Laparoscopic reconstructive metroplasty is a surgical procedure aimed at eliminating the incompetence of the uterine scar. The operation consists of excision of the existing pathological scar and the formation of a full suture, which leads to restoration of the integrity of the uterine wall.
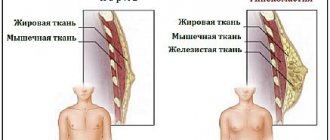
Normally, the wall of the uterus is made up of muscle tissue, which can stretch during pregnancy and contract during labor. But after damage to the wall of the uterus during diagnostic or surgical interventions, muscle fibers can be replaced by areas of connective tissue that are not able to stretch - in this case we are talking about an incompetent scar on the uterus; Most often it is caused by cesarean section. In case of repeated pregnancy, the presence of an incompetent scar is an indication for operative delivery, which quadruples the risk of complications compared to natural birth.
In our clinic, a woman with an incompetent uterine scar, after treatment, has the opportunity to give birth to a child through the vaginal birth canal thanks to reconstructive metroplasty. The operation is performed laparoscopically - all manipulations by the surgeon are performed through three small incisions on the abdominal wall, which after healing become invisible. Moreover, unlike open surgery on the uterine scar, which is accompanied by the risk of bleeding due to the numerous vessels located in this area, laparoscopy of the uterine scar is a low-traumatic surgical procedure and eliminates blood loss.
Find out the cost by phone: +7 (495) 782-50-10
Duration about 60-90 minutes
Time in hospital 3-4 days
Types of scars after cesarean section
By nature, scars after cesarean section are of two types:
- hypertrophic - a compaction that rises above the skin in the form of a roller and is colored pink;
- keloid - an elastic scar that protrudes significantly above the skin, has a purple color and an uneven surface, and can cause pain, burning, itching.
Depending on the intervention technique, scars are also of two types:
- horizontal - remain in 90-95% of cases, reach 10-12 centimeters in length, heal quickly and are more favorable for correction;
- vertical - performed along the midline of the abdomen only for special indications, they take a long time to heal, and are more difficult to correct.
Advantages of laparoscopic reconstructive metroplasty
- Low-invasiveness - thanks to the use of video endoscopic equipment, only the scar is excised, the surrounding tissues are minimally affected
- No blood loss
- Reliable suturing - thanks to the author’s technique used, pregnancy and childbirth naturally become possible in the future
- The use of anti-adhesive barriers during surgery on the uterine scar reduces the risk of formation of adhesions
- Short rehabilitation period and minimal hospitalization period
- Fast recovery after
- Excellent cosmetic result - only three barely noticeable marks remain on the skin.
How is the operation to remove a scar after a cesarean section performed?
Plastic surgery of scars and scars on the abdomen is performed under general or local anesthesia. The method of intervention is chosen individually, depending on the type of scar and on accompanying operations with which plastic surgery can be combined. As a rule, during correction, the surgeon excises the scar, aligns the edges of the wound and applies a cosmetic suture.
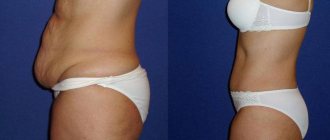
Often, scar plastic surgery after a cesarean section is combined with abdominoplasty - a tummy tuck, or liposuction - local removal of fat deposits. An integrated approach allows you to get rid of overhanging fat and skin tissue in the scar area.
