Article for the “Bio/Mol/Text” competition: Acne, or in common parlance pimples, is estimated to affect 70% of people and almost 85% of teenagers. Acne is a complex, multifactorial disease, and we became interested in the role of microorganisms that live on the skin. It is known that the skin of an unborn child is sterile, but soon after birth it is colonized by a variety of environmental microorganisms. They form the microbiome of our external integuments. We decided to take a closer look at whether bacteria and skin get along, what relationships are formed between bacteria - and how genetics and environment influence this.
Competition “Bio/Mol/Text”-2021/2022
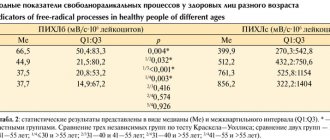
This work was published in the “School” category of the “Bio/Mol/Text” competition - 2021/2022.
The nomination partner is the non-profit boarding school “Letovo”.
The general partner of the competition is the international innovative biotechnology company BIOCAD.
The general partner of the competition is: the largest supplier of equipment, reagents and consumables for biological research and production.
"Book" sponsor of the competition - "Alpina Non-Fiction"
Skin structure
Human skin consists of three layers (Fig. 1).
The hypodermis, or subcutaneous fat, is the deepest layer. This is the main store of fat in the body.
The dermis (or skin itself) is located between the epidermis and hypodermis. It is a connective tissue with numerous collagen and elastin fibers. It largely determines the condition of the skin - hydration and elasticity.
The dermis is in contact with the basal layer, which gives rise to the upper layer, the epidermis. The main cells of the epidermis are keratinocytes. As they grow, they move upward from the basement membrane, releasing lipids. There are several layers of keratinocytes, depending on the age and condition of the cells, which are replaced in about a month [1].
We have not yet mentioned epidermal derivatives. Sebaceous, sweat, sulfur and mammary glands, hair have the same origin. The sebaceous glands secrete sebum (sebum), which microorganisms happily feed on.
The skin is a separate ecological niche in which complex microbial communities are formed. The set of microorganisms inhabiting the skin, or microbiome, is a dynamic system with its own patterns. Here, as in any ecosystem, there are different connections between organisms. Microorganisms also interact with the environment, which largely dictates the conditions of their existence [2].
Figure 1A. Skin structure.
Figure 1B. The structure of the epidermis.
author's drawing
Figure 1B. The structure of the sebaceous gland.
Now let's talk about the skin barrier. This is a system of various lipids and keratinocytes that protects the skin from dehydration and mechanical damage. But within the framework of the article, we are interested in the fact that the skin barrier is needed to prevent the effects of bacteria and pathogens on the vital activity of skin cells [3].
The skin barrier is usually divided into two components - the hydrolipid mantle and the lipid-epidermal barrier (Fig. 2). The main functional feature of the hydrolipid mantle, consisting mainly of secretions of the sebaceous and sweat glands, is an acidic environment, pH approximately from 4.7 to 5.7. Thanks to it, harmful bacteria stop multiplying and die. The lipid-epidermal barrier consists of many dead cells held together by lipids, which they gradually released into the external environment as they grew older. It is this that protects the skin from dehydration, reducing transepidermal water loss (TEWL), and is also the second link of protection after the hydrolipid mantle from the penetration of bacteria and allergens into the skin.
However, we should not assume that the skin barrier completely protects us from pathogens. Research still revealed the presence of bacteria in the dermis and hypodermis [4].
Figure 2. The skin barrier does not completely protect the skin from bacterial penetration. As keratinocytes grow, they secrete numerous sheets containing lipids (keratinosomes). Thanks to intercellular ligaments - corneodesmosomes - and lipids, corneocytes, that is, dead cells of the stratum corneum of the epidermis, are attached to each other, forming an integral structure, and are moisturized by NMF - a natural moisturizing factor. These are molecules that help retain more water in the epidermis: free amino acids, urea, lactates, etc.
website
Composition and functions of sebum
Sebum composition is a mixture of various lipids (fats). The composition may vary depending on gender, age, genetics and diseases.
Includes:
- saturated fatty acids - palmitic, stearic, oleic;
- squalene;
- sapienate and seboleate (unique fatty acids that are found only in sebum);
- unsaturated fatty acids - formic, acetic, propionic and others;
- glycerol;
- cholesterol;
- wax ether;
- phospholipids;
- metabolic products.
