Intranasal splints SPIGGLE & THEIS are a temporary implant that provides support to the nasal septum, prevents the development of hematoma inside the septum during nasal surgery (septoplasty and rhinoplasty) and prevents adhesion between the nasal septum and the lateral wall of the nose.
The use of splints minimizes the risk of damage to the nasal septum during surgery and in the postoperative period, and helps to accelerate the processes of regeneration of the nasal skeleton. Rehabilitation is much faster and more effective.
The frequency of use of tires is one-time use.
The product is sterile, each pair of splints is in sealed protective packaging to ensure sterility.
The edges of the SPIGGLE & THEIS intranasal splints are rounded and smoothed, which facilitates their gentle, atraumatic insertion and removal. There are holes for fixation with surgical suture material.
Intranasal splints SPIGGLE & THEIS are available in various materials, shapes and sizes.
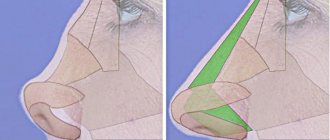
Septoplasty methods
During surgery, the nasal septum is straightened and centered.
Previously, a deviated septum was removed completely, but this caused a lot of complications - for example, there were cases when a patient’s septum sagged after septoplasty, etc.
Some doctors still practice this method today, although this surgical technique is considered outdated.
Modern plastic surgeons strive to preserve the elements of the septum as much as possible as a support for the external nose.
Septoplasty is often performed simultaneously with rhinoplasty.
conclusions
Intranasal splints, or rhinological stents, significantly simplify the early postoperative period, reduce the risk of complications, and provide optimal conditions for regenerative processes. Silicone inserts reliably fix the elements of the nasal skeleton, minimize bleeding, reduce swelling, and prevent infection of the postoperative wound, the formation of crusts and adhesions.
In modern plastic surgery clinics, instead of cotton swabs, only intranasal splints are used. The variety of shapes allows the doctor to choose the optimal silicone insert, which is ideal for fixing the nasal bones and cartilage, taking into account the specifics of the operation.
Types of septoplasty
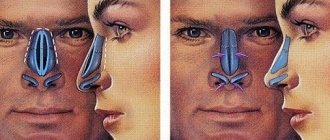
Correction of the nasal septum may require correction of only the bone or cartilage portion. The selection of an effective technique largely depends on the nature of the curvature.
- Endoscopic septoplasty is aimed at giving the nasal septum a central position and correct shape while maximizing the preservation of its tissues. To provide access, the doctor makes incisions on the inner surface of the nose.
- Laser septoplasty is the latest method in which the doctor will correct the shape and position of the nasal septum with minimal blood loss and high precision. The operation is performed through minimal incisions, the mucous membrane heals in the shortest possible time, and the risk of infection is extremely low.
- Ultrasonic septoplasty is performed using an ultrasonic knife, which cuts tissue, coagulating blood vessels, which makes the operation bloodless and shortens the recovery period. Ultrasound surgery eliminates obvious septal defects – spines and ridges.
Intranasal splints made of fluorinated ethylene propylene SPIGGLE & THEIS
Tire material: Fluorinated ethylene propylene (FEP) (fluoroplastic).
Shape: Reuter type (flat oval plate shape with 4/5 length cut).
| Catalog number | Description, dimensions | Number of pairs per package |
| 2041025 | Made from fluorinated ethylene propylene (FEP), size: Standard 42.77 x 25.87 mm, thickness 0.25 mm | 5 |
| 2041050 | Fluorinated ethylene propylene (FEP), size: Standard 42.77 x 25.87 mm, thickness 0.50 mm | 5 |
| 2041075 | Made from fluorinated ethylene propylene (FEP), size: Standard 42.77 x 25.87 mm, thickness 0.75 mm | 5 |
| 2042025 | Fluorinated ethylene propylene (FEP), size: Large 59.40 x 38.86 mm, thickness 0.25 mm | 5 |
| 2042050 | Fluorinated ethylene propylene (FEP), size: Large 59.40 x 38.86 mm, thickness 0.50 mm | 5 |
| 2042075 | Fluorinated ethylene propylene (FEP), size: Large 59.40 x 38.86 mm, thickness 0.75 mm | 5 |
Indications and contraindications
Septoplasty is prescribed if you have:
- Nasal breathing is difficult.
- Chronic/protracted diseases – otitis, sinusitis, etc.
- Frequent nosebleeds.
- Visible nasal defects.
