About the Demodex mite
There are two species of these mites found on humans: Demodex folliculorum and Demodex brevis.
Demodex mites can also live on various types of animals, in particular on dogs, which also suffer from demodicosis. But a person cannot become infected from an animal, since those ticks belong to other species and cannot live on humans. Demodex mites are considered opportunistic. This means that they can live on the skin of a healthy person - their presence does not always lead to the development of the disease. Different studies indicate different prevalence of Demodex. In any case, at least 50% of people are carriers of these mites; some researchers put the figure at 97%. It is believed that among children and young people there are fewer carriers of Demodex mites, the number of carriers increases with age, and almost all older people are affected by this mite.
Demodex lives in the sebaceous glands and hair follicles, preferring the face to other parts of the body. Larger mites, Demodex folliculorum, most often target the hair follicles of the eyelashes and eyebrows. Demodex brevis prefers to settle in the sebaceous glands of the wings of the nose, nasolabial folds, and chin. However, mites can also be found on other areas of the skin, including the cheeks, neck, chest and back.
Demodex mites are not visible to the naked eye. An individual of Demodex folliculorum can reach a size of 0.5 mm; Demodex brevis is even smaller - no more than 0.15 mm. Demodex does not like light and is most active at night. The most comfortable temperature for it is 30-40 °C, so the tick becomes active in the spring and summer.
Cosmetology procedures
Even after a sharp reduction in the number of mites, the skin remains vulnerable to external influences and is not able to withstand new possible exacerbations of the disease. This is due to its damage and disruption of its protective properties.
The following procedures have worked well in the treatment of demodicosis:
- electrophoresis: acts in 2 directions - the electric current is unfavorable for mites, but at the same time it conducts useful substances deep into the skin, moisturizing it;
- atraumatic facial cleansing and microdermabrasion: indicated in the remission stage in the absence of active inflammation; the purpose of the procedures is mechanical removal of the top layer of skin inhabited by mites;
- chemical peels: aimed at deep cleansing the skin and are a good prevention of demodicosis;
- photo and laser therapy: prescribed to eliminate vascular defects, reduce skin lumpyness, remove pigmentation and improve the overall appearance of the skin.
During the treatment of demodicosis, it is not recommended to use decorative cosmetics and fatty creams, which favor the proliferation of mites. You cannot independently reduce or extend the course of the drug prescribed by your doctor. Strict adherence to the instructions received speeds up the achievement of the expected result.
Causes of demodicosis
In a healthy person, the activity of the Demodex mite is suppressed by the body's immune defense. With a decrease in immunity, there are more ticks, which leads to the development of demodicosis. Also, an increase in the number of mites can be caused by metabolic disorders. Demodex feeds mainly on the secretions of the sebaceous glands, so increased productivity of the sebaceous glands leads to the activation of mites and, as a consequence, manifestations of demodicosis.
Thus, the list of the main reasons for the development of demodicosis may look like this:
- decreased general immunity;
- stress factors (stress and negative emotions contribute to decreased immunity);
- chronic diseases leading to a decrease in the protective ability of the skin;
- increased skin oiliness;
- hormonal changes (in particular during adolescence, when as a result of such changes the viscosity of the secretion of the sebaceous glands increases);
- use of cosmetics with hormonal supplements;
- failure to comply with personal hygiene rules.
Drug therapy
Combined treatment of demodicosis includes the use of:
- local antiparasitic agents;
- systemic drugs to enhance immunity;
- desensitizing drugs and vitamins.
The best antiparasitic activity is demonstrated by ointments and creams containing non-hormonal substances (zinc, sulfur, etc.). They block the respiratory process of ticks, thus leading to the death of the parasites. The use of local medications is carried out in courses at short intervals, lasting from several weeks to several months.
Symptoms of demodicosis
Mites destroy the cells of the follicle walls and sebaceous glands. This leads to the appearance of keratinization, foci of inflammation, and pigmentation. Demodex migrates across the skin, exploring new areas; Thus, with increasing demodicosis, the signs of damage spread over an increasingly larger area. It is also assumed that mites cause sensitization of the body, that is, an allergic reaction is added to mechanical damage.
