- Department of Aesthetic Medicine
Department of Aesthetic Medicine » - Injection cosmetology
Injection cosmetology »
- Services
Services "
- Regenerative therapy with autologous fibroblasts
Regenerative (or restorative) therapy with autologous fibroblasts is an amazing procedure that in 2010 moved from the field of experiment to the field of evidence-based medicine.
Regenerative therapy is a cell therapy that restores lost body functions through the transplantation of functionally active cells. The implanted cells release biologically active substances that have a healing and restorative effect.
The patient's own cultured fibroblasts are used for treatment
This unique method has received worldwide recognition as an effective and safe method. That is why regenerative therapy has been introduced into the daily practice of the RAMI Clinic.
Who is this technique for?
It is difficult to find a person in adulthood who would be satisfied with the condition of his skin. Over the years the number of active fibroblasts decreases , this leads to the appearance of wrinkles, drooping tissue of the eyelids or cheekbones.
Modern medicine can effectively replenish the deficiency of living skin cells. This is precisely what regenerative therapy with autologous fibroblasts is designed for, which is equally effective for both women and men .
In addition to correcting age-related changes, therapy with autologous fibroblasts is indicated for the treatment of post-acne scars, stretch marks, as well as during preoperative preparation and postoperative rehabilitation in plastic surgery.
Who conducts the research and develops the SPRS methodology?
This type of technology in Russia is carried out by HSCI OJSC. The same technology on which the fibroblast rejuvenation technique (SPRS technique) is based is patented and approved for use by the Federal Service for Surveillance in Healthcare and Social Development.
The Institute has a full package of licenses and has been continuously engaged in developments in the field of cellular technologies since 2003. Currently, HSCI is recognized as an international biotechnology company with many modern processing laboratories and offices in Moscow, St. Petersburg, Germany and Ukraine. In addition to laboratories, the Institute owns repositories of cellular material and regularly publishes the scientific publication “Cellular Transplantology and Tissue Engineering”.
The uniqueness of regenerative therapy
Autologous dermal fibroblasts are the main human connective tissue cells that form the extracellular matrix. They play a leading role in the physiology of the skin: they regulate all metabolic processes, stimulate cell renewal, and participate in the healing processes of damage.
One of the main reasons for skin aging is a decrease in fibroblast activity. They slow down the synthesis of intercellular space, as a result, the moisture content decreases, the skin fades, and wrinkles appear.
Thanks to the introduction of autologous fibroblasts, tissues start their own metabolic processes, natural restoration and rejuvenation of the skin occurs.
Regenerative therapy technology is absolutely safe , does not cause allergic reactions or rejections, since only natural ingredients are used - the patient’s own cells .
Cell fate and how to change it
The entire variety of cell types in normal development—neurons, skin cells, blood cells, liver cells, and others—is formed as a result of the division and differentiation of a single cell—the zygote. A zygote is formed by the fusion of gametes—an oocyte and a sperm. Then, as a result of cell division, a group of cells is formed - a morula. Next, a cavity is formed - the blastocoel; this stage of embryonic development is called blastocyst. The outer cells - the trophoblast - will participate in implantation and formation of the placenta, and all types of embryonic cells will develop from the inner cell mass. Embryonic development can be thought of as a tree, based on a single cell (zygote), and the branches extending from the trunk symbolize the sequential differentiation of cells. The analogy with the stem is also convenient because embryonic stem (ES) cells, which will be discussed further, are obtained from the cells of the inner cell mass. The cells of the inner cell mass are undifferentiated: they are capable of becoming any type of cell. Each branching of the tree is a choice of fate in the process of differentiation, specialization of cells and narrowing of the spectrum of differentiation. First, there is a division into three germ layers - endoderm, mesoderm and ectoderm. We can additionally distinguish the germinal path and future gametes. Very schematically, further development can be represented as the formation of cells of such organs as kidneys, lungs, stomach from the endoderm; muscles, heart, spleen, blood - from the mesoderm; nervous system and epidermis - from ectoderm. The ability to divide and differentiate into cells derived from the three germ layers is called pluripotency. The developmental program is carried out through the sequential activation of various groups of transcription factors that regulate the expression of many genes. Gene expression is influenced by both internal factors and external signals, such as those received from surrounding cells. Adult stem cells maintain the vital functions of organs and tissues. The different types of stem cells have already been discussed on the “biomolecule”: “Trunk and branches: stem cells” [1].