- Noisy breathing, snoring.
- A runny nose as a manifestation of an allergic reaction of the body.
- Dryness of the nasal cavity.
Any of these factors can occur due to a deviated nasal septum, but for surgical intervention the defect must be identified and proven.
Contraindications
- Age up to 18 years.
- Acute or chronic infectious diseases.
- Diabetes.
- Oncology.
- Blood coagulation disorder.
- Hypertension.
Examination and differential diagnosis
Dr. Peter Dawson once said, “Dentists are doctors of the masticatory system.” Every day, doctors carry out interventions in the area of the dentofacial apparatus, correcting the function of the TMJ, masticatory muscles, occlusion, trigeminal nerve system and even the central nervous system (Fig. 1). Disharmony, dysfunction and deformation of the dental system manifests itself in a variety of symptoms, so a thorough examination of the dental status is critical for the planning and implementation of the future treatment protocol, as well as the differential diagnosis phase (Fig. 2).
Rice. 1.
Rice. 2
A systematic approach to examining a patient involves identifying one of three main types of dental disorders:
- Extracapsular: problems of the masticatory system without damage to joint structures.
- Intracapsular: the presence of lesions in the structure of the TMJ.
- Others: general somatic disorders that affect the condition of the dentofacial apparatus; therefore, the treatment process involves the participation of additional specialists (Fig. 3).
Rice. 3
During the examination, it is necessary to ask the patient several questions, for example: “Where do you think the cause of the discomfort lies?” - after all, etiological factors are variable and may include the following:
- pain in the cervical spine;
- somatic pain, which can be triggered by fibromyalgia, chronic fatigue syndrome or rheumatoid arthritis;
- radiating pain as a result of reflex sympathetic dystrophy or chronic regional pain syndrome;
- central neurological, pathological, vascular, migratory or other lesions;
- trigeminal neuralgia with peripheral symptoms.
But, as you noticed, all these questions relate to the need to confirm or, conversely, exclude the presence of so-called other causes of occlusal pathology. Depending on the causative general somatic diagnosis, the use of a splint may be indicated, but may also be contraindicated.
The next question the doctor should ask the patient is: “Does it seem to you that the cause of the disorder is in the joint?” If so, it is very important to determine the diagnosis of articular pathology according to the Piper classification. Intracapsular disorders usually present with disc displacement (partial or complete) with the potential for osteoarthritis, but can also be caused by rheumatoid arthritis or osteoma. Treatment options also directly depend on the diagnosis. To diagnose the condition of the joint, tomography, computer or magnetic resonance imaging methods can be used. Treatment should begin only after a final diagnosis has been made. The patient should also be asked about masticatory muscle problems and occlusion. Occlusal-muscular pathology without affecting the joint area can be corrected through splint therapy, but the doctor must clearly understand which muscle and where should be deprogrammed in order to ensure an adequate pattern of movements of the lower jaw. In order to determine muscle soreness and the state of their hyperfunction, you can palpate the diagnosed area.
During the diagnosis, the doctor should remember the following aspects:
- Clenchers typically experience soreness in the temporal and masticatory muscles.
- The chronic protrusive position of the lower jaw provokes the development of pain in the area of the lateral pterygoid muscles and the anterior neck muscles.
- When registering Hit-and-slide occlusion (transition of the central relation to the state of maximum fissure-tubercle contact), clenchers and bruxists experience pain on palpation of all the above-mentioned muscles (Fig. 4-5).
Rice. 4. Problems begin with a mismatch between the central authority and the central authority.
Rice. 5. When shifting from the CO position to the CO position, muscle incoordination may occur.
Rice. 6. Permissive splint with anterior median contact point and nociceptive trigeminal inhibition function
It has also been found that tension in the temporal muscles often provokes the development of headaches and pain stimulus, which, in turn, triggers a number of vascular changes responsible for the progression of migraines.
Order of conduct
An otolaryngologist can recommend septoplasty, who will analyze the symptoms and complaints and evaluate the clinical picture.
Before surgery, the body should be examined to minimize the risks of complications and identify contraindications.
These tests are mandatory before septoplasty:
- X-ray,
- Fluorography,
- Clinical, biochemical blood test,
- Analysis of urine,
- Analysis for Rh factor and blood group,
- Blood test for hepatitis, syphilis, HIV,
- Prothrombin analysis.
A consultation is also scheduled with a plastic surgeon who will conduct the operation and an anesthesiologist to select the type of anesthesia and medications.