Check whether you are properly caring for oily, problematic skin.
Functions of sebum
Sebum has a number of functions for the skin, the main one of which is protective. That is why, when exposed to the sun, climate change, improper care or aggressive procedures, the skin begins to secrete even more sebaceous secretion for protection.
- Barrier – protecting the skin from external aggressive factors such as ultraviolet rays, pollution, dust and even microtrauma. By forming a sebaceous film, the skin builds a protective barrier to preserve deeper structures.
- Excretory - a number of drugs, toxins and skin metabolic products are excreted through the sebaceous glands by secreting sebum.
- Prevention of dehydration – the oily film on the skin prevents excess moisture evaporation with subsequent dehydration of the skin.
- Bactericidal - the unsaturated fatty acids included in the composition prevent the proliferation of pathogenic microflora and the development of inflammation, supporting the skin microbiome.
- Antioxidant – squalene contained in the composition neutralizes the effects of free radicals.
Pathogenesis of acne
The main mechanism of acne is an increase in sebum production and the number of differentiating keratinocytes under the influence of androgens. As a result, the pores become clogged, an anaerobic environment occurs, and aggressive strains of P. acnes begin to actively multiply. Sooner or later our body notices this, complex inflammatory mechanisms are launched, and acne occurs [5].
But not everything is so simple: acne, as already mentioned, is a multifactorial disease, and there are quite a few factors that can trigger it:
- Genetic features. There are several hereditary forms of acne. For example, those associated with the AR gene (androgen receptor). Sometimes acne is not due to excess androgens, but to hypersensitivity of the androgen receptors.
- Neuroendocrine disorders.
- Nutrition.
- Excess iodine and bromine, vitamin B12[5].
- Some drugs and chemicals (about 210 known).
- Use of broad-spectrum antibiotics. (Previously, acne could be treated this way). They acted against bacteria, but not against fungi of the genus Malassezia, the secretions of which also irritate the sebaceous glands [5].
- Smoking.
- Stress [5]. Although often the very fact of having acne and the inability to get rid of it is stressful.
- Photodamage.
- Incorrectly selected cosmetics.
How can care affect skin condition?
The surface of healthy skin has a slightly acidic environment. Under the influence of cosmetics, the pH changes, which changes the living conditions of the microflora, and can also disrupt the epidermal barrier.
A significant part of cleansers alkalize the surface of the skin. The lipids in the skin barrier are simply washed away. You can use an acidic tonic to minimize changes. But not everyone knows about this, and not all tonics have the appropriate pH. With an intact epidermal barrier, the skin can restore balance in a couple of hours, and a single exposure does not cause much harm.
There are also means that are harsher in relation to the microbiome. For example, chemical peels are a popular cosmetic procedure. Its essence comes down to the fact that the top layer of epidermal cells is removed, and the skin becomes smoother. However, along with these cells, many bacteria also leave, which reduces their species diversity. And diversity is often a sign of a good microbiome. Peeling also excessively lowers the pH of the skin.
Why is this important to know?
Many mass-produced cosmetics aimed at treating acne can, on the contrary, harm your skin. Therefore, it is important to carefully select cosmetics for home use [6]. Indeed, with systematic violation of the integrity of the epidermal barrier, the skin becomes more vulnerable to various external influences, and transepidermal moisture loss increases. This has a bad effect on both appearance and health.
Figure 3. Distribution of bacterial families on human skin. In the table below, the names of bacterial families are indicated under different colors; they correspond to the colors in the diagrams on the main diagram. Next to the diagrams are multi-colored dots: blue are areas with increased sebum production, green are wet, red are dry.
[7]
How to reduce sebum production
What steps can you take on your own in caring for oily skin in order to reduce the amount of sebum produced and not provoke its excess release?
Do not sunbathe and use SPF cream
Exposure to direct sunlight activates the sebaceous glands, because... the skin is protected from their aggressive effects.
It is imperative to use a cream with SPF, the main thing is that the protection factor is physical and not chemical.
- Chemical photo filters convert the energy of UV rays into heat, which has a detrimental effect on the functioning of the sebaceous glands.