In experimental systems and in some cases in normal development, changes in cell fate are possible (Fig. 1). If differentiation is the transformation of an undifferentiated cell into a differentiated one, then the reverse process is called dedifferentiation. The transformation of one cell precursor into another is transdetermination. For example, during the process of hematopoiesis, hematopoietic stem cells differentiate into precursors of the lymphoid series (lymphocytes, etc.) and the myeloid series (granulocytes, macrophages, erythrocytes, etc.). It turned out that in an experimental system it is possible to induce transdetermination - using the expression of transcription factors, to change the fate of the precursors of the myeloid series so that they differentiate into the precursors of granulocytes and macrophages, or, in another experiment, into the precursors of erythrocytes [2]. Finally, direct differentiation has recently been demonstrated—embryonic stem cells can be directly differentiated into neurons through the expression of specific transcription factors. This differentiation is called direct because the stages of differentiation required in normal development are absent in this case. Finally, the transformation of a differentiated cell of one type into another without going through the stages of dedifferentiation is transdifferentiation.
Figure 1. Different pathways for changing cell fate. Normal development is the differentiation of a totipotent zygote into various types of cells with a gradual narrowing of the potential for differentiation. In an experiment, you can change the fate of a cell—induce dedifferentiation, transdetermination, or direct differentiation.
All of the above methods for changing cell fate are potentially suitable for use in cell therapy. The possibilities of using these approaches will be discussed below, with an emphasis on obtaining neural cells and using a relatively new direction in research, transdifferentiation.
The effectiveness of the regenerative therapy method
The effectiveness of the technique has been proven by numerous clinical studies in the USA, Europe and Russia.
Specialists from the Ural State Medical Academy and the Institute of Medical Cell Technologies observed 45 patients aged 43 to 60 years who received autologous fibroblast transplants for two years.
As a result , it was revealed that after the procedure, patients’ fine wrinkles disappeared and deep wrinkles were corrected, skin turgor and elasticity increased, and its thickness increased. The effect is increasing in nature, reaches a maximum after 15 months (after the introduction of cells) and persists for at least two years. There were no side effects after the procedure during the observation period.
In 2012, at the RAMI multidisciplinary clinic, modern technology for non-surgical skin rejuvenation based on cell therapy was introduced into everyday practice.
This was preceded by the multifaceted work of our clinic staff :
- studying scientific publications on the use of cellular technologies in cosmetology, visiting international forums;
- participation in experimental work on cell cultivation, consultations with foreign and Russian colleagues;
- search for partners licensed to conduct biotechnological work;
- formation of appropriate material and technical base and human resources of specialists.
How does fibroblast rejuvenation work?
Work using this method involves 2 procedures per 1 course, performed at intervals of 1-1.5 months. During the course of rejuvenation with fibroblasts , the face, décolleté, arms and neck are corrected. The drug is administered using the thinnest insulin needles. An hour before the procedure, the required area is lubricated with an anesthetic cream to reduce the pain of the process.
After the product is in the dermis, the number of active fibroblasts increases: they begin to synthesize collagen at the same speed, and the natural regeneration process resumes. The result of treatment is noticeable rejuvenation, a decrease in the number and severity of wrinkles, an increase in turgor and moisture, and a significant slowdown in the aging process.
How is regenerative therapy treated?
Regenerative therapy with autologous fibroblasts involves 2 stages: clinical and laboratory (biotechnological).
