Types of Microtia
Type 1 The first type of microtia - the mild type - is characterized by an unusually small ear, while the ear canal is unchanged or significantly narrowed.
Type 2 The second type of microtia is characterized by a significant degree of deformation of the auricle, usually in the upper half of the ear, often accompanied by stenosis or absence of the ear canal.
Type 3 Type 3 is the most common form of microtia. The outer ear is represented by a small rudiment. The auditory canal is often absent.
Type 4 The fourth type of microtia is also known as anotia. It is characterized by the almost complete absence of the outer ear and auditory canal.
What causes Microtia?
Scientists are still not sure of the causes of microtia, and do not know for sure whether this pathology has a connection with pregnancy
.
Many parents are concerned that there is a lack of information on how to prevent microtia in a child. Moreover, it has been proven that this anomaly is not transmitted genetically. Microtia also cannot be detected
before the baby is born, even with prenatal ultrasound.
Microtia occurs in about one in 5,000 babies born in the United States. But in other regions, especially China, South America, Central America, Russia, Kazakhstan, statistics are at a higher level.
But, even if you are located in another part of the world, you can use the services of prof. Zilberstein in Israel.
Professor Silberstein Why choose Professor Silberstein for ear reconstruction surgery for your child?
World-renowned surgeon Professor Zilberstein is a highly qualified plastic surgeon who is the only one in Israel who specializes in auricular reconstruction using the Medpor method.
Education
- Faculty of Medicine, David Ben-Gurion University of the Negev, Israel
- Residency in Medicine, Be'er Sheva, Israel
- Internship on the use of the Medpor method at Harvard University, Boston, USA
Professor Eldad Zilberstein is a popular lecturer at David Ben-Gurion University. In addition to his busy clinical work, Prof. Zilberstein is actively involved in scientific activities. He is the author of numerous articles on plastic surgery published in leading international medical journals.
Membership in associations
- Israeli Association of Plastic Surgery (ISAPS)
- American Association of Plastic Surgery (ASPS)
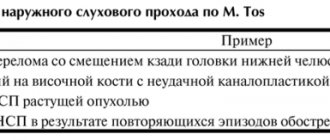
Classification
Pathology can be of varying degrees of severity:
- 1st degree: the ear canal may be of normal size or narrowed, the auricle is reduced in size, some of its elements, such as the tragus or antitragus, may be missing;
- 2nd degree: the ear canal is narrowed or completely absent, the auricle is underdeveloped, deformed;
- 3rd degree: usually the ear canal is closed, and in place of the auricle there is a fold of skin devoid of cartilage;
- Grade 4: The outer ear is completely absent.
What else do you need to know about microtia?
Many patients with microtia also have atresia. Atresia is characterized by narrowing or absence of the ear canal. In a normally developed hearing system, sound waves travel through the ear canal. They create vibrations in the eardrum, ossicles, and fluid in the inner ear. The brain receives these vibrations in the form of electrical impulses, which it translates as sounds. When sound waves are unable to travel down the ear canal normally, patients often have difficulty distinguishing individual sounds from background noise. As a result, atresia in children may also contribute to stuttering, language difficulties, and difficulty socializing the child.
How to treat microtia and atresia?
Medical correction of conditions due to abnormal development of the auricle should be divided into two problems - the problem of hearing and the problem of appearance.
The scope of necessary actions depends on the degree of impairment of the formation of the hearing organ. The actual functional assessment—the performance of the ear—can be assessed by audiologists, even at a fairly early stage. The method of studying auditory evoked potentials - AES - makes it possible to understand whether the auditory nerve is alive, and is it possible in principle to make a child hear?
The second step is morphology assessment. Computer multislice X-ray tomography allows you to build a very accurate, with a resolution of a fraction of a millimeter, three-dimensional picture of the bone, cartilage and soft tissue structures of the temporal bone area. On the tomogram it will be clear which part of the ear structures has not formed, in what condition the structures of the middle ear are - the auditory ossicles and the eardrum, which fills the area in which the ear canal should be located - bone or soft tissue formations. These data make it possible to understand, firstly, how promising the attempt to form the ear canal is from a functional point of view, and secondly, to determine landmarks that allow the surgeon to accurately enter the area of the tympanic cavity - the place where the preparation of sound for transmission to the auditory nerve should end. Essentially, these two studies determine how much work it makes sense to do from an objective standpoint. Based on the same data, you can understand how many steps will need to be completed and what result can be achieved.