Progress and technique of septoplasty:
- Anesthesia (general or local) is performed.
- Incisions are made in the mucous membrane to gain access to the cartilage tissue.
- Soft tissues peel off.
- The curvatures of the cartilaginous tissues are removed, for which in some cases the cartilage tissues are removed.
- If extracted, the cartilages are reimplanted after correction.
- Stitches are applied.
- Turundas are inserted into the nasal passages.
- A fixing bandage is applied.
Occlusal splints
The two main types of occlusal splints are permissive (permissive) and directive (directive). Permissive splints are formed in such a way as to eliminate painful occlusal contacts and normalize the condition of the masticatory system. The primary task of such splints is to change the occlusion and achieve complete seating of the articular head under the control of the masticatory muscles. Such tires are mainly represented by designs with a horizontal plane. Classic permissive splint designs are those with anterior midpoint contact and full contact. Permissive splints with an anterior midline contact point are designed to separate all teeth except the incisors.
The purpose of their use is as follows:
- Elimination of interfering occlusal contacts to ensure complete seating of the articular head.
- Providing freedom of movement for jaw positioning by eliminating contraction of the masticatory muscles.
- Ensuring free function of the lateral pterygoid muscle and anterior neck muscles when closing the oral cavity.
Using the electromyography method, it has been shown that contact in the molar area allows for 100% of the clamping force, while contact only in the premolar area is 60% of the maximum biting force, and in the area of the incisors only the muscles that lift the mandible can develop only up to 20-30% of the maximum possible jaw compression force. The width of the platform of the median contact point is limited by the width of the 2 lower incisors, which in millimeters is from 8 to 10 mm. Eliminating contact between distal teeth reduces the painful factor that provokes the sensory response. Such a mechanism, through the system of trigeminal interaction, makes it possible to free a person from vascular changes inside the skull, roughly speaking, to free him from headaches and migraines, if the development of such was associated with occlusion disorders. For this purpose, special splints for nociceptive trigeminal inhibition (NTI) are used. Other types of splints with an anterior midline contact point are the Luciajig (GreatLakesOrthodontics, LTD, Tonawanda, NY) (Figure 7) and the B-splint (Figure 8).
Fig.7. Permissive splint with anterior medial contact point Luciajig
Rice. 8. Permissive splint with an anterior median contact point of the B-splint type (for bruxism)
Permissive full contact splints are used to recreate ideal occlusion (Fig. 9). The contacts are formed so as to be evenly distributed over all teeth with full positioning of the joint by the muscles that lift the mandible, or directly by the doctor’s hands. The bimanual Dawson technique is used to seat the joint when the jaw occlusion is adjusted into centric relation by means of a splint (Fig. 10). It is extremely important to ensure adequate joint position when correcting the working position of the mandible. Only with this approach can the maximum therapeutic effect be achieved from the use of a permissive full contact splint.
Rice. 9. Permissive splint with full contact on the lower jaw
Rice. 10. Bimanual Dawson Deprogramming Technique
During excursive movements of the jaw, only the front teeth come into contact, thus reducing the activity of the masticatory muscles. The smooth, flat cusp-to-cusp contacts that form on the splint are designed to provide anterior guidance, which in turn allows freedom of lateral movement, as well as immediate disocclusion of all distal teeth.
Advantages of permissive full contact tires:
- elimination of discrepancies between the proper position of the joint and the established occlusion (CO = MIC);
- increasing the area to distribute the bite force;
- reducing the load on the joint;
- achieving adequate functional occlusion;
- the ability to monitor the stable state of the occlusion and joint.
Permissive full contact splints can be made for both the upper and lower jaws (Fig. 11). Splints on the lower jaw are characterized by certain advantages for practicing doctors :
- Reducing the effect of speech impairment (compared to maxillary splints).
- Less visualization when speaking.
- Possibility of forming deeper retention elements.
- Minimizing the effect of postoperative tooth sensitivity when forming retention elements only on the lingual side.
- Possibility of using splints both during the day and at night.
Rice. 11. Permissive splint with full contact on the upper jaw
Guide elements allow you to adjust the position of the joint so as to remove it from the position that provokes painful symptoms. That is, permissive splints allow the maximum anterosuperior position of the articular head to be achieved under the action of the levator mandibular muscles, while directive splints correct the position of the mandible in the anterior direction based on the design of the splint and excluding the achievement of a centric relation state. Anterior guide splints are used in two cases: for complex joint trauma with swelling of the retrodiscal space and for chronic painful disc displacement (Fig. 12).