The main symptoms of demodicosis are:
Acne (acne)
Juvenile acne in most cases is a manifestation of demodicosis.
Skin redness
Redness may be accompanied by swelling of the skin.
Itching
Itching with demodicosis usually intensifies at night, when mite activity increases.
More about the symptom
Skin changes
Progressive demodicosis leads to changes in the skin: roughening, peeling, and the appearance of thickenings similar to scars. In the advanced stage, the skin takes on an earthy color.
Blepharitis
When Demodex affects the eyelashes, signs of blepharitis (inflammation of the ciliary edge of the eyelids) develop: the eyelids begin to itch, turn red, swell, and may stick together. The eyes water, inflammation spreads to the conjunctiva - conjunctivitis develops. Loss of eyelashes is observed.
2. Symptoms of the disease
In low concentrations, the demodex mite does not manifest itself in any way. The skin's own immunity does not allow the parasite to have a negative impact on it. But under certain unfavorable conditions, the protection weakens, and the tick begins to actively feed and reproduce. Sebum contributes to this. Signs appear on the skin, collectively called “problem skin”: acne and pimples, enlarged pores, inflammation of the sebaceous glands. Most often, the parasite is localized on the chin, nose, cheeks, and forehead. The skin becomes unhealthy, oily shine appears, firmness and elasticity are lost. Mite damage to the eyelids also leads to inflammation, sometimes even leading to eyelash loss. The skin becomes lumpy, painful, itching and a tickling sensation on the skin often occur - these are parasites moving along the surface. Demodex is especially active in the evenings and at night.
Visit our Dermatology page
Methods for diagnosing demodicosis
The symptoms of demodicosis coincide with the symptoms of some other diseases (dermatitis, allergies). Acne with demodicosis is similar to the manifestations of rosacea (rosacea disease). Therefore, laboratory diagnostics are necessary to confirm the diagnosis.
Demodex analysis
The material for analysis is a scraping from the skin. If the eyelids are affected, eyelashes are taken for analysis. Next, a microscopic examination is carried out, which is designed to detect tick individuals or eggs.
More information about the diagnostic method
Sign up for diagnostics To accurately diagnose the disease, make an appointment with specialists from the Family Doctor network.
Treatment methods for demodicosis
Treatment of demodicosis is a long process. On average it takes 4-6 weeks, but in some cases it may take several months.
The difficulty of treating demodicosis, in particular, is that the most effective anti-mite remedies are quite toxic. Therefore, means for the treatment of demodicosis are selected individually, depending on the degree of damage and the patient’s condition.
Treatment must be comprehensive. The course of treatment includes both local and systemic therapy.
Local therapy
Local therapy for demodicosis is aimed at suppressing the activity of the mite. Without the use of local therapy, treatment success cannot be expected.
Systemic therapy
Systemic therapy for demodicosis involves measures to strengthen the immune system and normalize metabolism.
Make an appointment Do not self-medicate. Contact our specialists who will correctly diagnose and prescribe treatment.
Rate how useful the material was
thank you for rating
As is known, mites of the genus Demodex are often considered the etiological and pathogenetic agent in the development of papulopustular dermatoses. An important point is that mites, complicating existing skin diseases, reduce the clinical effect of therapy, thus contributing to the transition of dermatoses to a chronic form. An additional difficulty for antiparasitic therapy is created by the structural features of mites, which makes it necessary to prescribe long courses of therapy and select drugs with a minimum molecular size. The effect of the drug is hampered by the dense cuticle covering the body of the mites, which has three layers: the outer layer is the epicuticle, the middle layer is the exocuticle and the inner layer is the endocuticle. The exo- and endocuticle are impenetrable, so the body of the mite is difficult to access by large molecules of exogenous substances, incl. for acaricidal drugs. Communication with the external environment of ticks occurs through water or gas exchange [3].
