The debate about what is better – natural childbirth or caesarean section – continues. Various methods of delivery are assessed in terms of safety for mother and baby, the ability to quickly establish breastfeeding and return to normal life. Obstetricians-gynecologists, when deciding whether to allow a woman to give birth independently or to perform an operation, evaluate all possible indications and contraindications.
Over the past 10 years, the frequency of cesarean sections (or CS) has increased by 50%: so every third pregnancy ends on the operating table. Is this good or bad?
How does natural childbirth occur?
Modern knowledge about the moment of the onset of labor suggests that the initiator of the “woman’s release from the burden” is the child himself. When the body matures, and the placenta can no longer provide oxygen and nutrients in the required volume, the baby secretes a specific protein into the amniotic fluid. The substance stimulates the production of oxytocin, and uterine contractions begin.
Childbirth consists of three periods. During the first, the muscle fibers of the uterus contract and the cervix opens. During the second, the child passes through the birth canal and involuntarily makes turns. He “groups” by pressing his arms and legs to his body. While moving, the baby feels the pressure of the walls of the birth canal and itself acts on the mother’s tissues. During this period, the woman may be injured (tears of the perineal tissue). To prevent it, protective techniques or surgical dissection - episiotomy - are used.
During the physiological course of childbirth, mother and baby manage to adapt and “go through” this difficult path without damage. In the third period, the birth of the placenta occurs. The total duration of natural childbirth is 6-18 hours.
Early breastfeeding and staying together in the ward become the basis for establishing breastfeeding and forming a strong attachment between mother and baby.
In some cases, childbirth actually begins and ends through natural means, but the difficulties that arise during the process overshadow the joyful memories of meeting the child and cause longer recovery and treatment.
Sources
- Sara L., Millie L., Uma M. P040 Indications for Caesarean Section in Pregnant Women with Inflammatory Bowel Disease: Results from the PIANO Registry. // Am J Gastroenterol - 2022 - Vol115 - NSuppl 1 - p.S11; PMID:33566514
- Singh N., Pradeep Y., Jauhari S. Indications and Determinants of Caesarean Section: A Cross-Sectional Study. // Int J Appl Basic Med Res - 2022 - Vol10 - N4 - p.280-285; PMID:33376704
- Dorji T., Wangmo K., Dorjey Y., Dorji N., Kiran Chhetri D., Tshering S., Wangmo P., Tshokey T. Indications and factors associated with cesarean section in Bhutan: A hospital-based study. // Int J Gynaecol Obstet - 2022 - Vol - NNULL - p.; PMID:33259634
- OuYang Z., Wu J., Zhong B. Society for Maternal-Fetal Medicine Consult Series for cesarean scar pregnancy: each treatment option has its indications. // Am J Obstet Gynecol - 2022 - Vol224 - N1 - p.134-135; PMID:32980360
- Li M., Yin H., Jin Z., Zhang H., Leng B., Luo Y., Zhao Y. Impact of Wuhan lockdown on the indications of cesarean delivery and newborn weights during the epidemic period of COVID-19. // PLoS One - 2022 - Vol15 - N8 - p.e0237420; PMID:32790709
- Lecuyer AI., Baron S., Diguisto C., Laurent E., Turpin D., Potin J., Grammatico-Guillon L. . // Rev Epidemiol Sante Publique - 2020 - Vol68 - N4 - p.253-259; PMID:32591237
- Morton R., Burton AE., Kumar P., Hyett JA., Phipps H., McGeechan K., de Vries BS. Cesarean delivery: Trend in indications over three decades within a major city hospital network. // Acta Obstet Gynecol Scand - 2022 - Vol99 - N7 - p.909-916; PMID:31976544
- Saraya YS., Alashkar A.H., Ali MA., Rajab AM., Saquib N. Indications and rate of first cesarean delivery in the central region's maternity and children hospital. // Saudi Med J - 2022 - Vol40 - N12 - p.1251-1255; PMID:31828277
- Maskey S., Bajracharya M., Bhandari S. Prevalence of Caesarean Section and Its Indications in A Tertiary Care Hospital. // JNMA J Nepal Med Assoc - 2022 - Vol57 - N216 - p.70-73; PMID:31477935
- Chaudhary R., Raut K.B., Pradhan K. Prevalence and Indications of Caesarean Section in a Community Hospital of Western Region of Nepal. // JNMA J Nepal Med Assoc - 2022 - Vol56 - N213 - p.871-874; PMID:31065123
How is a caesarean section performed?