Rice. 12. Front repositioning guide splint
Treatment Options
Patients experience the following manifestations of simple occlusal-muscular disorders:
- Minimal symptoms (teeth wear, mobility and change in position of teeth, muscle soreness on palpation).
- Occlusal instability and uncoordinated muscle activity in states of central ratio (CR) and states of maximum fissure-tubercle contact (maximum intercuspidation).
In such cases, using a permissive splint with an anterior median contact point can achieve relaxation of the active state of the muscles for 1-5 minutes. After some time, with the help of a splint it is possible to achieve complete deprogramming of the jaw.
- The occlusal surface covers only the central incisors with the formation of perpendicular contact with the antagonist central incisors. Chairside deprogramming can be done using Luciajig and modeling material.
- The patient should be informed of the need to move the jaw forward/backward along the occlusal surface, after which the position of the jaw is deprogrammed by retrusion over 1-2 minutes. As a rule, the mandible relaxes quite quickly if the articular head is already positioned in the fossa and the lateral pterygoid muscle is adequately relaxed.
- When performing the TMJ orthopedic stress test during the bimanual Dawson's maneuver, there should be no signs of tension or pain.
- Occlusal supercontacts in the central position are easily identified after removal of the deprogrammer.
Deprogramming is a diagnostic manipulation; it allows you to compare diagnostic models in the centric relation, and also helps to conduct a more in-depth analysis of the occlusion and determine the degree of correction required.
Occlusal-muscular parafunctions develop as a result of non-compliance with the criteria for static and dynamic occlusion. After all, problems arise not only with an incorrect bite, but also with excessive chewing loads, which develop the muscles that lift the lower jaw. The combination of incorrect occlusal relationships with parafunctional habits provokes even more disorders in the structure of the masticatory apparatus such as headaches, abrasion facets, muscle discomfort, etc.
Permissive tires with a front medial contact point are capable of:
- Correct malocclusion.
- Reduce the force of muscle activity by separating the distal teeth.
Correction of pain symptoms can also be carried out using similar splint designs, and pain, as a rule, disappears within 24 hours - 1-4 weeks. HTT splints are ideal for the treatment of occlusal-muscular parafunctions.
B-splints are made directly in the blade using 1.5 mm Biocryl (GreatLakes Orthodontics), BIOSTAR® (ScheuDental, Iserlohn, Germany), orthodontic composite and a press. Factory-made HTTs are coated with acrylic directly in the chair and thus customized (KellerLaboratories, Inc (Fenton, MO).
This approach is very effective in the initial phase of splint therapy. When symptoms disappear, an occlusal analysis and appropriate occlusal corrections are performed. In most cases, symptoms do not return even without further use of the splint.
On the other hand, parafunctional habits can pose a significant problem for the clinician even in the absence of obvious occlusal disorders. In some cases, symptoms of parafunction remain even when complete occlusal correction is achieved. When clenching, even under conditions of ideal occlusion, soreness of the temporal and masticatory muscles is observed. In order to avoid feelings of discomfort in the morning, the patient must use a splint at night. It is also important to consider changes in the pattern of parafunction throughout the day and the biological response of the dentition to splint, which can be recorded using a jaw movement analyzer (Bioresearch Associates, Milwaukee, WI). Patients with muscle pain typically keep their teeth in contact even in a “resting state.” This daytime muscle hyperreactivity provokes fatigue and even headaches. A night guard allows you to protect the dentofacial apparatus from nocturnal parafunction, and teeth from pathological abrasion. However, it must be remembered that the use of segmented structures can sometimes provoke intrusion of some teeth and super-eruption of others (which are not in contact with the splint). To prevent this effect, it is advisable to use a double splint on the upper and lower jaws (Fig. 13).
Rice. 13. Double B-slint covering all teeth with anterior midline contact point
Permissive full contact splints allow for a traditional approach to the treatment of occlusal-muscular problems. The use of these structures for 20 days already provides an effective rehabilitation result. Patients themselves note the disappearance of symptoms that previously worried them. A 20-year follow-up of treatment results showed that only 10% of patients after splint therapy required the use of muscle relaxants and sleeping pills. Correction of parafunction is carried out through the constant separation of the distal teeth, which, in turn, reduces muscle soreness, tense muscle pain, and migraines.
