Childbirth by caesarean section is one of the oldest surgical operations. There are many indications for its implementation; the main goal of the manipulation is to preserve the health and sometimes the lives of the mother and baby.
In our realities, a cesarean section is performed strictly according to indications, and after the operation is completed, doctors continue to closely monitor the woman’s well-being and the recovery processes in her body. After all, despite the fact that this operation seems quite simple, and medical technologies are constantly improving, it is still a surgical intervention.
Expert opinion
What exactly and how should a woman be monitored if she has had a caesarean section, says Elena Borisovna Machneva
, Candidate of Medical Sciences.
Of course, the recovery processes after a natural birth and after a cesarean section birth are different. During childbirth, many changes occur in a woman’s body, for which nature prepared the expectant mother throughout pregnancy. These are various changes in the cardiovascular, endocrine, respiratory systems, blood coagulation system, etc. Some of these changes are activated during a cesarean section, while others follow a different scenario.
At the same time, during surgical childbirth, the woman’s body is subjected to additional load and stress due to systemic or local anesthesia, as well as the large wound surface that occurs as a result of abdominal surgery. Therefore, in addition to the general recovery processes, in the postpartum period after a cesarean section there are also processes of restoration of the nervous system after anesthesia, as well as healing processes of postoperative sutures.
Since both normal and cesarean births always go differently for everyone, the recovery period for each individual woman also has individual characteristics. A woman should definitely consult with the obstetrician-gynecologist who delivered or operated on her about these features and about the protective regime after childbirth.
Is it possible to completely remove a scar after a caesarean section?
Women should be immediately warned that it is impossible to completely get rid of any scar from a physiological point of view. However, modern means make the seam almost invisible. You shouldn’t succumb to advertising tricks that promise to remove the scar forever in a few days, and you shouldn’t thoughtlessly resort to “folk recipes.”
If you already have an unsightly scar after a cesarean section, then you should consult with a specialist or first study modern methods of scar correction. If you are just about to encounter this problem, then it is worth finding out how you can prevent the formation of a rough pathological scar.
IMPORTANT: The problem of getting rid of scars should not be put off for a long time. All non-surgical methods of scar correction are especially effective at the very beginning of scar formation. The older the scar, the more difficult it becomes to get rid of!
Sutures after childbirth: materials and technologies
Childbirth is a complex physiological process that affects many muscle groups, tissues, and organs.
For a woman, labor involves significant physical exertion and, unfortunately, does not always occur without undesirable consequences. Most often, obstetricians encounter tissue ruptures that require immediate and effective suturing. Two types of materials are used for suturing:
- self-absorbing and represented by catgut of animal origin or semi-synthetic threads;
- non-absorbable threads based on silk or nylon.
The seam can be continuous, fixed only at the beginning and end of the cut, or consist of separate parts, each of which is secured with a knot.
Why is it that sometimes almost invisible scars form after a cesarean section, and sometimes they are voluminous and ugly?
Scar formation is a natural tissue healing process during which connective tissue fibers form at the site of a surgical incision (or wound). Depending on how the healing process proceeds, the future appearance of the scar largely depends.
If the healing process proceeds without complications and the young mother does not have a genetic predisposition to the formation of excess scar tissue, then the result is the formation of a pale, almost invisible normotrophic scar. But in some cases, a pathological scarring process starts, the scar tissue grows, and an unsightly, voluminous pathological scar forms at the site of the wound. It is very important to properly care for the postoperative scar, then the healing stage will be shorter and the scar from the operation will be less noticeable.
The type of future scar also depends on the type of suture.
What's the best way to care for a scar?
Massage and silicone therapy, according to real reviews, are two simple non-surgical methods to minimize the appearance of an unsightly scar.
The use of silicone, along with reducing the unsightly appearance and size of the scar, can also reduce discomfort from burning, toothache, and redness.
If a woman has a large, dense or sensitive scar, she can try a special massage. But you need to get the approval of your doctor. You can begin this treatment after the wound is completely closed without any remaining red inflamed areas. You need to gently touch the scar with your fingers, using natural oils or cosmetics without aggressive ingredients.
You can massage the scar in a circular motion, making up/down movements, working approximately a centimeter of skin around the incision. Repeat the massage several times a day. Pay more attention to dense areas, in such areas apply light pressure, which should not be painful or cause discomfort!
What incisions are made during a caesarean section?