In order to achieve the elimination of ticks, antiparasitic (acaricidal) drugs are used. Over the years, metronidazole, which is a derivative of the nitroimidazole group, has proven the greatest clinical effectiveness. This drug is prescribed for a course of 4 to 6 weeks [7, 29]. It has been established that metronidazole enhances the protective and regenerative functions of the mucous membrane of the stomach and intestines [2, 4] and causes a pronounced anti-edematous effect [30]. The drug has a bacteriostatic effect, complicating the DNA synthesis processes of gram-negative anaerobic bacteria [13, 38], and is also antiparasitic against Demodex folliculorum [2].
Studies by DI Grove (1997) and PG Nielsen (1988) have proven the suppressive effect of the drug on some indicators of cellular immunity, in particular the suppression of leukocyte chemotaxis [26, 32]. The drug has an immunomodulatory effect due to the inhibition of vascular endothelial growth factors, preventing neoangiogenesis [15]. Tolerability of the drug is generally satisfactory. Side effects include headache, nausea, vomiting, dry mouth, urticaria, itching, leukopenia, candidiasis [13].
A.A. Frankenberg (2007) notes that in recent years, failures in the treatment of demodicosis with metronidazole have increased significantly. In his opinion, the ineffectiveness of therapy may be associated with the development of resistance of bacterial-parasitic flora to metronidazole, which has been used for more than 40 years [16]. As an alternative method of treating demodicosis, Ya.A. Yutskovskaya (2010) suggested using metronidazole topically. The study showed significant clinical improvement, which was manifested in a decrease in erythema, the number of papulopustular elements and the severity of the inflammatory process. According to the authors, laboratory elimination of mites after 14–21 days reached 2–3 mites in a scraping per 1 cm2 [17].
From the group of other synthetic antibacterial agents, the 5-nitroimidazole derivative ornidazole is widely used in cycles of 8 to 10 days. The drug has both antiparasitic and bacteriostatic effects, increases the activity of neutrophils, stimulates adrenergic structures, and enhances reparative processes [4, 18].
When comparing the effectiveness of the drugs ornidazole and metronidazole A.A. Frankenberg et al. (2007) the following results were obtained: the therapeutic effect when using ornidazole occurs almost 2 times faster compared to metronidazole; patient tolerability of the drug is satisfactory; minor side effects were noted, among which the most common were nausea and a metallic taste in the mouth; The blood and urine test results of the patients before and after treatment were within normal limits. When treated with metronidazole, side effects were observed more often, including: nausea, metallic taste in the mouth, dizziness, and the development of candidiasis. During 9 months of observation of patients taking ornidazole, there was no relapse [9, 16].
When choosing local treatment for demodicosis, one should take into account the general principles of external therapy used in dermatology. In some cases, etiotropic therapy should be immediately prescribed; in some cases, symptomatic therapy should be started, aimed at eliminating and resolving acute inflammatory manifestations and accompanying subjective sensations. Strict personalization of external treatment and constant monitoring of the patient's condition are necessary. In acute and subacute forms of the inflammatory process, you should first use dosage forms with a surface action of agents (lotions, shaken suspensions, pastes). After eliminating the acute inflammatory phenomena, the next stage is to switch to the ointment form of the drug, which acts directly on the etiological factor.
In external therapy, drugs containing metronidazole 1% in the form of an ointment or gel are most often used for 14 days. Metronidazole acts on the body's nonspecific resistance and affects cell-mediated immunity [33, 35]. As an alternative therapy, topical application of 10% benzyl benzoate ointment at night is possible [1, 6, 23]. Demoten gel (sulfur, hyaluronic acid, AloeVera juice, polyvinylpyrrolidone) for the treatment of patients with demodicosis and rosacea was highly praised [14].
In special cases, pathogenetic treatment is carried out for demodicosis. For example, in the case of acneiform type demodicosis or resistance to antiparasitic drugs, it is advisable to use systemic retinoids (isotretinoin) at a dosage of 0.1–0.5 mg/kg body weight per day for 2–4 months [24].
For the treatment of demodecosis of the periorbital region, alcohol-ether mixtures, 3–5% trichopolum cream, sodium sulfapyrazine, anticholinesterase agents (cholinomimetics): physostigmine, 0.02% phosphakol, 0.01% armin, 0.5% - ny tosmilen [11]. Good treatment results are observed with the use of blepharogel-1 and -2, blepharolotion [12].