Plastic surgery of an incompetent uterine scar
Caesarean section is one of the most common obstetric operations. Over the past few decades, the rate of cesarean sections in Russia has more than doubled and is about 24%. The increase in the number of these operations occurs mainly due to large obstetric hospitals and perinatal centers, where women with the most severe obstetric pathology and high maternal and perinatal risks are concentrated. The increase in the number of cesarean sections is due to the fact that this operation reduces perinatal risk, and, according to some data, child and maternal injuries. Caesarean section also simplifies delivery in difficult obstetric and borderline situations. But the increase in the number of cesarean sections in Russia and in the world also has certain negative aspects. First of all, this is an increase in the number of women of reproductive age who have a scar on the uterus. And according to statistics, about 30% of women who have had a cesarean section plan another pregnancy in the future. In this regard, the issue of the consistency of the scar on the uterus after a cesarean section and the influence of the condition of the scar on the course of subsequent pregnancies and childbirth is particularly relevant. Therefore, an extremely important problem today is an incompetent scar on the uterus after a cesarean section.
What is uterine scar failure?
The scar on the uterus after a cesarean section (as well as after other operations on the uterus - myomectomy, metroplasty) may or may not be consistent. A healthy scar has adequate thickness and does not contain any cavities. This scar is quite elastic and can stretch and withstand the load during pregnancy and childbirth. An incompetent scar is characterized by its small thickness, the formation of depressions (niches), and a high content of connective tissue. In the literature, there are many terms that describe an incompetent uterine scar: defective scar, cesarean section scar defect, isthmocele, cesarean section niche.
What is the danger of an incompetent uterine scar?
Pregnancy with an incompetent uterine scar is associated with the risk of uterine rupture during pregnancy and childbirth, and abnormal attachment of the placenta (rotation). Perforation of the uterus in the niche area has also been described when an intrauterine device is inserted into the uterine cavity.
Why does an incompetent scar form on the uterus after a cesarean section?
Adequate healing of the suture on the uterus and the formation of a full scar after a cesarean section is one of the main issues of this operation. The healing process of a suture on the uterus is influenced by many factors.
The following risk factors for the formation of an incompetent scar on the uterus after cesarean section can be identified:
- Long operation time
- Major blood loss during caesarean section
- Emergency caesarean section
- Using the Gusakov technique when opening the uterine cavity (promotes the formation of hemorrhages and hematomas in the area of the edges of the incision, there is a risk of the incision going into a vascular bundle)
- Violation of uterine suturing technique, use of inadequate suture material
- Endometritis after cesarean section
Of all the listed factors in the formation of an incompetent scar on the uterus, the main one is endometritis (inflammation of the uterus). In women, the postpartum period occurs against the background of a physiological decrease in immunity, so in the postpartum period various infectious and inflammatory diseases (endometritis, mastitis) arise much more easily. And after a cesarean section, this is “superimposed” by risk factors for infectious complications, such as the presence of a suture on the uterus, edema and ischemia (insufficient blood supply) of tissue in the suture area, and the presence of suture material. Therefore, the incidence of endometritis after spontaneous birth is on average 5%, and after cesarean section - 15%.
How is the failure of the uterine scar formed after a cesarean section?
Early failure of sutures on the uterus, which occurs against the background of progressive acute postpartum endometritis, can manifest itself as pelvic peritonitis (acute inflammation of the pelvic peritoneum due to the entry of infected contents of the uterine cavity through an incompetent suture into the pelvic cavity). In most cases, acute endometritis can be dealt with, but the inflammatory process in the suture area can take a subacute (torpid) course, which leads to slower healing of the suture on the uterus and ultimately to the formation of the so-called late scar failure. The current situation is complicated by the fact that endometritis in most patients after cesarean section initially has a subacute, latent course, leading to late diagnosis.
How does the failure of the uterine scar manifest itself after a cesarean section outside of pregnancy?
The relationship between scar failure and gynecological symptoms in non-pregnant women has been established relatively recently. A niche in the area of the uterine scar can manifest itself as heavy and prolonged menstruation, prolonged spotting before and after menstruation, painful menstruation (dysmenorrhea), pain during sexual intercourse (dyspareunia). It is believed that the main cause of menstrual irregularities is the accumulation of menstrual blood in the niche and disruption of the contractile (contractile) ability of the uterus, which leads to postmenstrual bleeding and pain.