Such an operation has long ceased to be considered a dangerous surgical intervention on a woman’s body, because the technique of execution and the means used have already been sufficiently established. In short, the process consists of the following steps:
- the doctor first cuts the abdominal wall;
- then makes an incision in the uterus;
- removes the child;
- retrieves the placenta;
- puts a suture.
The delivery operation is performed under local or general anesthesia. The decision on the method of anesthesia is made by the anesthesiologist depending on the condition of the patient, the fetus and many other factors. But recently, doctors are increasingly using the first method. Your attending physician will provide details.
There are several options for making the cut. The surgeon can choose one of them. The speed of healing and tissue restoration depends on what he applies. This will also affect the appearance of the scar on the abdomen after a cesarean section.
Corporal section
In most cases, the scar after such an incision will be of impressive size - from the umbilical area to the pubic area. The healing process is quite long. In addition, scar tissue grows gradually and the injury site becomes denser.
Not everyone knows how to get rid of such a scar after a caesarean section, and it is not easy to do. The good news is that this incision is used only in emergency cases when fetal hypoxia or severe blood loss is present. When the question is about saving the life of a mother and child, the appearance of a scar is the last thing that worries the doctor and the patient. The main thing is to save lives.
Cross section
Widely used today. It leaves a small, neat scar from a caesarean section on the abdomen. But it's not just about aesthetics. Cross cuts allow you to:
- reduce the duration of the operation;
- reduce blood loss;
- speed up the healing process.
There are several types of transverse incisions, depending on the technique used:
- Pfannenstiel method - after surgery and in the absence of complications, the scar will be practically invisible. It looks like a thin thread of 10–12 cm. And over time, the scar may completely disappear. The operation is low-traumatic and the wounds heal quickly;
- Joel-Cochin method - an incision is made below the umbilical zone by 5-7 cm, after the intervention a scar of no more than 20 cm remains. During the operation, the doctor cuts the uterus in the upper part. The advantage of this technique is a less painful postoperative period. The fat layer mitigates trauma.
Reviews
- Yulia, 31 years old
I had a cesarean section due to diabetes. Unfortunately, after 1.5 years, the stitch remained, despite the fact that I followed all the doctor’s instructions. Now I’m thinking about going to a laser clinic.
My seam became less noticeable after just a year. To look at the dynamics, I took photos by month, and then compared the healing.
Unfortunately, due to the transverse position of my son, I had to agree to a caesarean section. Half a year has passed, and this red scar still doesn’t go away... it doesn’t even lighten.
A caesarean section is a surgical procedure in which the baby is removed from the uterus through an incision in the abdomen. It is not easy, and those who consider such childbirth easier than natural ones are wrong. Such an intervention carries many risks. A caesarean section is prescribed when there is a threat to the life and health of the child and mother. Caesarean section is indicated under certain conditions when the decision to perform it is made before the onset of labor.
When is a second caesarean section “threatened”?
Repeated caesarean section is recommended for girls who, for various reasons, cannot or do not want to give birth on their own. But even if a woman dreams of natural childbirth, she may well be prohibited from having it if there are the following indications:
- little or, on the contrary, a lot of time has passed since the birth of the first baby - if it is less than 2 years old, then the scar after a cesarean section is not yet strong enough, and if it is more than 8 years old, then it has already lost its elasticity;
- there were complications after the last operation - in case of a difficult rehabilitation period during the first cesarean, the procedure will be scheduled again the second time;
- incompetent scar - if it is thinner than 2.5 mm at the time of planning conception and less than 5 mm by the thirty-fifth week, then there is a high risk of rupture during natural childbirth;
- vertical suture - if the incision was longitudinal, then subsequent independent childbirth is excluded.
The healing process of any suture is individual, so it is impossible to predict with 100% probability what kind of scar will result. However, there are methods to prevent the formation of unsightly pathological scars.
The essence of the procedure
The laser that will remove the scar consists of several beams that come at a short distance from each other. Some of them are deliberately directed at the scar itself. In it, they evaporate the columns of scar tissue, and the scar has to bring the edges between the micro-holes closer together. So it shrinks from the inside.
Some of the laser beams hit healthy skin around the scar. They cause a thermal reaction here, as a result of which the cells that are responsible for the formation of new skin elements are activated. They synthesize 3D scaffold structures, and they creep onto the scar, causing it to be replaced by normal covering tissue. This way the scar also shrinks on the outside.
