Perineoplasty is a modern, low-traumatic and highly effective method using vaginal threads. A minimally invasive gynecological operation that does not require general anesthesia, with an immediate effect and a quick recovery period.
Very often, women experience problems associated with an enlarged vaginal opening. This may be a consequence of weakness of the muscles and ligaments that support the pelvic organs in a normal position, for example, as a result of muscle damage during childbirth, epithiotomy, surgical interventions, or age-related decrease in muscle tone. And a number of other reasons.
This condition leads not only to cosmetic discomfort, but is also of great importance for the general health of a woman and the normal functioning of her reproductive system, since it leads to decreased sexual satisfaction, prolapse of the vaginal walls, and is the cause of recurrent inflammatory diseases of the vagina, urinary incontinence, genital prolapse (prolapse). or prolapse of internal pelvic organs).
HAPPI LIFT VAGINAL NARROVER - threads produced only in Italy by Promoitalia and are already recognized by the ministries of health in more than 30 countries, including Russia.
The new caprolactone threads HAPPI LIFT VAGINAL NARROVER have international certificates confirming the products’ compliance with medical standards.
Structure and functions of the female perineum
The perineum , in an anatomical sense, is the area between the pubis and the top of the coccyx, on the sides it is limited by the ischial tuberosities of the pelvic bones, in fact it is the exit from the small pelvis. In a clinical (obstetric) sense, the perineum is considered the area between the posterior commissure of the labia majora and the anus (Fig. 1).
Rice. 1.
Anatomical landmarks of the female perineum: 1 - anterior commissure of the labia majora, 2 - posterior commissure of the labia majora, 3 - anus (anus), 4 - apex of the coccyx, 5 - ischial tubercle (on the left).
The thickness of the perineum consists of the skin, muscles, their tendons and fascia. The set of soft tissues occupying the space of exit from the small pelvis forms the pelvic floor (bottom of the abdominal cavity). The muscles and fascia of the pelvic floor form the pelvic diaphragm. A woman's urethra, vagina, and rectum pass through the pelvic diaphragm. The condition of the perineum reflects the condition of the pelvic floor.
The muscles and ligaments of the pelvic floor support the pelvic organs (bladder, vagina and rectum) in an anatomical position and provide a number of very important physiological functions: voluntary urination and urinary retention, defecation, retention of feces and intestinal gases, closure of the vaginal opening, are part of labor paths (Fig. 2).
Rice. 2.
Sagittal section of the pelvic floor
Back to contents
Advantages of visiting our clinic “Polyclinic+1”
- Competence of doctors. Perioneoplasty services are provided by gynecologists R. A. Sasunova, V.S. Rigas. Our doctors have a certificate that confirms the right to practice aesthetic gynecology.
- Use of proven drugs. We use safe and effective products from well-known pharmaceutical companies.
- Caring for every patient. Before prescribing the procedure, we will make sure that the woman has no contraindications. Fillers are introduced carefully, in small doses, so that the drug is distributed evenly.
- Anonymity. We maintain complete confidentiality, so we do not require passport information.
- Convenience. To make an appointment, just call or leave a request on the website. We are waiting for you any day from 9 am to 9 pm. The clinic is located at the same distance from the Novokuznetskaya and Tretyakovskaya metro stations.
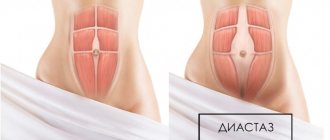
Insufficiency of the perineal muscles
Numerous muscles of the pelvic diaphragm (perineum) are divided into superficial and deep, some of them are sphincters. For example, the bulbospongiosus muscle is a vaginal sphincter - it narrows the entrance to the vagina. For normal functioning of any muscle, at least two points of fixation are required. In Fig. 3 and 4 it is clear that many muscles of the pelvic floor depart from the bones (the first point of fixation) and converge at the center of the pelvic outlet, intertwine with each other and form a second, limitedly movable point of fixation - the tendon center of the perineum.
Rice. 3.
Superficial muscles of the perineum
Rice. 4.
Deep perineal muscles
Damage to the tendon center of the perineum, or separation of the muscle from the tendon center during childbirth leads to insufficiency of the pelvic floor muscles
, as a result, dysfunction of the pelvic organs and prolapse of the vaginal walls develops. (Fig. 5).
Video 1.
Animation of the birth process
Rice. 5.