Recently, dermatological practice has been significantly enriched with new drugs, significantly increasing the possibilities of choice in the treatment of patients with parasitic dermatoses. The drug Spregal, containing a solution of esdepaletrin and piperonyl butoxide, showed high effectiveness. It is used on the affected areas of the skin, rubbing with a swab 1-3 times a day. The drug is well tolerated and does not cause serious side effects [5, 8].
Permethrin (a group of pyrethroids) also has antiparasitic properties. Pyrethroids bind to the lipid structures of nerve cell membranes, disrupting the functioning of sodium channels that regulate membrane polarization. Repolarization of the membrane is hindered, which paralyzes the parasite. The important point is when pyrethroid molecules are able to penetrate the tick cuticle and concentrate in the hemolymph [3]. Permethrin 5% cream is applied twice daily for 15–30 days [31, 37]. However, we must remember that the permeability of different areas of the skin is not the same. Medicinal substances penetrate most actively into the skin of the face, where the thickness of the stratum corneum is minimal, so the rapid development of side effects in the form of erythema and simple contact dermatitis is possible.
The drugs ivermectin, lindane 1%, and crotamiton 10% also have acaricidal activity [23, 29]. Ivermectin is a synthetic derivative of compounds with antiparasitic activity known as avermectins. The drug is effective against endoparasites with tropism for the skin (Strongyloides stercoralis, Ancylostoma braziliense, Cochliomyia hominivorax, Dermatobia hominis, Filaria bancrofti, Wucheria malayi, Onchocerca volvulus, Loa-loa) and ectoparasites (Sarcoptes scabies, Pediculus humanus, Demodex folliculorum and Cheyletiella spr.) [22]. Foreign studies recommend using ivermectin systemically or topically in the form of a 1% cream. Studies have proven that ivermectin has antiparasitic and anti-inflammatory effects. Clinical improvement with topical 1% ivermectin cream was observed after 12 weeks of therapy [27]. The drug is administered orally at a dose of 200 mg/kg body weight twice with a break of 7 days [28]. However, in Russia this drug is used only for the treatment of demodicosis in animals. The use of 1% lindane also raises many doubts due to its neurotoxicity, therefore the drug is banned in a number of countries, and in some its use is limited [21]. As for the drug crotamiton 10%, it is applied to the skin at night for two to three days and is quite often used in pediatric practice [20, 34].
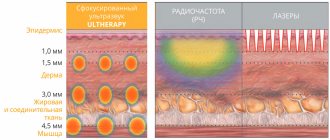
Among physiotherapeutic techniques, it is recommended to use the properties of narrow-band blue light (405–420 nm). The wavelengths of blue light are slightly longer than those of ultraviolet radiation, so narrow-band blue light reaches the reticular layer of the dermis, penetrating to a depth of 2.5 mm, corresponding to the location of the sebaceous glands. Single observations indicate the high effectiveness of this method in the treatment of acne complicated by demodicosis [10]. Some studies have proven the positive effect of using intense pulsed light (IPL - Intensive Pulse Light), discovered in 1992 and having a wavelength from 515 to 1200 nm [25]. IPL radiation suppresses the secretion of the sebaceous glands with their subsequent involution, which leads to the resorption of lymphocytic infiltrates and the death of mites [36].
Cryotherapy has an antidemodic effect, and to achieve a more lasting therapeutic effect, it is recommended to use cryotherapy in combination with external preparations containing metronidazole [1, 19].
Despite the fact that, according to various authors, the current “gold” standard and most effective method of treating demodicosis is the systemic use of the antiparasitic drug metronidazole, the drug itself has many side effects and has a number of contraindications. Since the search for new therapeutic agents that have the least negative effect on the body remains a pressing topic in medicine, we assessed the effectiveness of external therapy for demodicosis in comparison with the systemic use of drugs.