- Find out the current offers
- Sign up for a consultation
Online registration
The procedure is sterile: in the area where the laser beams hit, the temperature becomes high - more than sufficient to destroy microbes. There are no burns: the cooling is turned on while the laser device is operating.
There will be no bleeding during the procedure: all blood vessels that fall within the laser’s area of effect are sealed. And if the beam hits the pigment spots, which also often surround the scar, then they also disappear.
When should you start preventing scar formation?
Prevention of the formation of a pathological scar can begin after complete epithelization of the wound (2-3 weeks after surgery). As already written above, if a woman removes a post-cesarean scar and makes it less noticeable, then its correction should begin as early as possible.
The speed and effectiveness of the scar correction process depends on the stage of formation. Scar formation is usually divided into 3 stages.
- The initial stage lasts 5-7 days after surgery and ends with the appearance of the primary scar. The seam is bright red or burgundy in color, with clearly defined edges. There is some pain, but this is natural during healing. Besides, they will pass soon.
- The second stage lasts about a month. During this period, the primary scar begins to thicken and changes its color to a less bright one. Pain and discomfort in the scar area stops. But itching may appear, which in some cases lasts up to a year. With a transverse cut, the seam softens within 12 months, and with a vertical cut, this process can last 2 years.
- The last stage lasts about twelve months and depends on the characteristics of each woman’s skin regeneration. During this period, the process of filling the wound incision with epithelium and connective tissue occurs, and a dense scar is formed. The number of vessels in the scar tissue decreases sharply, so the scar changes its color to pink or pale pink.
Once a scar has gone through the final stages of scarring, it becomes much more difficult to remove.
Find out which method of correcting scars and stretch marks is optimal for you!
doctor Svetlana Viktorovna Ogorodnikova.
doctor
Performing a cosmetic seam
The technique for suturing the edges of the wound and the type of threads are selected in accordance with the characteristics of the operation and the presence of certain diseases or complications. To apply a cosmetic suture, special atraumatic needles and other instruments used in plastic surgery are used that do not injure the skin and subcutaneous fat. Suture material is a very thin mono- or poly-fiber thread made of lavsan, silk or synthetic material.
Currently, subcutaneous sutures are most often used, which dissolve on their own within a few weeks after surgery. If their application for some reason is not possible, the integrity of the tissues is restored with non-absorbable threads. In this case, the ligature is removed approximately 7-8 days after the operation. Removal of suture material usually coincides with the day the patient is discharged home.
What scars are called pathological?
After a cesarean section, a healthy normotrophic scar can form. This is a thin elastic scar located at the same level as healthy skin and almost similar in color to it. Over time, these scars themselves become thinner. They require virtually no correction, and if desired, they can be made even less noticeable with the help of peelings and proper care.
However, after surgery, pathological scars may form, most often these are hypertrophic and keloid scars, less often atrophic. In a nutshell, we’ll tell you how to distinguish one type of scar from another.
- Hypertrophic scars - clearly protrude above the skin within the suture, and may even decrease in size over time.
- Keloid scars are a very unpleasant type of scar; they also protrude above the skin, but gradually grow beyond the boundaries of the previous wound, penetrating into healthy tissue.
- Atrophic scars - consist of thinned tissue, located below the level of healthy skin, outwardly they seem to sink inward. When correcting this type of scar, an important step is to activate the skin’s production of healthy collagen, which will fill the sunken area.
Possible complications
Early complications after surgery include:
- Inflammation of the wound after infection. Accompanied by suppuration and swelling of the suture and the surrounding skin, fever, chills, and deterioration in general well-being.
- Divergence of wound contours and rupture of threads. Most often it occurs due to early removal of threads, high physical activity or injury.
- Bleeding and hematomas as a result of extensive damage to blood vessels or certain vascular diseases in a woman in labor.
The listed early complications are diagnosed in the hospital or in the first days after discharge. Treatment depends on the nature and severity of the pathology and includes taking antibiotics, hemostatic drugs, additional dressings or additional suturing of the wound.
Many of the effects of a cesarean section become apparent months after birth. The most common late complication is ligature fistulas, which form as a result of the body’s rejection of suture material or infection of the threads. Their symptoms are:
- redness and slight pain in the scar area;
- periodically occurring suppurations;
- the gradual formation of one or more holes in the skin (fistulas), in which ligature stitches are visible.