- Physical photo filters simply reflect UV rays without causing an increase in skin greasiness.
CBD “Blue Light” face cream SPF 30 is a cream with a natural composition. Contains zinc oxide - a physical photo filter, creates a complete screen for the skin, and has an anti-inflammatory effect. Cannabidiol, the newest ingredient and the basis of the CBD line, soothes, restores the skin and normalizes the functioning of the sebaceous glands.
Do not overdry the skin
The use of aggressive cosmetics and procedures increases the risk of dehydration, which means a response from the sebaceous glands in the form of hyperproduction of sebum.
Daily use of cleansers with high percentages of acids, peelings with AHAs that activate the sebaceous glands, tonics with alcohol are enemies for skin with increased sebum production.
Regular skin moisturizing
Moisturizers are needed to avoid skin dehydration and compensatory release of sebum. Use moisturizers based on hydrants (substances that attract water), such as hyaluronic acid.
Serum B5 moisturizing mattifying for oily skin DermaQuest is a unique gel serum designed specifically for skin with an oily sheen. Micronized hyaluronic acid moisturizes and restores the skin, while Lilac Stem Cells and sebum regulators normalize sebum production.
The result is instantly hydrated and matte skin!
Skin cleansing
The importance of this stage for shiny skin is difficult to overestimate. There are two types of cleansing for oily skin: daily and deep.
The sebaceous glands are most active at night. Do not ignore morning cleansing of the skin using a delicate cleanser.
For daily cleansing, use specialized products that effectively and at the same time gently cleanse the skin.
Cleansing gel "DermaKlia" with DermaQuest enzymes is a soft, slightly foaming gel, created specifically for daily washing of oily skin.
Deep cleansing is carried out 1-2 times a week to completely cleanse pores and remove skin hyperkeratosis.
Example: Pumpkin mask DermaQuest
Skin microbiome
Map. Who lives where
Let's look at the most common microorganisms and their habitats on the skin. Those of them who live in the same place on the body have the greatest influence on each other.
P. acnes and P. granulosum are found in areas rich in sebaceous glands. P. acnes predominates on the scalp, forehead, ears, back and sides of the nose. It is the main colonizer of the sebaceous glands.
Moist areas such as the navel or armpit mainly contain Staphylococcus and Corynebacteria species. The axillary region is populated by gram-positive bacteria of the genera Staphylococcus, Micrococcus, Corynebacterium, as well as some Propionibacterium (Fig. 3) [7].
Drier areas are predominantly inhabited by Staphylococcus, Micrococcus, Corynebacterium, Enhydrobacter and Streptococcus
Perhaps the name P. acnes we mentioned earlier made you think that it is these bacteria that cause acne.
First of all, it should be remembered that acne is a complex and multifactorial disease that cannot depend on one bacterium. Some studies even show that healthy skin follicles provide a habitat that allows only P. acnes to colonize, while Staphylococcus epidermidis and other species have been found in acne patients. Therefore, the role of P. acnes is quite ambiguous, and there is even a possibility that P. acnes does not cause acne, but, on the contrary, protects against it [8].
The opinion that the skin is a habitat only for bacteria is wrong. In fact, the microbiome of our integuments is much more diverse and includes various types of protists, fungi, and sometimes even animals like Arthropods! Below you can see the demodex skin mite, a typical inhabitant of human skin that feeds mainly on sebum. This comrade itself is harmless, but its excessive reproduction in some people can cause an allergic reaction, manifested in the form of an acne-like condition (small pimples).
Video 1. This is a skin mite. Every person has at least one species.
How to reduce oily skin
It is necessary to understand that the main cause of oiliness is excess sebum production. It can be reduced or increased, in the second option an unpleasant oily sheen appears, seborrhea and acne are likely to develop, pores become clogged, the skin does not breathe, comedones appear and the skin is more susceptible to external influences.
Let's look at several ways to reduce sebum production.
Care products
Products should be designed for oily skin, they should be gentle so as not to cause more damage. Particular attention should be paid to cleansing products; they should not dry out or cause irritation. It is advisable to wash your face with water at soft room temperature, do not remove rashes using mechanical methods, and use products that do not clog pores.
Diet
Nutrition, like nothing else, helps reduce oily skin. It is on this that the flaws in a person’s diet are reflected.