Joint lesions often manifest as partial or complete anterior disc displacement. Disc slippage is often associated with:
1) with macrotrauma;
2) with microtrauma, which can be caused by:
a) persistent excessive compression of the joint (parafunction);
b) anterior tension of the disc from sustained contraction of the superior convexity of the lateral pterygoid muscle (malocclusion, parafunction);
3) with a “weak link” in the system as a result of impaired collagen production, ligament weakness and hormonal imbalance.
Partial disc displacement usually develops on the lateral side of the condyle (Piper stage III) (Fig. 14).
Rice. 14. Lateral displacement of the disc with a normal head-to-disc relationship
Treatment using occlusal splints aims to achieve three main goals:
1) the formation of a harmonious interaction between the occlusion, muscles and joints;
2) reducing the load on damaged joint tissues;
3) elimination of symptoms associated with intracapsular edema, inflammation and muscle pain.
Full permissive splints (Fig. 15) are usually prescribed for several reasons:
It is believed that the contact of all teeth allows the load to be distributed over a larger area, thus reducing the load on the weakened joint. With proper distribution, only 5% of the load is transferred to the joint, the rest is “extinguished” by the teeth. The reduced load on the joint, in turn, allows for decompression of the retrodisc space and creates better conditions for healing of the affected area. In cases of partial disc displacement, the use of a permissive splint with an anterior midline contact point provides effective clinical results. In addition, these splint designs are also highly suitable for controlling parafunctional forces by dissociating the distal teeth. Some clinicians are concerned that a permissive splint with an anterior contact point may increase the risk of further disc displacement.
Rice. 15. Permissive splint with full contact on the lower jaw with contact of all teeth during joint positioning
To make a final decision when choosing a splint, additional studies of the joint reaction need to be conducted. We recommend using full permissive splint designs.
Other clinicians are concerned that a permissive splint at the anterior midpoint may pose a risk of further disc displacement. Let's consider these contraindications. Releasing the lateral pterygoid muscles reduces tension forces on the disc anteriorly. Due to the presence of hard and soft tissue damage, more time is required to achieve adaptive stability in the setting of partial disc displacement. Typically, the rehabilitation period takes from 6 to 8 weeks and is combined with the use of anti-inflammatory drugs.
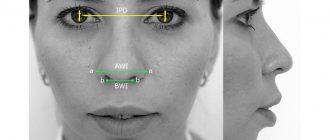
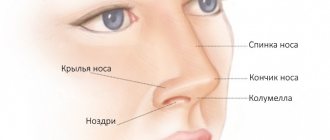
Results of nose correction (rhinoplasty before and after)
The nose occupies a central place on the face. It's impossible to ignore. The shape, size and symmetry of the nose largely determine your individuality, create the overall harmony of your face, and speak about your character and even your age. Rhinoplasty will not only give you a proportionate and graceful nose. As a result of plastic surgery you will receive:
- You will gain a harmonious, proportional and beautiful profile;
- Your face will become more symmetrical;
- The face will look younger (anti-aging rhinoplasty);
- Your facial expression will become more welcoming and open;
- The face can become more European (if you want);
- Breathing will be easier and freer;
- You will feel confident in your external attractiveness.
Another great opportunity that Dr. Kudinova can provide to her patients is profile reshaping surgery (rhinoplasty in combination with chin surgery). This unique method of appearance correction allows you to harmonize facial proportions even in complex cases that other specialists in the field of plastic surgery cannot cope with.
Do you want to change not only your nose, but also other areas of your face? Read our article about a comprehensive change in appearance.
Severe trauma with swelling of the retrodiscal space
In cases of acute injury with swelling of the soft tissue behind the condyle, it is advisable to hold the articular head anteriorly to avoid compression of the affected retrodiscal space. Dr. Parker Mahan, former chairman of the University of Florida Facial Pain Center, even coined the phrase “Cheerleader Syndrome” to describe a clinic of cheerleaders who fell on their chins, causing them to develop joint pain, retroarticular swelling, and acute distal open bites. Examples of such symptoms are also “Airbag Syndrome”, “Barriff Syndrome” and “Extreme Gaming Syndrome”. In such cases, displacement of the articular head anteriorly for a period of 10-14 days is a diagnostic measure, as a result of which it is possible to achieve decompression of the already swollen and painful tissues. This treatment algorithm is also accompanied by an appropriate diet, taking anti-inflammatory drugs and physiotherapeutic procedures.