If signs of ligature fistulas are detected, you must immediately consult a doctor to surgically remove the remaining threads and treat the wound.
Other rarer long-term consequences of surgical delivery include hernias (bulging of soft tissue on the surface of the scar) and keloid scars. The seal does not pose a threat to health and is purely a cosmetic defect. Such scars usually occur only in patients who are predisposed to excessive tissue growth.
How to get rid of scars after cesarean section at home?
The choice of the optimal correction method depends on the type and age of the scar. Of course, the financial capabilities of a young mother also play a significant role. However, experts do not recommend resorting to the cheapest means, the effectiveness of which has not been proven. Such unprofessional or homemade “medicines” can provoke rapid growth of scar tissue, and there is also a high probability of losing valuable time and missing the period when the scar can be easily corrected.
If you have a young, loose scar, then conservative methods of treating scars in the form of skin applications of anti-scar gels or creams are suitable for you.
If you have an old, dense scar, then using only skin products will be ineffective and it is best to entrust the choice of correction method to a specialist. The presence of internal seals in the scar area, as well as painful sensations, may indicate the development of an adhesive process, in which case a trip to the doctor is vital.
Products for the correction and prevention of young scars.
- Silicone-containing gels and plates
- Anti-scar agents based on collagenase
- Products based on hyaluronidase
- Hormone-based products
- Products with plant extracts, vitamins, oils
Silicone-containing products are designed to moisturize and soften the skin in the scar area. Silicone-based gel is capable of prosthetizing the insufficient function of scarred skin, due to which the water balance in the epidermis is normalized and the scar is softened. Silicone-containing plates (bandages, patches) are designed in such a way that they are able to exert slight pressure on the scar, mechanically preventing the growth of the scar.
If you have already formed a protruding scar, then using only silicone-containing preparations will be ineffective (it is necessary to use products that can destroy scar tissue).
Now there are a large number of silicone-containing products from different manufacturers. Your choice should be based on the reputation of the manufacturer.
Collagenase is an enzyme that breaks down pathological scar tissue. Volume scars are formed when, during wound healing, pathological collagen appears instead of healthy collagen. Pathological collagen fibers are bonded to each other with hyaluronic acid. Collagenases are capable of destroying the very basis of the scar: pathological collagen and hyaluronic acid.
There are a number of collagenase-based products, but not all of them are equally effective because they contain enzymes of different activity. Experts highlight the product Fermenkol. The complex of collagenase enzymes included in its composition destroys pathological collagen and hyaluronic acid to individual amino acids.
Collagenase is used both to prevent scar formation and to correct existing scars. If you have a young scar, then skin applications with Fermencol gel will be sufficient. If the scar is older, then experts recommend using physiotherapy (phonophoresis, electrophoresis) together with Fermenkol. The procedures can be performed in a clinic or at home; all you need to do is purchase a phonophoresis kit.
Hyaluronidase is an enzyme that breaks down hyaluronic acid. As mentioned above, the basis of a pathological scar is pathological collagen, which is bound by hyaluronic acid. The destruction of hyaluronic acid leads to positive external changes in the scar (it decreases in volume), but if pathological collagen is not destroyed, then there is a high probability that the scar will later acquire its previous size and consistency.
Experts recommend using hyaluronidase-based products as a component in complex scar therapy. In this case, the set of measures should contain agents that can destroy pathological collagen.
Hormonal products contain synthetic or natural hormones (corticosteroids and glucocorticoids). They are prescribed exclusively by a specialist! To avoid adverse side effects, you must strictly follow your doctor's instructions and adhere to the dosage regimen. Self-use of products containing hormones is highly discouraged! In addition, it must be remembered that there are a number of contraindications. Pregnant and breastfeeding women should be especially careful when using hormonal medications; many of them are contraindicated for them.
Hormones prevent scar formation by reducing collagen production, and also inhibit areas of inflammation and fibroblast proliferation. Most often, hormonal agents are used in combination with other methods of scar removal.
Most often, products of this type contain fruit acids, which during use provide a light superficial chemical peel. When correcting a pathological scar, the result of such peeling will be almost invisible. But for caring for a neat normotrophic scar, a similar method can help make a neat scar even a little less noticeable.