Caesarean section is the process of surgical delivery. During it, the obstetrician dissects the tissue of the anterior abdominal wall layer by layer, then makes an incision in the uterus and expands the hole to the desired size. The baby is removed by hand, the umbilical cord is clamped and cut. Then the obstetrician-gynecologist examines the uterine cavity, separates the placenta, and “cauterizes” the injured vessels to prevent bleeding. Sutures the wall of the uterus and all layers of the anterior abdominal wall, including the skin.
The duration of the operation is 30-40 minutes. At this time, the expectant mother is under spinal anesthesia or general anesthesia. In the first case, she hears what is happening, feels that the doctors are performing some kind of manipulation, but does not see the process itself, since the surgical field is fenced off with a screen. She is shown the baby immediately after birth.
When a caesarean section is performed under general anesthesia, the mother “wakes up” after the operation in the intensive care unit. If everything is fine with the baby, he is brought in the same day.
Depending on the circumstances, a distinction is made between planned and emergency caesarean section. Planned birth is prescribed to women who are not going to be allowed into childbirth. They try to bring his time as close as possible to the preliminary date of birth, and in some cases they wait for the start of contractions. An emergency CS is performed to save the life and health of the mother and child when vaginal birth or further continuation of pregnancy is impossible. During surgical intervention, the woman’s body does not trigger those hormonal changes that are characteristic of the natural process, and the baby does not feel the physiological stress of passing through the birth canal.
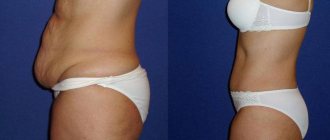
Abdominal restoration after childbirth
Abdominal restoration after childbirth includes a set of measures to eliminate aesthetic and other dissatisfaction. A woman may not be satisfied with sagging abdomen, diastasis, stretch marks... It is worth noting that if diastasis appears, it is necessary to consult with a specialist about correction options: recommended exercises, bandages, etc.
Insufficient attention to the problem can lead to hernias in the future!
Restoring the skin of the abdomen after childbirth worries many women: the skin can stretch after pregnancy, lose turgor, and stretch marks appear as a result.
Using special cosmetics for stretch marks during pregnancy does not always help. They can be eliminated during abdominoplasty if other conservative methods have not given the desired result.
Advantages and disadvantages of various methods of delivery
Supporters of one or another option try to list as many “pros” as possible of the preferred method of delivery and “cons” of the undesirable one. The truth is that physiological birth is truly a natural process. But they can also be painful, uncomfortable, and a sudden change in the situation will require urgent surgical intervention. There are also women for whom surgery is indicated for health reasons.
Pros and cons of natural childbirth
Self-delivery at term is the best scenario for ending the pregnancy. What benefits do they give to women and children? Here are the main advantages:
- a woman can recover quickly and leave the maternity hospital within 2-3 days;
- hormonal “readiness”, rapid attachment to the breast, and being together trigger lactation. The process of breastfeeding is established in a short time;
- the likelihood of postpartum complications is lower than after surgery;
- there are no undesirable effects of drug therapy.
WHO experts indicate that the mortality rate during natural childbirth is 5 times lower than during cesarean section. However, the news article that mentions this fact does not contain data on the initial health status of the mother and fetus.
Proponents of childbirth exclusively through natural means tend to describe the process as long, joyful, easy, and characterize the pain as tolerable. However, complications during childbirth are also possible: characteristics of the mother and child that already exist at the beginning of the process or acute situations that arise. The first group includes:
- multiple pregnancies;
- post-term pregnancies;
- premature rupture of water;
- incorrect presentation of the baby.
Acting in the interests of the mother and fetus, the obstetrician can pre-refer the woman for a CS.
There are no less formidable complications that are impossible to predict:
- abnormal position of the fetus;
- amniotic fluid embolism;
- labor disturbances;
- placental abruption, bleeding;
- uterine rupture;
- loss of umbilical cord loops.
While describing the desire to give birth on their own as a conscious choice, women are not always ready to accept its consequences:
- injuries in a woman in labor;
- death of mother, child;
- severe pain syndrome.
The pros and cons of natural childbirth for a child can be described in three main points:
- the baby passes through the birth canal and turns out to be more prepared for life in new conditions;
- the digestive tract is more quickly populated by normal flora;
- Injuries to the child, bone fractures, and hematoma formation are possible. The risk increases in cases of rapid or rapid labor, and the speed of labor cannot be predicted.
Speaking about the “ordinary” conditions that accompany vaginal childbirth, obstetrician-gynecologists describe damage to the genital organs and pelvic floor muscles in women. So a large fruit or low elasticity of the connective tissue causes ruptures. To facilitate the passage of the baby, the obstetrician performs an episiotomy, after which recovery is faster than with a mechanical rupture. But in both cases, stitches are placed on the perineum. The mother's quality of life deteriorates. Until healing, she is forbidden to sit down; she “adapts” to feed the baby while standing or lying down. Subsequently, cosmetic defects may occur in the perineal area.