What examination is necessary to identify an incompetent uterine scar?
Pregnancy in women with an operated uterus (after a cesarean section) must be planned and requires preconception examination and preparation. Assessing the consistency of the uterine scar after a previous cesarean section is one of the main issues. Diagnosis of uterine scar failure is always difficult and requires the use of a complex of instrumental studies.
Ultrasound examination is an important method for assessing the course of reparative processes and assessing the consistency of the scar of the operated uterus. Ultrasound criteria for a complete incompetent uterine scar: complete or almost complete (thinning of the myometrium to 2 mm or less) myometrial defect in the form of a niche in the projection of the uterine scar. With partial failure, niches of a smaller size are determined, covering only part of the scar, cavities in the thickness of the scar on the uterus, heterogeneity of the scar and a decrease in blood flow (vascularization) in the scar area, which indicates the presence of scar tissue.
The use of hydrosonography is more informative, since with this diagnostic method the uterine cavity and the niche in the scar area are better visualized. Hydrosonography is an ultrasound examination of the uterus combined with contrasting the uterine cavity with saline solution. The research method allows you to determine the depth of the niche and the minimum thickness of the uterine wall (myometrium) from the niche area.
Magnetic resonance imaging (MRI) of the pelvis is a fairly promising method for assessing the condition of the uterine scar after cesarean section. MRI allows you to accurately determine the size of the niche and the thickness of the uterine wall in the area of the scar, assess the condition of the periuterine tissue and the severity of the scar process in the vesico-uterine space after a cesarean section.
If an incompetent scar on the uterus is detected or suspected based on ultrasound data, hysteroscopy is indicated. This is an endoscopic research method in which the doctor, using a special optical instrument (hysteroscope) inserted through the cervical canal, examines the uterine cavity. Hysteroscopy should be performed in the first phase of the menstrual cycle, when the thin endometrium allows one to assess the condition of the underlying tissue in the scar area. If the scar is incompetent, the presence of a niche or retraction in the scar area is noted. A depletion of the vascular pattern and a whitish color of scar tissue are often noted, which indicates a pronounced predominance of the connective tissue component. Sometimes you can find remnants of suture material and endometrioid cysts in the scar area.
How to treat incompetent uterine scar after cesarean section?
If there is a shallow niche according to ultrasound and hysteroscopy, there are complaints of painful menstruation and postmenstrual spotting, it is possible to perform hysteroresectoscopic resection of the niche. This is an endoscopic operation, which is performed using an optical instrument - a hysteroscope, combined with an electrosurgical instrument in the form of a loop, with the help of which the scarred edges of the niche are cut off, making them flatter. This leads to an improvement in the outflow of menstrual blood from the niche in the scar area and a reduction in the pain of menstruation.
If the uterine scar is completely incompetent, there are complaints, and to prevent complications during planned pregnancy and childbirth, uterine scar plastic surgery outside of pregnancy is indicated. This operation is also called metroplasty. The operation can be performed by laparotomy (open), laparoscopic or vaginal access. Each access has its own indications and contraindications, advantages and disadvantages. But the meaning of the operation is the same - to separate the bladder from the cervix, highlight the scar area on the uterus, excise the scar tissue and suture the uterine defect. With the formation of a full-fledged scar on the uterus, complaints about menstrual irregularities disappear and it becomes possible to plan a pregnancy with lower risks (pregnancy in a niche, rotation of the placenta, uterine rupture along the scar during pregnancy and childbirth).
What complications are possible during uterine scar plastic surgery?
After a cesarean section, a cicatricial adhesive process always occurs in the area of the vesicouterine space. If endometritis and failure of the uterine scar occur after a cesarean section, this is often accompanied by the formation of more pronounced scars in the vesicouterine space, tightly attaching the posterior wall of the bladder to the area of the uterine scar. During subsequent surgery to repair the uterine scar, this may cause injury to the bladder. If damage to the bladder is recognized during surgery, then it is necessary to suture the defect in the bladder wall with a double-row suture and drain the bladder with a urethral catheter in the postoperative period for 7 to 10 days to prevent the formation of a vesicouterine fistula.
