing implants” (breathe implant). The implants are a titanium structure that is installed on top of triangular cartilages and fixed to them with sutures. Obvious disadvantages of both methods include the need for open access and implantation of allogeneic materials.
The technique of radiofrequency thermotherapy of NK, proposed by E. Seren [39], does not fit into any of the listed groups of methods. The essence of the method is radiofrequency exposure to soft tissue in the area of the inner surface of the triangular cartilages and the edge of the pyriform opening. According to the authors, scarring in the submucosal layer should lead to a decrease in tissue volume, similar to a decrease in the size of the inferior turbinates during their radiofrequency reduction. The authors call the advantage of the method its non-invasiveness, however, the first surgical steps are an intranasal incision and isolation of the lateral crus of the alar cartilage, apparently to avoid its damage by the radio wave. This stage of the operation negates all attempts to create a minimally invasive outpatient technique. In addition, as S. Rizvi and M. Gauthier rightly note [23], the article does not contain long-term results of using the method; The only illustration shows severe postoperative asymmetry of the nostrils, and the possibility of uncontrolled scarring is not taken into account.
Thus, the complexity of methods for restoring NK function, as well as the variability of their results, lead to the fact that the problem remains. Articles devoted to the problem of NK mainly contain endless descriptions of new surgical techniques without adequate assessment of the results. There were no controlled studies among the published studies, and only one article met level IIIb evidence [40].
Obviously, further search for reliable and adequate methods of diagnosis and correction of NK is required, taking into account the individual clinical and anatomical features of each case, as well as well-organized comparative studies that take into account all the requirements of modern evidence-based medicine with reliable statistical processing of the results.
TURBINOPLASTY
In the 1980s, the term “turbinoplasty” was coined (Mabry, 1982, 1984). It combines various intraturbinal methods of surgical reduction of the inferior turbinate while preserving the mucous membrane. Recently, a number of authors have developed and disseminated techniques for intraturbinal reduction of the inferior turbinate (Gray, 1965; Lenders and Pirsig, 1990; Grymer et al., 1993; King and Mabry, 1993; Illum, 1997; and Marks, 1997; Huizing, 1998). After displacing the concha medially, an L-shaped incision is made on its inferolateral edge. The mucosal flap is raised and a portion of the bone and parenchyma is resected as needed. Then the mucous flap is placed in place and fixed.
Figure 5. Anterior turbinoplasty technique according to Pirsig and Huizing (from the textbook Huizing and De Groot, 2001)
a. Medialization and L-shaped incision of the head of the nasal concha with a Beaver knife No. 64; b. Separating a flap of the mucous membrane and resection of part of the bone and adjacent parenchyma of the inferior turbinate; c. Placement and fixation of the mucosal flap and lateralization of the reduced inferior turbinate.
When the resection of bone and parenchyma is limited to the anterior part of the concha, we speak of an “anterior turbinoplasty.” This technique is used in patients with inspiratory respiratory obstruction due to hyperplasia of the head of the concha. Another technique is “partial lower turbinoplasty.” This technique involves making two separate incisions that connect at the center of the shell. The wedge-shaped part of the shell is then removed and the edges of the resulting defect are joined together (Schmelzer et al. 1999). Intraturbinal turbinoplasty allows for size reduction while preserving all mucosal functions, as recently demonstrated by Passali et al. (1999) in a comparative study. Its second advantage is the low likelihood of postoperative bleeding and crusting. From the point of view of “optimal amount of reduction while preserving function,” intraturbinate turbinoplasty is the method of choice for the treatment of turbinate hypertrophy. This is a tissue-reducing procedure, but it can be modified according to pathology without regard to mucosal function.
LASER SURGERY
Lenz in 1977 was the first to report the use of laser technology for reduction of the inferior turbinate, using an argon laser (Lenz et al., 1977; Lenz, 1985). Subsequently, other types of lasers were used: CO2 laser (Mittelman, 1982; Simpson et al., 1982; Fukutake et al., 1986, Kawamura et al., 1993; Kubota, 1995; Lippert and Werner, 1997; Lagerholm et al., 1999; Papadakis et al., 1999; Katz et al., 2000); potassium titanium phosphate (KTP) laser (Levine, 1989, 1991); neodymium-YAG laser (Werner and Rudert, 1992); diode laser (Min et al., 1996); and holmium-YAG laser (Serrano et al., 1998).
The laser produces a beam of coherent light that is absorbed by tissue; the degree of absorption depends on the wavelength. At the same time, its energy leads to evaporation of the tissue. The depth of the resulting damage thus depends on the wavelength, the degree of tissue absorption and the amount of energy applied. Its diameter depends on the size of the laser beam spot. Therefore, laser technology can be used for various purposes depending on the parameters applied. One of the parameters is the operating mode, either continuous or pulsed. Most authors use pulsed mode, since a continuous laser beam can cause damage to a large area. A series of spots or small craters are created on the mucous membrane at a distance of 1-2 mm (Figure 6). Laser energy can be supplied directly (CO2 laser) or through optical fiber (KTP, Nd-YAG, Diode, Ho-YAG). Some authors prefer to make linear cuts as with electrocautery. Continuous radiation expands the thermal damage zone. The laser can also be used to remove tissue during partial (or total) conchotomy or intraturbinal tissue reduction. Thus, laser technology can be used to perform partial conchotomy and intraturbinal tissue reduction. The laser can be used in cases where a knife or scissors would normally be used. We emphasize that laser surgery is not a new operation, but a new type of equipment for performing the operation.
Figure 6. Laser treatment of the inferior turbinate (after Werner and Lippert, Rhinology 35: 33-36, 1997)
Microscopic studies of the mucosa after laser exposure have revealed limited regeneration of the ciliated epithelium, while the number of seromucous glands and cavernous plexuses gradually decreases (Kubota, 1995; Elwany and Abdel-Moneim, 1997). Another study found significant degeneration of the superficial submucosal layer and its replacement by granulation tissue, with scar tissue visible after a year (Fukuta et al., 1986).
Laser turbinate surgery can be performed under local anesthesia on an outpatient basis. The hemostatic properties of laser exposure are such that postoperative bleeding is very rare and nasal tamponade is not necessary. However, temporary crusting is common, and synechiae may also occur.
Published results of turbinate laser surgery vary widely (from “43% success” to “excellent results”). However, almost all studies are retrospective and non-comparative. Therefore, they are of little value and are not considered here. We are aware of only one prospective comparative study that compared the results of different types of laser surgery. This study did not find significant differences (DeRowe et al., 1998).
Laser surgery for conchae does not meet the requirement of “optimal amount of reduction combined with preservation of function.” With limited evaporation of the mucous membrane and submucosal layer, the volume of reduction is clearly insufficient. If the volume removed is sufficient, then the functional changes are severe and irreversible. Therefore, laser surgery is not compatible with the modern concept of functional nasal surgery and should not be used to treat hypertrophied inferior turbinates.
ELECTRICAL TOOLS
Recently, electric instruments for turbinate surgery such as “shavers” have come into use (Setcliff and Parsons, 1994). These instruments are used both on the conchal surface and intraturbinally, often in combination with endoscopic guidance. They are claimed to allow precise removal of soft tissue. Some surgeons cut away portions of the shell from the lateral and inferior margins, while others work with a shaver inside the shell (Friedman et al., 1999; Van Delden et al., 1999). This technology is said to be fast, effective, well tolerated and low in pain (Davis and Nishioka, 1996).
The use of power tools is determined by personal preferences. It depends little on the type of instrument. This is more of a surgical technique than a measure of the amount of turbinate reduction.