Strained pelvic floor muscles cause stress urinary incontinence in 10% of women who have undergone natural childbirth.
It is also worth noting that the first period is the most painful stage of childbirth. Dilatation of the cervix may be accompanied by nausea, vomiting, and chills. Lack of preparation can lead to the fact that the woman is “lost” from pain, begins to panic, and the blood supply to the child suffers. To alleviate the condition, epidural anesthesia is increasingly prescribed, but it is not allowed for everyone.
Pros and cons of caesarean section
Not all women are ready to experience all the sensations that occur during natural childbirth. Some are preparing for surgical intervention and trying to find indications for a planned CS. What are the pros and cons of such an operation for mother and baby? Among the most common:
- the ability to prepare for or “schedule” surgery for a specific date;
- absence of pain characteristic of contractions.
- prevention of perineal injuries, prevention of hemorrhoids. stress urinary incontinence after CS occurs in only 5% of women;
- The operation takes less than an hour, most of it is spent on suturing;
- less trauma to the baby;
- the opportunity to rely on the actions of doctors and not worry about doing something “wrong” and harming the child.
But if operative delivery had only advantages, the CS rate would probably be higher. What do obstetricians-gynecologists say about the “cons”:
- the woman loses more blood, replacement solutions or blood products may be required.
- the patient undergoes anesthesia, recovery from which is incomparable to recovery after childbirth;
- After the operation, the woman receives antibacterial therapy and cannot immediately put the baby to the breast; the lack of timely “switching on” of lactation can lead to difficulties with breastfeeding in the future.
- postoperative bleeding and hematoma formation at the suture site.
- formation of adhesions in the abdominal cavity.
- longer recovery.
- limited number of CS: obstetricians recommend no more than three operations during a lifetime, as the risk of uterine rupture and placental attachment abnormalities increases.
- difficulties with the maturation of the child’s gastrointestinal tract due to the fact that it was not populated in a timely manner by the mother’s microflora;
- violation of the baby’s adaptation to new conditions, respiratory distress syndrome.
Preparation
- 7 - 10 days before the expected date of birth, you will be hospitalized in the antenatal department of the maternity hospital and a date for surgery will be set. Typically, PCS is performed at 38–39 weeks.
! In many modern maternity hospitals, the expectant mother is allowed to come to the ACL on the day of the operation.
- For ACL, you will need to buy special compression stockings or bandages to protect the vessels of the legs from the formation of blood clots;
- On the day of the operation you should not drink or eat - the doctor will remind you of this;
- Two hours before the PCS, you will have a cleansing enema.
Mother's emotions during natural childbirth or caesarean section
Choosing a medical institution, a doctor, drawing up a plan - this is what instills confidence in the heart of the expectant mother. A positive attitude, preparation, and studying relevant literature can give you the feeling that everything should end well.
But real childbirth can cause unexpected negative experiences: too scary, too painful, the midwife does not give a fitball, but puts in an IV. A child is born, but the exhausted mother cannot enjoy the new family member, but constantly returns to traumatic memories.
Or the situation during childbirth changes, and the woman undergoes an emergency caesarean section. She faces pain in the suture area, cannot establish breastfeeding, and most importantly, worries about the “incompleteness” of the pregnancy itself.
Speaking about negative emotions after any method of childbirth, psychologists summarize a woman’s experiences with one phrase - “something went wrong.” Unfortunately, neither a cesarean section nor a completely natural birth guarantees that a young mother will remember them with joy.
Where did the name of the operation come from?
The word "Caesar" is the Greek form of the Latin "caesar" (monarch, ruler). It is believed that the name of this operation is directly related to Gaius Julius Caesar himself. According to legend, the mother of the future Roman emperor died during labor pains. The frightened obstetricians had no choice but to take sharp knives and open the pregnant woman’s womb: they hoped to save at least the child. Fortunately for them, the operation was successful, and a great monarch was born. Since then, such operations have allegedly been nicknamed “caesarean sections.”
On the other hand, the name may be due to the fact that during the reign of Caesar, a law was first passed, which required that in the event of the death of a woman in labor, saving the child: cutting the abdominal wall and uterus and extracting the fetus. The first caesarean section on a living woman with a successful outcome was performed only in 1500. The Swiss Jakob Nyfer, who made his living by castrating boars, distinguished himself. When thirteen experienced midwives could not help his pregnant wife, he asked the city council for permission to perform the operation and personally performed a caesarean section on his wife. Everything went well - the wife and child were saved. According to statistics, for every 6-8 women who give birth on their own, there is one who undergoes a caesarean section.