You should limit fast carbohydrates and saturate your diet with fiber (fruits and lots of vegetables), you must follow a drinking regime (consume enough water depending on your weight). It is better to prepare food yourself to avoid introducing dangerous additives into the body, or carefully study the ingredients before purchasing. The diet can be simple but balanced.
Additional procedures
Without a specialist, it is better not to resort to home procedures; they can cause more damage than is already present.
As an aid, you can do massages to relieve swelling and improve blood circulation; this helps improve the “breathing” of the skin, which is very important for oily people. Darsonvalization (microcurrents), the use of light bactericidal agents, and facial cleansing by a qualified cosmetologist are suitable.
How bacteria adapted to live on the skin
The skin microbiome is formed under the influence of a wide variety of variables: age, skin pigmentation, environmental factors (sun rays, cosmetics that we constantly use) [7], [9], [10].
We have already looked at the distribution of species on the surface, let’s dig deeper. It was revealed that the lower part of the stratum lucidum of the epidermis (Fig. 1) has an alkaline reaction, the middle part has a neutral reaction, and already dead cells have an acidic reaction [1]. Thus, environmental conditions depend not only on the location on the body, but also on the depth at which bacteria colonize the skin.
All organisms strive to increase their numbers, and bacteria are no exception. Here are some of the successful strategies they developed:
- Variable proteins. Bacteria of the same species are different from each other, and the immune system is less able to recognize and deal with them.
- Proteins that provide attachment to the epithelium. The better the bacteria attach to the epidermis, the more this species will be present [11].
- Substances that prevent competitors from living: antibiotics, SCFAs (short-chain fatty acids), and so on [12].
- Substances that act against other strains of the same species [13].
A number of SCFAs are naturally produced by skin cells, as well as by beneficial bacteria, which have also learned to break down fatty acids into shorter fragments. Such bacteria help the skin perform its protective function, since SCFAs slow down the development of random microorganisms (beneficial bacteria mostly need this ability in order to take root on the skin). In our case, P. acnes ferment glycerol to various SCFAs, including propionic acid [12].
Do bacteria and our immunity get along?
Bacteria can activate various signaling pathways in human skin cells (Fig. 4).
Figure 4. The effect of microorganisms can be positive, negative or neutral. The relationship between bacteria and skin is exemplified by the skin's innate ability to detect microorganisms through Toll-like receptors (TLRs). Other types of interactions are shown in the figure: at the top - the influence of ordinary skin bacteria, at the bottom - pathogenic. On a colored background - descriptions of molecules. The scheme is quite conventional and there are much more real interactions. And they are more complicated.
author's drawing
Bacteria are able to influence the innate immune response of keratinocytes, making them more or less reactive [14].
Are the microbiome and acne connected?
We have already understood that various bacteria live on the skin, which can be both beneficial and pathogenic. Now we should consider their connection with acne.
So, bacteria and fungi colonize the skin because it is a convenient habitat for them, since it has a suitable food source - for example, some kind of epidermal lipids. And here we come to an extremely interesting moment. This lipid is released to the surface from the cell under the control of genes. In conclusion: what is the true cause of acne - a pathogenic bacterium or genes? The influence of genes or environment (i.e., the established microbiome)?
Is R. acnes good or bad for health?
We previously mentioned P. acnes and promised to look into it in more detail. In this part of the article we will talk about beneficial and harmful traits, various interactions of this bacterium, as well as the possibility of determining it on yourself.
Useful features
P. acnes shares properties with dairy propionibacteria, which are considered harmless - and even beneficial [12]. Organisms like it have many positive properties: synthesis of vitamin B12, riboflavin, folic acid. P. acnes is also able to regulate the number of other bacteria by producing SCFAs (short chain fatty acids). Fermentation of glycerol by P. acnes and S. epidermidis can inhibit the growth of the most common skin pathogen, Staphylococcus aureus. This prevents the dangerous bacterium from colonizing skin wounds [15].
Opportunistic traits
The pathogenesis of acne is the mechanism of disease development in which P. acnes plays a significant role. It secretes enzymes that destroy human tissue components and can aggravate a number of other diseases [16], [17].