Vitamins and all kinds of nutrients have a restorative effect on a fresh wound, promoting rapid healing and thereby preventing pathological scarring. Products with nutrients can be used to care for young scars for minor cuts, wounds and abrasions. They are also suitable for caring for a normotrophic scar after a caesarean section. But you shouldn’t count on any positive effect if your pathological scar has already begun to grow.
IMPORTANT: When using anti-scar agents, remember that the scar has natural stages of development: extensive growth, plateau, spontaneous regression of the scar. Sometimes the use of a remedy coincides with the natural stage of regression, which creates the illusion that the treatment is effective. Normotrophic, atrophic and hypertrophic scars can themselves decrease over time. Therefore, if you continue to use some product, but notice that the positive effect has stopped, this most likely means that the product itself was initially extremely ineffective.
Means for the correction of mature scars.
As noted above, using only skin products to get rid of mature scars will be ineffective and the choice of correction method is best left to a specialist. However, now there are special compact devices that allow you to carry out physiotherapy with anti-scarring agents at home.
- Physiotherapy with anti-scar agents based on collagenase. As mentioned above, collagenase-based products, such as Fermenkol, destroy the main components of scar tissue: collagen and hyaluronic acid. Physiotherapy (electrophoresis and phonophoresis) are an effective method of introducing collagenolytic enzymes into scar tissue. Thanks to their effect, active enzymes penetrate into deep areas of scar tissue, thereby accelerating the process of reducing pathological collagen. In addition, the procedures themselves also have a beneficial effect.
- Phonophoresis is an effective and painless procedure during which medicinal substances are introduced into the skin using ultrasound. Ultrasound increases the elasticity of connective tissue, stimulates metabolic processes, including intracellular metabolism, enhances the production of biologically active substances and increases the activity of enzyme systems.
- Drug electrophoresis is a common method of physiotherapeutic treatment. The therapeutic effect consists of a simultaneous positive effect on the body of electric current and active charged molecules of the medicinal substance. A drug depot (reserve) is created in the skin and subcutaneous fat, significantly increasing the exposure time of the drugs.
There are a number of compact devices that allow you to carry out phonophoresis and electrophoresis procedures at home. Their use can save patients time and money, and achieve better results in a shorter period of time. It is better to consult a specialist about what type of procedure should be carried out in each specific case. Physiotherapy also has its contraindications.
Recovery after anesthesia
Nowadays, a woman can choose the type of anesthesia that will be used to numb her. However, doctors also pay attention to the following factors when choosing an anesthesia method:
- condition of a pregnant woman;
- fetal condition;
- planning of the operation;
- safety of drugs for mother and child;
- availability of a qualified specialist.
General
This method is most often used in emergency situations as it requires less time to administer. First, the woman is given a “preliminary anesthesia” intravenously. A tube is inserted into the trachea through which a mixture of oxygen and anesthetic gas is supplied, a drug is injected that relaxes the muscles and the uterus, after which the operation itself begins.
Indications for the use of general anesthesia:
- emergency section;
- with a transverse, oblique position of the fetus;
- refusal of regional anesthesia;
- with prolapse of the umbilical cord;
- if there are contraindications for epidural anesthesia.
There are practically no contraindications to general anesthesia, however, there are a number of complications or side effects:
- headache, dizziness;
- cough and sore throat from the tube;
- nausea, muscle pain;
- allergic reactions, respiratory tract infections.
General anesthesia has a greater effect on a child than epidural anesthesia:
- possible toxic effects on the brain, development of perinatal encephalopathy;
- lethargy, drowsiness.
Spinal
This method of anesthesia is used for planned surgery, but sometimes also for emergency surgery, if there are 10-15 minutes of time left. Spinal anesthesia has a number of advantages:
- the drugs used for this anesthesia do not affect the child;
- a small dose of anesthetic is administered, thereby reducing the risk of toxic poisoning if it accidentally enters the blood;
- the anesthetic acts very quickly, which is important, since when the medicine acts, the pressure in the woman’s lower body drops, which leads to oxygen starvation, which means the child needs to be delivered as quickly as possible;
- the muscles of the body completely relax;
- the risk of breathing problems decreases, since the woman is conscious;
- a woman immediately hears the first cry of her child and can put him to her breast.
But there are also disadvantages:
- there is a sharp drop in pressure due to which it is raised artificially before the operation, and since the pressure rises in the mother, it also increases in the child, which can subsequently negatively affect his nervous system;
- the dose of the medicine is one-time and cannot be changed, which indicates that if there are any complications that will increase the duration of the operation, the patient will also have to endure general anesthesia;
- possible manifestations of headaches.