The purpose of this study: to compare the traditional treatment regimen for demodicosis of the facial skin (250 mg metronidazole orally 2 times a day; topically - 1% metronidazole cream once a day for 20 days) with the effectiveness of topical therapy (7% metronidazole cream topically for 20 days).
Material and methods
The study included 64 patients with acne and rosacea complicated by demodicosis. The diagnosis of acne and rosacea was made at the initial appointment based on the clinical picture of the diseases. At the same time, the main complaints of patients were taken into account, divided into the following groups: rashes, pain, burning, redness, itching, pigmentation, the presence of crusts/excoriations, telangiectasia, oily sheen. When assessing the local status (status localis), the following primary and secondary morphological elements were identified: papules, pustules, open comedones, milia, telangiectasia, crusts, redness, pigmentation, oily sheen. Each morphological element was counted and the clinical picture as a whole was assessed for the presence of perifocal erythema and oily sheen of the facial skin in patients before and after treatment. All patients included in the study were examined for the presence of Demodex mites by scraping the facial skin and squeezing out the contents of the sebaceous glands before and after treatment. The diagnosis of demodicosis was established when more than 5 mites per 1 cm2 were detected. The study included men and women over 18 years of age with no somatic complications and upon signing informed consent to participate in the study.
All patients were divided into two equal groups depending on the chosen treatment method. Patients of the first group (n=32) received 250 mg of metronidazole orally 2 times a day, externally - 1% metronidazole once a day for 20 days, patients of the second group (n=32) received 7% metronidazole externally in within 20 days. The treatment method was chosen randomly.
Statistical data processing was performed using the SPSS-21 software package. The relationship between categorical indicators was determined by Fisher's exact method. Fisher's exact test is a test of statistical significance used in the analysis of categorical data when sample sizes are small. To assess the significance of differences in follicle sizes, one-way analysis of variance with pairwise comparisons was used.
Research results
Of all the patients included in the study, 38 (59.37%) had acne and 26 (40.62%) had rosacea. The distribution by gender, age and diagnosis is presented in Table. 1.
The patients' return visit took place after 20 days of continuous therapy. Subjectively, both treatment regimens were well tolerated by the patients, no side effects were noted, and none of the patients were excluded from the observation group. Evaluation of the effectiveness of therapy was based on patient complaints and clinical picture. As can be seen from table. 2, after treatment there was a statistically significant decrease in patient complaints of rashes, burning, pain, itching, and redness. Moreover, in patients of the second group, complaints about oily skin decreased, which is an additional advantage of topical therapy.
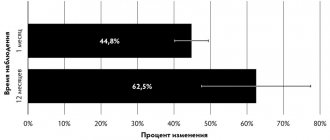
Analysis of clinical manifestations after therapy showed that the number of the following morphological elements in patients of the first and second groups significantly decreased: papules, pustules, perifocal erythema, excoriations (p = 0.005) compared to the initial data (Fig. 1, 2).
When repeated scraping for the presence of Demodeх mites in two groups, the following data were obtained: in the first group, mites were found in 19 (30%) patients, in the second - in 20 (32%), i.e. mites of the genus Demodex after treatment in the two groups were found in approximately equal numbers of cases.
Thus, assessing the results of treatment, we can state that the effectiveness of therapy in both groups was the same. Analysis of the clinical picture showed a positive dynamics of therapy, which was manifested in a significant decrease in the number of morphological elements characterizing the severity of inflammation. The effectiveness of therapy was confirmed by a decrease in subjective complaints of patients after treatment, and in patients who received only external therapy, complaints about oily skin decreased, which is an additional advantage. Thus, clinical observations have demonstrated the lack of superiority in systemic therapy of demodicosis compared to external therapy using a drug containing 7% metronidazole in the form of a cream or cream-gel, which was confirmed by the results of statistical analysis.
conclusions
Our study showed that the use of a topical product containing 7% metronidazole for 20 days by patients with demodicosis is comparable in effectiveness to systemic treatment with metronidazole 250 mg orally for 20 days. External use of 7% metronidazole makes it possible to avoid polypharmacy and systemic administration of the drug, which reduces the risk of developing side effects of therapy.