A clogged sebaceous gland creates an anaerobic environment. It is beneficial to P. acnes and promotes overgrowth. But during the development of acne, not only this bacterium was found there, but also other microorganisms, including S. epidermis. That is, more than just P. acnes is involved in the process.
The relationships between bacteria are ambiguous. S. epidermidis breaks down fatty acids into shorter SCFAs. It turns out that it can curb the excessive growth of P. acnes and indirectly improve the situation with acne [18]. Although not so long ago we talked about how S. epidermidis and P. acnes together “protect” us from Staphylococcus aureus (Staphylococcus aureus).
Useful products for the sebaceous glands
- Walnuts. They contain a large amount of polyunsaturated fatty acids and are an important component of the human diet. In addition, the phytoncide juglone contained in them significantly increases the bacteriostatic function of sebum.
- Chicken eggs. Due to the large amount of nutrients, eggs play an important role in providing the sebaceous glands with adequate nutrition.
- Carrot. The substances contained in carrots are responsible for maintaining the normal functioning of the sebaceous glands. This is due to the presence of provitamin A in carrots, in the form of beta-carotene.
- Fatty fish. Polyunsaturated acids contained in fish are actively involved in the process of sebum production, which plays an important antibacterial and protective function.
- Chicken meat. It is a source of protein, which plays an important role in the construction of sebaceous gland cells.
- Sea kale. Contains a large amount of iodine, which, together with the phytoncide juglone, is involved in ensuring bacteriostatics of sebum.
- Bitter dark chocolate. Stimulates the release of serotonin, which is responsible for providing the entire body, and the sebaceous glands in particular, with a normal amount of oxygen. Can only be consumed in small quantities.
- Spinach. Good source of antioxidants. Participates in maintaining the water-salt balance of sebaceous gland cells.
- Greens and leafy vegetables. An excellent source of magnesium, potassium and organic calcium. Improves the functioning of the sebaceous glands. Protects against excess sebum secretion.
- Beet. Cleanses the body of waste and toxins. Helps normalize the functioning of the sebaceous glands.
General recommendations
For the normal functioning of the body, it is important that its largest organ, called the skin, is healthy and can normally perform its protective functions. But to do this, it is necessary that the skin cells have good turgor and are protected from the effects of pathogenic microorganisms. And, as mentioned above, the sebaceous glands are responsible for this. And in order for them to fulfill their role, it is necessary to provide them not only with adequate nutrition, but also with appropriate training.
- Massage using patting movements helps very well in this case, as a result of which the blood vessels of the skin are activated, feeding the sebaceous glands.
- Also, to prevent blockage of the glands, visiting a sauna is useful (it is advisable to consult a cardiologist first).
- A contrast shower is also good, as a result of which the functioning of the sebaceous glands improves.
Products for cleansing and healing the sebaceous glands
Pharmacy mash, which contains substances such as sulfur and resorcinol, has shown good results for cleansing the sebaceous glands, as well as for preventing acne. Thanks to these components, the sebaceous passages expand, clearing dirt and sebaceous plugs. You can order such a chatterbox at pharmacies that prepare your own medicines.
Harmful products for the sebaceous glands
- Alcoholic drinks. Alcohol intake stimulates the occurrence of spasms in the excretory ducts of the sebaceous glands, as a result of which they may be completely blocked and the appearance of wen (lipomas).
- Long-term storage products. Due to the presence of high levels of preservatives in them, they also have an adverse effect on the cells of the sebaceous glands.
- Pastries and sweets. Lovers of everything floury and sweet run the risk of disrupting the normal functioning of the sebaceous glands. In this case, increased production of sebum begins, as a result of which the skin takes on an unkempt appearance, shines, and acne appears on it.
Attention! The information is for informational purposes only and is not intended to make a diagnosis or prescribe treatment. Always consult a specialized doctor!
Tatyana Eliseeva chief editor of the Food+ project
Ask a Question
Rating:
5
/10
Votes: 2
Usefulness of material 5
Reliability of information 0
Formatting of Article 5
Interactions between P. acnes and other bacteria
P. acnes and related species can produce bacteriocins (substances that cause damage to bacterial cell structures). They usually act against closely related species, but at least one of them (propionicin) inhibits even some gram-negative bacteria and fungi. In addition, P. acnes is capable of producing 2 types of thiopeptide antibiotics (high sulfur content). They strongly inhibit protein synthesis in gram-positive bacteria. And some strains of P. acnes are able to suppress other strains of their own species! [13]
Bacteriocins and bacteriocin-like substances of P. acnes may be responsible for successful competition with other microorganisms, which explains its dominant presence in healthy follicles.