Clinical stage
Takes place in the multidisciplinary clinic “RAMI”.
First, a comprehensive examination of the patient is carried out , indications for the use of this treatment method are established, possible contraindications are identified, and the optimal regimen for administering the drug is determined.
Then specialists from the RAMI clinic take a flap of skin from the behind-the-ear area measuring 0.6*0.6 cm. The resulting biopsy is transported to a specialized laboratory for cell processing (cultivation).
Laboratory stage
It is carried out in a specialized institution that has a license to conduct biotechnological work, isolate, cultivate and store cell cultures. The fibroblast culture obtained in the laboratory is tested for stability, oncological and infectious safety. Each drug that contains a therapeutic dose of cells is issued a corresponding passport .
For intradermal injection into the patient's problem area, a certain therapeutic dose of fibroblasts (at least 1 million cells) is required, which is determined by the doctor.
The collection of a skin flap, its transportation, and intradermal introduction of cells are carried out under conditions of maximum sterility.
The time for culturing cells and forming a fibroblast culture in a specialized laboratory is 25 - 29 days. The resulting fibroblast culture is frozen in liquid nitrogen and stored for the required time in compliance with all requirements.
Next, a preparation of living fibroblasts is prepared from the resulting culture in the form of a suspension, 1 ml of which contains at least 1 million functioning fibroblasts. The time required to prepare the drug is 5 - 7 days.
Skin rejuvenation with your own fibroblasts.
The essence of SPRS therapy® is that a piece of skin with a diameter of 4 mm is taken from the patient’s ear (where the skin is least damaged by UV rays) and a fibroblast culture is obtained from it. In the skin of every person, regardless of age, fibroblast precursor cells are present. In culture, they are able to form colonies - clones consisting of tens and even thousands of fibroblasts, developed from a single precursor cell. This means that in a person of any age, from a small fragment of skin, you can obtain the number of fibroblasts necessary for therapy. We are not exaggerating when we talk about “any age”: in the skin of even a 95-year-old person there are up to 14% active fibroblasts!
As it turned out, by culturing cells it is possible to obtain a very interesting individual characteristic of the skin, on the basis of which one can calculate the value of the regenerative potential of fibroblasts (that is, their ability to maintain tissue self-regulation and restore it when damaged), on the basis of which a conclusion can then be made about the regenerative potential of the skin in general, and, therefore, its ability to self-heal. The magnitude of this potential is individual for each person, it does not depend on his age. Taking this indicator into account, it is possible for each patient to develop his own individual program for skin renewal and restoration (the so-called “Skin Passport®” and “SPRS program”).
What is it for? Everyone is familiar with this situation: two patients of the same age undergo the same procedures, then one is completely delighted, and the other complains that there is no point. “Skin Passport” helps predict the result, find out who will easily get an excellent effect, and who needs to undergo preparatory procedures. This is the essence of the individual SPRS program.
The process of introducing cells into a problem area
The schedule for introducing cells into the problem area of the skin depends on:
- the time required to obtain a cell culture;
- therapeutic dose of a living cell drug;
- individual characteristics of the patient's skin;
- from choosing the optimal treatment regimen recommended by the doctor.
Cell injection area
The area into which fibroblasts are injected intradermally is determined jointly by the doctor and the patient. As a rule, problem areas of the face are selected - around the eyes, nasolabial folds. The cell preparation can also be injected into the neck and décolleté area.
Of particular interest is the use of autologous fibroblasts for rejuvenating the skin of the dorsum of the hands. Autologous fibroblasts can be injected into the area of scars, stretch marks, and wrinkles.
Depending on the depth and severity of skin changes, a papular or tunnel method of administering the cell preparation is used.