So, what effect is even possible ? Ideally, we aim to give a child a true, complete ear that will look like an ear, hear like an ear, and behave like an ear throughout the child's life. The path to achieving this goal lasts for several years, several stages of reconstructive surgery are performed, as a result of which we must restore the ear canal, eardrum and appearance of the ear.
The latter, in fact, is almost the smallest problem on the entire list. It’s just that the outer ear is the most noticeable component of the entire complex.
Let's consider the most promising option. The child has a formed tympanic cavity, there are auditory ossicles and a living auditory nerve, but the ear canal is completely closed and the auricle is missing or incorrectly formed. This is the classic combination of auditory canal atresia and microtia.
First and foremost, the child needs to improve his hearing. This is done with the help of early prosthetics with special bone conduction hearing aids, special devices that transmit sound to the auditory nerve bypassing the ear, causing the skull bone to resonate, usually through a special metal pin - an anchor, which is implanted into the bone. Regardless of your desire to restore the child’s normal anatomy, a hearing aid must be installed as early as possible; this will be the key to the child’s adaptation to society and will significantly facilitate rehabilitation in the postoperative period. From zero to three or four years of age, audiologists and teachers of the deaf should definitely work with the child. As the structure of the temporal bone and ear grows, they reach the state in which they must remain for almost their entire life. This period lasts until the third or fourth year of life. Once the formation of the area is completed - we can evaluate this from the tomogram - we can begin the surgical stage. The first operation performed is the formation of a bone canal. A complex and painstaking operation, which carries the greatest number of risks of complications, is performed taking into account knowledge about the microanatomy of the area obtained from tomography, often using special navigation tools that “link” the position of the doctor’s instrument to the reconstructed three-dimensional image on the monitor. This is the most high-tech stage of the operation. Precisely because there are serious risks at this stage, we must approach the justification for completing this stage with all possible responsibility. If there are no auditory ossicles and, moreover, the auditory nerve is fully functional, this stage is not recommended.
But here's the dilemma. The optimal period for the formation of a bone canal is about 4 years, and we begin to make the auricle only at 7-8 years. Therefore, after drilling a channel in the bone, we do not open it outward, but fill it with a silicone cylinder. This cylinder rests on the preserved part of the bones at one end, and is located under the skin at the other. It does two things. Firstly, already at this stage, hearing improves noticeably without a device. Secondly, this cylinder is a kind of protector that does not allow bone tissue to close the defect. The area between the cylinder and the surface of the drilled bone is filled with granulations - loops of small vessels. These granulations then become a bed for the transplanted skin, which will line the ear canal, and ensure rapid and accurate engraftment of the displaced skin fragment.
The next step is the formation and implantation of the auricle frame. This stage is performed at the age of 6−7 years. The ear frame can be the child’s own cartilage, taken from the costal arch, or a ready-made silicone frame made from Medpor material. Each option has its own advantages and disadvantages.
The Medpor frame is supplied preformed, molded, sterilized and ready for transplantation. Therefore, all we need is to prepare a bed for the prosthetic frame and transplant it under the skin. It sounds simple, but it’s also simple to do. Where are the cons? First of all, the silicone frame is a factory-made finished product. Therefore, the number of ear designs is limited. The ear created in this way will usually be different in appearance from the other ear with unilateral microtia. Thousands and thousands of children who have Medpor installed have exactly the same ears.
In addition, we do not yet have long-term results of such an operation. There may be difficulties with long-term effects. Over time, such an ear can change, lose shape, or move - like any silicone prosthesis. Unfortunately, the method has not been used for very long, and there is no complete characterization of long-term results yet. In addition, the absence of a living “substrate” can lead to disruption of nutrition, innervation and disruption of the sensitivity of the skin over the defect.
The option with cartilage is more time-consuming and somewhat more traumatic - an incision is required to remove a fragment of the costal arch - but it has its advantages. Unlike a factory artificial frame, an ear made of cartilage changes in shape over time, matures, the skin on it, adapted from a flap on the head, matches the appearance of the surrounding skin, innervation is preserved, and cartilage tissue serves as a conductor for vascular growth. The ear turns red when the patient is ashamed and turns pale when it is cold. The ear feels touch. The ear behaves like an ear - this is one of the points we want to achieve when performing correction, and this is one of the main differences between the cartilage framework method and the Medpor method. The second advantage is that in case of a unilateral malformation of the auricle, the formed ear can be made absolutely the same as the existing one. Therefore, despite the high labor intensity and long duration of the process, we consider it preferable to form a cartilaginous frame. Although in a number of cases we use Medpor, according to indications, this is done when we anticipate great technical difficulties, when there is a deficiency of tissue, inelastic skin in the area, since this method is less demanding. And of course, since we are talking about cosmetics, we use the technique in cases where the patient himself desires it.