Indications for caesarean section
When discussing which is better, it should be remembered that before the invention of this operation, the most common cause of death for women was death in childbirth. A caesarean section saves the life of mother and baby. And it is carried out strictly according to indications. They are divided into absolute and relative.
Absolute indications include:
- clinically narrow pelvis (the situation arises during childbirth and is impossible to predict);
- abruption or placenta previa;
- threatened or already begun rupture of the uterine wall;
- incompetent scar of the uterine body;
- pelvic tumors that prevent the baby from moving through the birth canal;
- cervical cancer in women;
- severe cervical ruptures;
- preeclampsia, eclampsia:
- severe somatic diseases;
- varicose veins of the pelvis and vagina.
There are also relative indications in which the issue of surgical delivery is also decided. Obstetricians are inclined to CS if there are two or more conditions from the list:
- incorrect, transverse position of the fetus;
- violation of insertion and incorrect presentation of the head;
- multiple pregnancy;
- post-term pregnancy;
- pregnancy after a long period of infertility;
- breech presentation of the fetus;
- chronic disturbance of uteroplacental blood flow;
- malformations of the female genital organs;
- somatic diseases, including myopia.
It is incorrect to compare what is better - natural childbirth or caesarean section. The operation is a necessary measure that saves the life of the mother and child. Independent childbirth is a physiological process, the participants of which are not protected from injuries and complications.
Postoperative postpartum period. Rehabilitation of a woman
How recovery will proceed after the intervention depends on many reasons and objective factors, including medical ones. Three main problems of this period can be identified.
Pain.
A wound can hurt, as can any postoperative suture. In addition, the involution of the uterus (its reverse restoration) after a CS proceeds in the same way as after a normal birth, so pain cannot be avoided for this reason. Due to the fact that any operation causes a temporary disruption of the intestines, gases will be bothered, which can cause spasmodic pain. To solve this problem, painkillers, symptomatic medications, and, if necessary, antibiotics will be prescribed. Local cooling (an ice pack or hypothermic pack) will help relieve pain in the wound and uterus and reduce swelling.- The seam.
It usually causes discomfort for 1-3 days, and then healing begins. Don't be upset by the unusual color: the reddish or purple tint will go away in a few months, the scar will be barely noticeable. If the incision was cosmetic, then it is made along the hairline, above the pubic symphysis and is not visible there. - Flatulence.
Gases begin to form in large quantities due to atony (decreased normal tone) of the intestines. They move away with difficulty, accumulate, stretch the intestinal walls, the spasm causes pain, nausea, and a feeling of weakness. As soon as the regime is expanded, you will be allowed to get up, bowel function will improve, and flatulence will decrease. These days, it is better to follow a diet that does not contain foods that increase the formation of gases: rye bread, cabbage, peas, sweets, etc.
Possible complications
In the early postpartum period, on the first day after surgery, complications such as peritonitis, endometritis, inflammation of the deep veins may occur. In the late postpartum period: suture dehiscence on the uterus, adhesions in the abdominal cavity.
Spinal anesthesia often leaves unpleasant consequences. An error when placing an injection leads to a puncture of the dura mater. Cerebrospinal fluid leaks into the epidural area. This causes headaches and back pain that can last for several months or even years.
Often difficulties arise due to the simple inattention of obstetricians. When a postpartum mother is placed on a couch after surgery, medical staff sometimes do not straighten her legs and they remain bent. But the woman does not feel the lower part of the body after anesthesia and can spend several hours in this position. This leads to poor circulation. Tissue compression occurs, severe swelling and muscle atrophy develop. After the operation, it is better to draw the nurse’s attention to this point.
When is a caesarean section indicated?
Sometimes caesarean section
prescribed for medical reasons even before the onset of the first contractions.
Planned caesarean section
prescribed for an anatomically narrow pelvis in a pregnant woman, with complete placenta previa, or if the previous pregnancy was also resolved by cesarean section and a scar on the uterus with signs of thinning. Also among the reasons for which a planned cesarean section is prescribed: severe gestosis during pregnancy, the presence of chronic diseases in the mother such as heart disease, diabetes, hypertension, kidney disease, in which natural childbirth poses a risk, as well as exacerbation of genital infections at the time of birth (for example genital herpes).
Sometimes the mother herself chooses the option of a cesarean section, but, as a rule, in the absence of serious complications, doctors strongly recommend natural childbirth.