Interaction between P. acnes and skin cells
How else to explain the dominance of P. acnes? She has identified 4 proteins that can trigger the body's immune response. Some of them are variable (DsA1 and DsA2). It turns out that within the same species, bacteria are slightly different, as if they are camouflaged. This is how P. acnes evades immunity.
There are TLR9 receptors inside keratinocytes that are capable of sensing bacterial DNA. When P. acnes binds to them, a very interesting thing happens: the bacterium is, as it were, turned a blind eye and can thus exist inside the cell for several weeks. After which inflammation still starts [19].
What happens to healthy skin and skin with acne?
By looking at the proteins, you can quite accurately say which “development program” the cell followed. So, in the sebaceous glands of healthy skin there are many proteins that are involved in protection against cellular stress and reactive oxygen species.
However, the sebaceous glands of people with acne have discovered proteins that are involved in tissue repair. This indicates that something has gone wrong and the tissue has been damaged. The foreign proteins identified were exclusively from P. acnes. The most common are CAMP factors (about them in the next section), as well as proteins that ensure the attachment of bacteria to the epithelium.
It would seem that everything is quite clear: P. acnes in this case behaves like an aggressor. But it was not there! It turns out that these same P. acnes proteins are also found on healthy skin. This once again confirms the controversial role of P. acnes in the development of acne [11].
Function of the sebaceous glands
Sebaceous glands are found on the skin of the entire body, except the soles and palms.
Their secretion (sebum) serves as a lubricant for hair and skin.
There are so-called “seborrheic zones”, in which the density of the sebaceous glands is much higher. These include: forehead, central part of the face, ears, scalp, interscapular region, chest, shoulders. The sebaceous glands of these areas are involved in the inflammatory process, which leads to the formation of acne.
They lie under the skin at a level of 0.5 mm, at the root of the hair, forming the so-called pilosebaceous follicle. It opens on the surface of the skin as a pore.
Over the course of life, the depth, number and size of the sebaceous glands change. In a child, they are located more densely and work more actively. But over the years, their activity weakens, and some of the sebaceous glands die off altogether.
Before puberty, the consistency and chemical composition of sebum changes. During puberty, hormones (androgens) act on the sebaceous glands, under the influence of which the secretory activity of the sebaceous glands increases. The maximum is reached by 18-25 years.
Significantly more sebum is produced, but in addition it becomes denser. When the follicles of the pilosebaceous ducts are clogged with a “plug” of a mixture of sebum and dead skin flakes, acne vulgaris develops (another name is comedones, acne).
If the follicles are open, the plugs look like blackheads on the face and are called open comedones. Comedones can also be closed (they do not communicate with the surface of the skin). These comedones are called whiteheads, or whiteheads.
If the cause is not eliminated and excess sebum is not removed, then favorable conditions are created inside the follicle for the proliferation of pathogenic bacteria and microorganisms. The bacteria Propionibacterium acnes (P.acnes) are constantly present on our skin, which, under unfavorable conditions, begin to actively multiply and cause inflammation in the pilosebaceous follicle.
Metabolic activity of P. acnes
Involvement in inflammation
A number of in vitro studies have shown that certain strains of P. acnes are able to trigger inflammation in skin cells through different mechanisms [19–22], while other strains are associated with healthy skin [23], [24]. Analysis of the P. acnes genome has revealed putative differences between them that may help explain its dual role [25].
It is clear that there are also proteins that are encoded in the genomes of all P. acnes, for example, CAMP (Christie-Atkins-Munch-Peterson) factors (5 in total). Inhibition of CAMP2 has been shown to attenuate inflammation in a mouse ear model. Their exact role in vivo is unclear, but they appear to be quite important since they are conserved in all P. acnes.
conclusions
The variety of microorganisms on our body is enormous. You can imagine the skin as a giant country whose population is constantly changing under the influence of the outside world, the immune system and interactions with neighboring countries. That is, with the microbiome of the surface of the eyes, intestines, and mucous membranes. The totality of genomes and metabolic pathways of some microbial symbionts can work for the benefit of our body [26], because some bacteria are capable of carrying out reactions beneficial to humans. Such representatives of the microbiome can be assessed as another human organ [27].