How long after surgery is pregnancy possible?
Typically, after the operation, the patient is monitored on an outpatient basis, and an ultrasound examination of the pelvis is performed 1, 3, 6 and 12 months after the operation. If a full-fledged scar on the uterus is formed, pregnancy is planned 9–12 months after the operation.
Doctor's comment
Are you worried about the upcoming operation to remove an incompetent scar on the uterus? However, the proprietary technique used in our clinic excludes the development of any complications during the intervention. Thanks to the practiced methods of anesthesia and modern painkillers, the patient does not experience pain either during metroplasty or after removal of the uterine scar. The laparoscopic method used in our clinic also makes it possible to reduce the length of hospitalization to a minimum; after 1.5 months you can return to your usual physical activities. But the most important thing is that after treatment of the uterine scar, it becomes possible to carry and give birth to a child naturally. If you are just planning an examination, in our clinic you can undergo all the necessary procedures, after which treatment tactics will be selected taking into account the characteristics of your body. Do not delay treatment, because correct diagnosis and timely correction are the first step to happy motherhood!
Head of the surgical service at SwissClinic Konstantin Viktorovich Puchkov
FAQ
Do I need special preparation for laparoscopic reconstructive metroplasty?
A few days before surgery for uterine scar failure, a woman should, in consultation with her doctor, avoid taking medications that affect blood clotting. You also need to avoid foods that cause excessive gas formation. Metroplasty is performed on an empty stomach, with the last meal and water taken eight or more hours before.
How is laparoscopic reconstructive metroplasty performed?
During the operation, to prevent blood loss, atraumatic clamps block the blood flow, after which, under the control of video endoscopic equipment, the scar tissue is excised, while it is possible to visualize the boundaries of healthy tissue and layers of the uterine wall - which allows all manipulations to be carried out with high precision. When suturing the wound, absorbable suture material is used, and modern anti-adhesive barriers are used to prevent the formation of adhesions, which is important for preserving the patient’s fertility. Finally, the clamps from the vessels are removed, and blood flow is completely restored.
What to expect after laparoscopic reconstructive metroplasty?
Bloody discharge can last up to 10 days, in the first couple of days it is intense, it gradually becomes insignificant. In the first week, the temperature may rise to 38°C. Each patient is under the supervision of staff; the condition of the scar is also monitored by ultrasound specialists.
What types of reconstructive metroplasty are there?
There are several methods of performing the operation: transabdominal - through the anterior abdominal wall: the intervention can be performed by laparotomy (open method) and laparoscopy (through three small punctures), as well as transvaginally. Each technique has its own indications, but laparoscopic metroplasty is the least traumatic method.
Are there any disadvantages to laparoscopic reconstructive metroplasty?
The scar is located in an area with good blood supply, which is accompanied by the risk of intraoperative bleeding. If events develop in this way, it may be necessary to switch to an open method. In addition, the seam formed is less reliable. However, thanks to the use of the author’s technique in our clinic, such problems can be successfully eliminated.
How is the rehabilitation going?
Already on the first day the patient begins to get out of bed, on the second day light food is allowed. In the first days, anti-inflammatory and antibacterial drugs are prescribed. Discharge is possible on the third day. Showering is allowed 5-7 days after surgery. A week after the operation, an ultrasound is performed, and follow-up examinations are scheduled after 1, 3, 6 months. For better recovery, the patient is prescribed hormonal medications for a period of 3-6 months. In the first 4-6 weeks, physical activity should be avoided; normal activity is possible after 1.5-2 months. During the first month, it is also recommended to abstain from sexual relations and visiting the pool. It is better to plan pregnancy no earlier than 6-8 months after the end of treatment.