Live cell injection procedure
- the procedure is performed under local anesthesia. The doctor injects a drug enriched with fibroblasts into the patient’s problem area with a thin needle;
- depending on the problem, several sessions may be required;
- the procedure is performed under local anesthesia. Using a thin needle, the doctor injects a drug enriched with fibroblasts into the patient’s problem area;
- After the procedure, slight redness and swelling may occur, which will disappear within 2 - 3 hours.
When active fibroblasts are introduced into the skin, the natural processes of restoration of the dermis are launched. The effect of the procedure begins to appear 6-8 hours after the session and increases over time. 8 - 9 months after the course of treatment, a persistent positive result is observed.
Result after regenerative therapy
After the introduction of cultured fibroblasts, the number of dermal cells in the treated area increases, the synthesis of its own collagen increases, microcirculation is restored, metabolic processes and blood circulation are stimulated.
The high efficiency of the method is due to the ability of implanted living cells to produce biologically active substances characteristic of young skin for a long time (8-9 months): its strength and elasticity increases, and a lifting effect occurs.
The result of implantation of living cells: wrinkles, scars, and stretch marks disappear. The dermis is completely renewed, healthy skin color , its turgor increases, the skin becomes velvety , dryness and flaking disappear.
How safe is fibroblast rejuvenation technology?
The technology of fibroblast rejuvenation is 100% safe, which is confirmed by the results of a huge number of preclinical and clinical studies (Russian and foreign). All of them speak about the high efficiency and safety of using cultured own dermal cells to slow down the aging process. More information about these studies can be found here. It is worth emphasizing that each sample of material taken from a patient is necessarily tested for biosafety in order to exclude the presence of a number of viruses and bacteria.
Difference from other methods
The main difference from other methods is the drug used. The patient's skin is restored using its own cells , which are cultured in the laboratory.
During the procedure, living cells are transplanted onto the skin, which dramatically accelerate the skin regeneration mechanism due to their production of growth factors and components of the dermal framework. The method not only corrects visible skin defects , but also restores it at the microtexture level.
Modern cosmetological techniques (antioxidants, hydrants, elastic stimulants, biostimulants, capillary protectors, etc.) have a certain rejuvenating effect, but the principle of action is based on correcting the effects of aging. Cell replacement therapy solves the problem of skin aging on a fundamentally different level: the process of reducing the reserves of one’s own skin cells stops. This means that the aging process in the treated area is not only stopped, but even reversed.
Regenerative therapy treats age-related skin changes when other methods only correct their consequences.
Those lazy fibroblasts
Now we look at the reports of scientists: after 40 years, a woman’s body experiences a decrease in the production of hyaluronic acid. Every year it becomes 5% less. This means that the gel “filler” weakens and the number of collagen fibers decreases. The “springs” themselves become thicker and stiffer. And between the “springs”, under the influence of external forces, folds – wrinkles – are formed.
And why all? Because fibroblasts (cells living in the hypodermis) synthesize less and less hyaluronic acid. Unfortunately, this happens not only due to age. The aging process is genetically programmed in us: some people maintain youthful skin up to 50 years old, while others don’t look their best at 30.
The following sources were used in preparing the material:
- “30 years of experience in the development and application of cell technologies in clinical practice.” V.P. Tumanov, D.A. Zhakota, N.S., Korchagina. Scientific and practical journal “Plastic surgery and cosmetology”, 2012 (3), Moscow, Russia.
- Isaev AA, Prikhodko AV, Zorin VL, etc. Medical technology “Collection, transportation, isolation, cultivation, cryopreservation, storage and use of autologous fibroblasts for the correction of age-related and scarring changes in the skin.” FS No. 2009/308 dated July 21, 2010, Moscow, Russia.
- “The use of autologous dermal fibroblasts to correct age-related changes in facial skin. Results of one-year research.” Authors: V. Zorin, A. Zorina, V. Cherkasov et al. Journal “Aesthetic Medicine”, volume XI No. 2, 2012, Moscow, Russia.