Changes within our body adjust the living conditions of bacteria. Thus, with increased secretion of sebum, changes in its qualitative composition occur.
The microbiome is a complex dynamic system. If we more fully characterize the relationships within it, it may provide additional insight into modern human evolution. Helps assess whether and how evolving technologies and lifestyle changes affect health and susceptibility to disease. In particular, to acne.
It is now known for sure that quantitative and qualitative changes in the microbiome complicate the course of acne. P. acnes secretions are thought to contain several proteins that may cause inflammation. However, since acne is a multifactorial disease, it is worth taking into account other causes, such as care, genetics, stress, nutrition, etc. In addition, P. acnes has a number of useful features: it “protects” us from S. aureus by acting as a role of a probiotic. So it is incorrect to blame her for everything.
Studies have begun to appear showing that the introduction of normal flora preparations improves skin condition (Aspergillus, Bifida Ferment Lysate, Lactobacillus/Rye Flour Ferment Filtrate). They show that one of the promising directions in the treatment of acne [28] (and not only) can be pro- and prebiotics, and drugs based on them.
Due to the complex systems of interaction between micro- and macroorganisms, the result is not always predictable. Studying the function of the microbiome in health and disease is an urgent task in medicine. And there are still many questions to be answered.
Thanks for reading the article! We will be happy to answer your questions in the comments.
Causes of acne
There are many causes of acne, but the main ones are:
- increased blood levels of male sex hormones (androgens)
- action of propionic bacteria (Propionibacterium acnes)
- follicular hyperkeratosis
- excess sebum production, changes in its composition
* Sebaceous gland cells have a high affinity for the male sex hormone - testosterone. They also contain an enzyme (5-alpha reductase), which converts testosterone into its active form (dihydrotestosterone). It is he who is involved in the formation of rashes and increases the secretion of sebum.
Therefore, to identify the causes of acne, it is recommended to study the amount of sex hormones.
* The appearance of rashes in the second phase of the menstrual cycle (“before menstruation”) is most likely associated with the effect of progesterone, the level of which increases. This hormone has the ability to somewhat suppress the immune system and retain fluid in the body. All this leads to increased activity of bacterial flora and the development of inflammation in the sebaceous gland.
Often, increased sebum production is the result of increased sensitivity of the sebaceous glands to sex hormones, and not a consequence of their high levels. In this case, a genetic predisposition to acne comes to the fore.
* Hyperkeratosis is an increase in the upper, stratum corneum layer of the skin. Lack of vitamin A, occupational intoxication, prolonged pressure or friction of the skin, exposure to petroleum products (for example, lubricating oil) on the skin are the main causes of hyperkeratosis. Hyperkeratosis of the sebaceous glands also develops under the influence of hormones. It is the cause of acne. With hyperkeratosis, the sebaceous glands become overcrowded with epidermal scales and bacteria, causing acne.
* Rashes may appear or increase in number under stress, since sebum production is regulated by the nervous system.
* Often patients note the appearance of rashes while eating certain foods. These include nuts and chocolate. But these are rather individual characteristics of the body and there is no clear diet for this disease. However, animal fats (lamb fat and lard), vegetable oils, nuts, hot cheeses, and spices can affect the composition of sebum and lead to blockage of the sebaceous glands.
* Comedogenic cosmetics can lead to acne formation.
Acne-provoking cosmetics (creams, lotions, powders, blushes, sunscreens for tanning) contain lanolin and its derivatives, squalene, sulfur, D and C red pigments (used to give a red tint and are extremely comedogenic). Acne-aggravating cosmetics contain mineral and vegetable oils. As a rule, with acne, cosmetics are used to disguise pimples and acne, aggravating the course of acne. A vicious circle is formed. Pay attention to the non-comedogenic label on the packaging of both decorative and care products.
* Some medications may cause rashes (medicinal acne). Drug acne is characterized by the sudden appearance of pus-filled pimples or pimples in people taking corticosteroid medications. After stopping oral contraceptives, many women also experience moderate acne.