Perineal injury during childbirth
The first sign of muscle failure is a gaping opening to the vagina (genital slit). Normally, 8-10 months after birth, the genital opening should be closed (closed). The tendinous center of the perineum and the deep pelvic floor muscles hold the rectum in place. If these formations are damaged, the anterior wall of the rectum, together with the posterior wall of the vagina, gradually begins to descend downwards - a rectocele develops (Fig. 6).
Rice. 6.
Scheme of development of rectocele: A - whole tendon center. B - when the tendon center of the perineum is damaged, nothing holds the rectum.
You can diagnose your pelvic floor yourself using a special questionnaire.
Causes of pelvic floor muscle insufficiency
The main cause is trauma to the perineum during childbirth.
- Quick birth, delivery of a large fetus, surgical obstetric care during childbirth;
- Inadequate restoration of ruptures and incisions of the perineum;
- Dystrophy of connective and muscle tissue. Develops as a result of a decrease in the level of female sex hormones (mainly during menopause);
- Connective tissue dysplasia (genetic defects).
- Sedentary lifestyle (sedentary, standing work).
Symptoms of pelvic floor muscle deficiency
Clinical manifestations are directly related to the functions of the damaged muscles and the tendon center of the perineum.
- Gaping of the genital fissure, as a result of chronic vulvitis;
- Suction of air into the vagina during sexual intercourse (not a tight girth of the penis by the vulvar ring);
- Prolapse of the posterior vaginal wall - rectocele. Nagging pain in the perineum;
- Urinary problems;
- Impaired defecation and gas incontinence;
Treatment is carried out by gynecological surgeons. A logical method of treating pelvic floor muscle insufficiency is surgical restoration (reconstruction) of the normal anatomy of the perineum - perineoplasty
.
When pelvic floor muscle insufficiency is combined with rectal prolapse, perineoplasty is performed in combination with plastic surgery of the posterior vaginal wall - posterior colporrhaphy. Back to contents
Perineoplasty classic
Perineal plastic surgery is performed for severe ruptures of the tendon center and cicatricial deformities of the perineum. When a perineal rupture and rectocele (prolapse of the posterior wall of the vagina and rectum) are combined, perineoplasty is combined with posterior colporrhaphy and sphincteroplasty. I wrote in detail about prolapse of the walls of the vagina and pelvic organs in this article.
During perineal plastic surgery, skin scars are excised, tissue is prepared layer-by-layer, and damaged structures of the pelvic diaphragm are restored (Fig. 7)
Rice. 7.
Stages of perineal plastic surgery
Expected results:
- Restoration of function - restoration of normal anatomy leads to normalization of the function of the perineal muscles.
- Cosmetic effect – restoration of the aesthetic attractiveness of the intimate area, narrowing of the vagina.
Back to contents
Contraindications to plastic surgery of the intimate area
Perineal plastic surgery is not performed when diagnosing the following pathological processes and disorders:
- Severe cardiovascular pathology;
- Decompensated chronic diseases of internal organs;
- Inflammatory and infectious diseases of the genitourinary system;
- Venereal pathologies;
- Bleeding disorders;
- Diabetes mellitus in the decompensation stage;
- Excessive scarring of tissue (the appearance of keloid scars).
The advisability of perineoplasty is determined by the attending physician after a thorough examination, laboratory tests and clinical studies. This will allow you to diagnose contraindications and assess the patient’s health status.
Minimally invasive perineoplasty
Another name for the operation is pernieovaginal lifting, which is performed for minor ruptures of the tendon center of the perineum and stretching of the superficial muscles of the pelvic diaphragm (transverse muscle and sphincter of the vagina). Minimally invasiveness is achieved using specially designed long-absorbable threads. The threads are passed in a special way through the muscles, through small incisions in the skin (3-5 mm), and fixed to the tendon center of the perineum. Over time, connective tissue forms in place of the threads and continues to maintain the normal anatomy of the pelvic floor.
As a preventive and therapeutic measure, minimally invasive perineoplasty with vaginal threads can be performed under local anesthesia on an outpatient basis as early as 2 months after birth (the end of the late postpartum period). The advantages of vaginal thread plastic surgery are the possibility of vaginal delivery and a short recovery period. The surgical technique is clearly presented in the following video.
Expected results
- Restoring the normal anatomy of the perineum leads to normalization of the function of the pelvic organs;
- Cosmetic and aesthetic effect - attractiveness of the intimate area;
- Improving the quality of sexual life.