- “Qualitative and quantitative assessment of the condition of facial skin after the use of autologous dermal fibroblasts.” Authors: V. L. Zorin, A. I. Zorina, V. R. Cherkasov, P. B. et al. Journal “Bulletin of Aesthetic Medicine”, volume 10, No. 2, 2011, Moscow, Russia.
Perhaps you will find it useful:
- Post-traumatic, post-burn regeneration of the skin
If you are really looking for your doctor...
In this article we will talk about the function of dermal fibroblasts in the skin, their aging process, as well as the method of renewal and stimulation of skin regeneration by introducing autologous fibroblasts.
Introduction
The role of dermal fibroblasts (DF) in skin renewal is difficult to overestimate, since they are the main cellular component of the connective tissue basis of the skin, ensuring its homeostasis and morphofunctional organization. The relevance of this topic for regenerative (reparative) cosmetology, the task of which is to rejuvenate the skin by activating the natural processes of its restoration, is obvious.
Functions of dermal fibroblasts
Of all the functions of DF, the greatest attention of specialists in the field of aesthetic medicine and dermatology is focused on the production by these cells of the components of the extracellular matrix (ECM) of the dermis: collagen, elastin, proteoglycans, especially hyaluronic acid (HA), and structural glycoproteins.
The increased interest in this particular function of the DF is understandable: the named components of the ECM form and maintain the structure of the skin, ensuring its elasticity and strength. Moreover, DF not only synthesize these substances, but also ensure their catabolism through direct phagocytosis of “spent” fragments of collagen and elastin fibrils, secretion of collagenase, hyaluronidase and other enzymes.
Resident cells of a tissue are those that are formed and permanently reside in this tissue.
Another, and no less significant for the skin, activity of DF remained until recently somewhat on the sidelines of the field of view of practitioners, but today it is also becoming the object of close attention of clinicians. We are talking about a number of important functions of fibroblasts. Thus, by producing type IV collagen and laminin, they influence the formation of the basement membrane. Fibroblasts form stroma, which not only serves as a framework (support) for the epithelium, but also regulates the structural organization and functioning of epithelial cells. They produce and secrete cell growth factors (KGF-1 - keratinocyte growth factor, GM-CSF - granulocyte-macrophage colony-stimulating growth factor), immunoregulatory interleukins IL-6, IL-8. Due to the secretion of growth factors and interleukins and direct interaction with epithelial cells, DF play a key role in the regulation of epidermal morphogenesis. Their paracrine activity serves as the basis for maintaining the homeostasis of stem keratinocytes.
Dermal fibroblasts secrete factors that influence lymphocyte differentiation and factors that regulate the number, migration and function of granulocytes and macrophages, thereby maintaining skin immunity. By producing a variety of proangiogenic factors that induce differentiation and migration of endothelial cells, DFs contribute to the formation and stabilization of blood vessels.
They take part in the processes of neuroendocrine regulation of the skin. They synthesize biologically active peptides: hormones, biogenic amines, neuropeptides and neurotransmitters, identical to those in the central nervous and endocrine systems, express androgen and estrogen receptors, through which the influence of these hormones on human skin is achieved.
Fibroblasts, interacting with various resident cells: epidermal, endothelial, nervous, adipose, hematopoietic, participate in almost all skin processes, including physiopathological ones. Thus, DFs represent a central link in the biology of the skin: they support not only the homeostasis of the ECM of the dermis, ensuring its remodeling and renewal, but also the physiological state of other layers and structures of the skin.