For a child, the most important complication is oxygen starvation, which occurs as a result of a drop in pressure.
Epidural
An anesthetic substance is injected into the spinal canal, as a result of which the woman loses sensitivity in the lower part of the body, but her consciousness remains clear. This method is most often used during planned operations, when there is time for its preparation. In emergency situations, it is problematic to carry out such a procedure quickly.
Epidural anesthesia has contraindications:
- inflammation of the skin at the puncture sites;
- diseases of the spine;
- acute infectious diseases;
- bleeding disorders;
- allergies due to intolerance to anesthesia drugs;
- narrow pelvis and heavy weight in the child;
- in some cases, a scar on the uterus;
- oblique or transverse placement of the fetus.
It is also possible to develop side effects and complications, which are much more common due to the large dose of the drug. Their presence may depend on the skills of the anesthesiologist, but most often the following side effects occur:
- headache;
- trembling in the legs;
- backache.
The child may experience a decrease in heart rate, hypoxia and respiratory failure. But a competent pediatrician can very quickly cope with all these complications.
How to get rid of scars after cesarean section using medical methods?
- Plastic surgery
- Laser resurfacing
- Microdermabrasion
- Deep chemical peeling
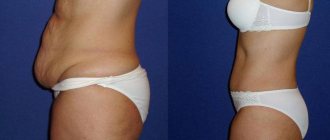
When a scar has already formed and looks extremely unsightly, many doctors suggest getting rid of it by excision. Instead of a rough scar, the woman will receive a barely noticeable mark. This procedure is performed under local anesthesia and requires a period of rehabilitation. To resort to plastic surgery, you need to invest a lot of money and meet all medical indicators.
Another expensive procedure. To achieve the required effect for correcting a scar after a cesarean section, a whole course of treatment will be required, which may require from 5 to 10 procedures. Each procedure is quite painful and involves layer-by-layer removal of tissue. After each procedure, a recovery period is required.
This method of scar resurfacing is considered a more gentle method than laser resurfacing. Scar correction occurs by grinding with aluminum oxide microparticles. To achieve results, a course of procedures will be required (about 6-8 sessions). Each procedure lasts about half an hour. After the procedure, you should not sunbathe or apply unnatural cosmetics to the polished area of the body for 2–3 weeks.
The tripe is first treated with fruit acids, then cleansed with chemicals. This type of treatment is considered the most inexpensive and ineffective, so it is advisable to use it only for mild scars.
Rehabilitation after abdominoplasty
The rehabilitation period after abdominoplasty, of course, takes some time: you need to be prepared for this. You will need to stay in the hospital under the supervision of medical personnel for about 1-2 days. After discharge, come every 2-3 days for examination and dressings: such control over healing allows you to exclude any emergency situations. The sutures from the navel are removed at 10-14 days. The doctor may prescribe antibiotics and rehabilitation procedures.
Many patients are also interested in the question: how is recovery after surgery to remove an abdominal hernia (during abdominoplasty)? As after a classic operation (without removing protrusions), it is important to follow a diet for a month, wear compression garments for about 1.5 months, and avoid physical activity (especially on the abs) for 10-12 weeks. You can start work (not physical) literally after 5 days if the patient’s condition is normal and the doctor has nothing against it.
Recovery from abdominal liposuction takes about two weeks and is a less invasive procedure than a tummy tuck.
During this time, it is worth limiting physical activity and sports.
During the recovery period after abdominoplasty (tummy tuck), it is important not to hesitate to contact the clinic and the surgeon operating on you with any questions. You must inform your doctor about any unexpected ailments, increased body temperature, pain, etc.: it is easier to prevent a problem than to deal with it for a long time later.
Video
Examples of abdominal reconstruction
Abdominal restoration - price
| Name | Price |
| Endoscopic abdominoplasty | 120,000 rub. |
| Abdominoplasty with one-stage waist modeling, category 1 | 220,000 rub. |
| Removal of local deposits of abdominal fat (top or bottom) category 1 | 45,000 rub. |
| Excision of the abdominal fold due to deformation of its lower part (miniabdominoplasty) category 1 | 120,000 rub. |
| Primary appointment (examination, consultation) with a plastic surgeon | FOR FREE |