Back to contents
Examination, preparation, postoperative period
During a gynecological examination, the doctor determines the nature of the damage to the muscles of the perineum and the degree of dysfunction of the pelvic organs. Based on the data obtained, the patient is recommended the preferred method of perineoplasty, and a preoperative examination is prescribed. Based on the results, a second consultation is carried out, preoperative preparation and surgery date are assigned.
Examination for surgical treatment and expiration dates of tests
Valid for 6 months:
- Fluorography;
- Cervical smear for oncocytology.
Valid for 3 months:
- Blood test for HIV (AIDS);
- Blood test for RW (syphilis);
- Blood test for hepatitis B and C viruses;
- Ultrasound of the pelvic organs;
Valid for 1 month:
- Blood group and Rh factor.
- Clinical blood tests;
- General urine analysis;
- Biochemical blood tests (sugar);
- ECG;
- A certificate from a therapist with a detailed diagnosis and a conclusion about the absence of contraindications to surgical treatment.
Valid for 10 days:
- A smear to determine the degree of vaginal cleanliness (if infections and inflammation are detected, treatment is indicated).
Based on the results of the preoperative examination, a second consultation is carried out, the date of the operation and preoperative preparation are set.
Preparation for surgical treatment
- Stop sexual intercourse two days before surgery.
- The day before, cut or shave the hair on the pubic area, labia and perineum.
- On the eve of the intervention, go to bed no later than 22:00. You can take a sedative: tinctures of motherwort, peony, valerian, etc., according to the instructions included with the medications.
- In the morning, on the day of surgery, empty your bowels, take a shower and thoroughly clean the external genitalia, and put on clean knitted underwear.
- Hunger – last meal three hours before surgery.
- Immediately before the procedure, empty your bladder.
- HAVE WITH YOU:
- Referral for surgery, examination results (ultrasound and tests).
- A clean shirt (robe) and socks, sanitary pads, slippers. Leave jewelry (earrings, rings, etc.) at home.
Recommendations after perineoplasty
To achieve the best effect, in the postoperative period the woman must
observe a number of prohibitions and doctor’s prescriptions. They are determined by the anatomical features of the intervention area, the timing of tissue healing and the resorption of suture materials.
- Do not sit on the crotch for 3 weeks;
- Avoid sports, running, and heavy physical labor for 2 months;
- Avoid sexual activity for 2 months;
- Toilet the external genitalia at least 2 times a day;
- Avoid excessive and prolonged increases in intra-abdominal pressure (do not push or lift heavy objects).
Back to contents
How is the procedure carried out at Polyclinic+1?
Perineoplasty does not require hospitalization. The procedure takes place in a gynecological chair and takes only a few minutes. After the consultation, the doctor will determine how much of the drug you need to administer. Typically 1 to 3 ml is used. The gel is injected with ultra-thin syringes and, as a rule, the injections do not cause discomfort, but if you wish, the perineal area can be numbed. Perineoplasty has no complications, so you can immediately return to your normal life. The effect lasts from 6 to 18 months, depending on your individual characteristics, after which the procedure can be repeated.
Conservative treatment methods
Conservative methods include: pelvic floor muscle training, physiotherapy, hormonal therapy.
Pelvic floor muscle training
Various exercises to strengthen the pelvic floor muscles can be easily found on the Internet. For muscle training, various stationary and portable myostimulators—vaginal simulators—are widely used (Fig. 8).
Training the pelvic floor muscles is possible only after restoration of the normal anatomy of the perineum, i.e. after perineoplasty. Any damage to the pelvic diaphragm must be eliminated before training the pelvic floor muscles! Otherwise, the situation will only get worse.
Video 2.
Exercises to strengthen the pelvic muscles
Rice. 8.
Vaginal simulators
Physiotherapy
There are various methods of influencing the vaginal walls and underlying tissues with physical factors (laser, magnetic field, etc.). Physiotherapy improves blood supply and metabolic processes in muscle tissue (to accelerate regeneration), has an anti-inflammatory effect, and is prescribed in combination with other conservative techniques.
Hormone replacement therapy
Hormonal drugs are prescribed for a deficiency of sex hormones in the body (age-related and surgical menopause, infantilism). These can be tablets for oral administration and dosage forms for topical use (creams, ointments, suppositories). Self-prescription of hormones, without prior examination of the body’s condition, is UNACCEPTABLE!!!
Back to contents