Rice. 1. The relative position of fibroblasts and collagen fibers: a - in the skin of young people (18–29 years old); b - in the skin of older people (over 80 years old) (Varani J., et al. 2006, as amended)
Involution of dermal fibroblasts
As the body ages, the number of DFs in which age-dependent changes occur, mainly associated with the continuous accumulation of damage, increases. Such DFs are designated as “senescent” or senescent fibroblasts (DFst). Their ability to remodel and organize the ECM decreases, as their synthesis and secretion of the main components of the ECM decreases. Epidermal homeostasis is disrupted due to negative changes in the paracrine mechanisms connecting the epidermis and the papillary layer of the dermis. In the DFst population, there is an increase in the secretion of the cysteine-rich angiogenic inducer protein 61 (CYR61, or CCN1), which stimulates the production of proinflammatory cytokines and matrix metalloproteinases (MMPs). CCN1 and MMPs support cellular aging by negatively regulating collagen homeostasis and increasing its degradation.
Gradually, the balance between collagen synthesis and degradation is disrupted in favor of the latter. The damaged collagen framework of the ECM can no longer hold fibroblasts in the stretched state characteristic of young cells. A kind of collapse of fibroblasts occurs, which leads to disruption of their functions. During the process of involution, the number of fibroblasts decreases. The biosynthetic activity of these cells also decreases, and the balance between the synthesis and degradation of the ECM of the dermis is disrupted. On average, in older people, compared to young people, the total amount of DF is 35% less, collagen production in the skin is reduced by 75%, and collagen content decreases by approximately 1% per year.
All senescent changes in the DF population lead to a gradual and significant decrease in the skin's ability to regenerate and renew. How does this change the status of the skin? Its thickness decreases, its firmness and elasticity decrease, wrinkles, creases, and tissue ptosis appear—the skin ages.
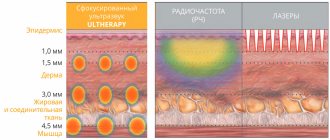
It is obvious that it is DF that should be the main “target” of skin rejuvenating cosmetic methods. So it is: all modern therapeutic interventions for the purpose of correcting age-related changes in the skin - injection, including PRP therapy, hardware (laser, radio frequency, ultrasound) - are aimed primarily at stimulating the functional activity of DF, both proliferative and biosynthetic. A special place in this series is occupied by the use of autologous (own) dermal fibroblasts, or SPRS therapy.
SPRS therapy as a method of skin healing and renewal
SPRS therapy (SPRS - from the English Service for Personal Regeneration of Skin - a personalized set of therapeutic and diagnostic procedures for skin restoration) is a method of regenerative medicine (RU FS No. 2009 / 308 dated 07/21/2010). Its use makes it possible to replenish the DF population that has decreased with age due to specialized young and functionally active cells introduced into the skin. The patient’s own skin fibroblasts are transplanted, so they fully take root, integrate with the resident cell population and live “according to the laws” of the dermis.
After transplantation, their biosynthetic activity remains for at least a year, without any additional stimulation. As a result, the synthesis of collagen and other components of the ECM increases, due to which the microstructure of the dermis is remodeled, its thickness increases, and the number and depth of wrinkles decreases.
Senescence is a condition in which cells with accumulated DNA damage and depleted DNA repair mechanisms stop dividing and lose the ability to remodel and organize the ECM.
Rice. 2. Skin after using autoDF: a — after 1 month, b — after 3 months, c — after 6 months, d — after 12 months. Arrows indicate groups of introduced cultured autoDFs. Left column—hematoxylin and eosin staining, right column—silver nitrate impregnation. Uv. ×200. Preparations and microphotographs of R.V. Deev.
Description of technology
In a specialized laboratory of the Institute of Human Stem Cells, which complies with international GMP standards*, a cell preparation containing cultured autologous DF (autoDF) is obtained from a 4 mm biopsy of the patient’s skin. At the stages of cellular processing, only functionally active DFs are selected and stimulated, which, despite the aging of the body, retain a high ability to divide and synthesize components important for the skin. The fact is that the proliferative potential of the entire population of dermal fibroblasts of an adult throughout his life remains at a fairly high level - due to the presence of stem / progenitor cells in the fibroblastic differential. These are precursor cells that are responsible for renewing the cell population of the dermis. In vitro studies have shown that primary cultures obtained even from very elderly people (95 years old) contain up to 14% mitotically active fibroblasts.
Rice. 3. Relative change in skin thickness after the use of autoDF (according to the results of histological studies).
This fact is confirmed by our experiments: cultures of dermal fibroblasts obtained from patients 18–82 years old are characterized by a fairly high efficiency of colony formation (45.0±9.5%), regardless of the age of the donor. This makes it possible to obtain the number of functionally active cells necessary for therapy from a small biopsy of the skin of any adult.
After transplantation of cultured autoDFs into the dermis, their biosynthetic activity is maintained. In our work, we injected the resulting cellular material simultaneously into both the facial skin and the skin behind the auricle, from where a biopsy sample was then taken for histological examination. Our research has shown:
- transplanted autoDF synthesized dermal ECM components for at least 12 months [Fig. 2];
- transplanted autoDF were present in the dermis in small groups, without signs of mitotic activity, that is, without signs of cell division (hence, there is no risk of developing any hyperplastic processes when using them);
- new collagen fibers were formed;
- dermal thickness increased by an average of 62.5±13.6% (p=0.028) during the first 12 months after the use of autoDF [Fig. 3].
24 months after the use of autoDF, separate groups of fibroblast-like cells were also recorded in the dermis [Fig. 4], producing collagen fibers. However, no signs of collagen maturation (thickening) were observed, which means that two years after autoDF transplantation, the intensity of their synthetic activity (compared to that during the first year after transplantation) was reduced.
Rice. 4. Skin of patient M. (54 years old) after using autoDF after 24 months. Left column—hematoxylin and eosin staining, right column—silver nitrate impregnation. Uv. ×200. Preparations and microphotographs of R.V. Deev.
Most likely, this is due to the level of physiological needs of the dermis (it is known that to ensure its physiological state, a minor functional activity of fibroblasts is sufficient). Apparently, the transplanted autoDFs have fully integrated with the dermis, become a natural component of its main cell population—fibroblastic differon—and are under the control of the microenvironment.
Conclusions of histological examination:
- introduced autoDF retain their viability in the dermis;
- they are located in the dermis mainly in groups;
- their functioning does not lead to adverse consequences, the cells are not proliferatively active;
- At all periods of observation, signs of an increase in its volume and the process of synthesis of young collagen fibers are recorded in the dermis.
The positive dynamics of skin changes revealed at the histological level after the use of autoDF fully corresponds to the clinical picture. Already 10–14 days after the end of the course of SPRS therapy, an increase in skin elasticity, a decrease in its relief (reduction in the severity of wrinkles), and an improvement in the color and contours of the face are noted. The effect is growing. So, if a month after the injection, 88% of patients rated the clinical result as “good” or “excellent”, then after three months and later - 100%. Research doctors determined the result as “good” or “excellent” in 86% of patients after a month, and in 100% of patients after three months and later. Positive changes in skin condition that progress over time (over at least 12 months) have been confirmed by us using instrumental research methods.
Conclusion
Innovative technology - SPRS therapy, based on the principles of regenerative medicine - allows you to restore the structure and functions of the dermis lost with age due to the unique biological mechanism of the patient’s own collagen-forming skin cells.
SPRS therapy has been used in domestic aesthetic medicine for more than eight years; more than 1,000 clinical observations of patients have been recorded, of which more than 80% have repeatedly (two or more times), having treated one area of the skin, gone to clinics to treat the skin of other areas with this method.
It is important for medical practice that SPRS therapy is not only an independent effective method of dermal remodeling, but also a good basic basis for the use of other cosmetic interventions aimed at stimulating the synthetic activity of fibroblasts, which allows maintaining the patient’s skin in good condition for a long time.
Authors: Alla Zorina, Ph.D., biochemist, Moscow. Vadim Zorin, Ph.D. Sc., biophysicist, Moscow.
Magazine: Appearance. Esthetic guide №6(29)