The final stage of ear restoration is the “opening” of the ear canal. This stage is quite demanding on the condition of tissues, elasticity and skin reserve. It is performed when the outer frame is fully formed, the surrounding tissues have taken root and the ear has acquired its natural appearance. In some cases, opening the ear canal is not recommended, for example, when the deformation of the area has led to a significant displacement of the middle ear from its normal position. In this case, the opening of the ear canal indicates a pronounced defect in the aesthetics of the final result. Even if you do not open the previously formed ear canal, the silicone “sound guide” installed at the first stage allows you to achieve a very noticeable, usually over 60%, increase in hearing. Also, there is no point in opening the ear canal if the middle ear is not formed or does not hear due to a defect in the auditory nerve. In such situations, a relatively small depression is made - a fold in the tissue, which carries only an aesthetic load.
Thus, a set of surgical measures makes it possible to create not only aesthetics and appearance, but also, in a large number of cases, to give the child a fully functioning hearing organ. This, ultimately, is our main goal every time we start working with each child.
Other abnormalities associated with microtia
All children with microtia have either ear canal atresia or ear canal stenosis. Stenosis - characterized by a narrowing of the ear canal and a small eardrum. With any type of atresia or stenosis, the ability to transmit sound to the inner ear is hampered and leads to significant hearing loss. While all children with microtia have auditory atresia or stenosis, not all children with auricular atresia or stenosis have microtia. When a baby is born with microtia, it is usually an additional abnormality. The vast majority of children with microtia have no other abnormalities.
In rare cases, microtia is accompanied by other abnormalities as part of the syndrome. The most common abnormality associated with microtia is hemifacial microsomia. With this anomaly, both halves of the face develop disproportionately. The degree of hemifacial microsomia varies from barely noticeable (most common) to very noticeable (less common).
Treacher Collins syndrome is characterized by the presence of both ears. The cheekbones are small, and there is damage to the eyelids and lower jaw.
Goldenhar syndrome may involve the presence of developed one or both ears with incomplete development of the nose, soft palate, lips and jaw. These children often have a bone disorder in the neck as well as a benign tumor of the eye. There are other, less common syndromes that may accompany microtia.
Surgery to restore the auricle and hearing functions for microtia
Microtia II degree Stages of auricle reconstruction
Due to the fact that microtia is usually combined with conductive hearing loss, and sometimes occurs in combination with the sensorineural form, reconstructive operations are a rather complex problem and are planned by a plastic surgeon together with an otolaryngologist. Doctors of these specialties determine the age of the child for surgical intervention, as well as surgical methods, stages and sequence of surgical treatment.
Compared to eliminating a cosmetic defect, restoring hearing in the presence of concomitant atresia is a higher priority. Children's age significantly complicates diagnostic studies. However, if there are visible congenital defects in a child at an early age, the hearing function is first examined using objective methods such as registration of evoked otoacoustic emissions, acoustic impedance measurements, etc.
In children over four years of age, the diagnosis of hearing acuity is determined by the degree of perception of intelligible spoken and whispered speech, as well as through threshold audiometry.
In addition, a computed tomography scan of the temporal bone is performed to detail the existing anatomical disorders.
Determining the age for reconstructive surgery in children also poses a certain difficulty, since tissue growth can change the results obtained in the form of complete closure of the external auditory canal and/or displacement of the auricle.
At the same time, late hearing prosthetics, even with unilateral hearing loss, leads to delayed speech development of the child, difficulties in school learning, psychological and behavioral problems and, in addition, no longer brings significant benefits in terms of hearing restoration. Therefore, surgical intervention is usually planned individually for ages 6 to 11 years. Before surgical restoration of hearing function, especially in cases of bilateral hearing loss, for the purpose of normal speech development, it is recommended to use a hearing aid based on the perception of sound bone vibration, and in the case of the presence of an external auditory canal, a standard hearing aid.
Microtia: Treatment Options
If you are looking for the most effective microtia treatment for your child, you always have several options.
- Cartilaginous reconstruction from the rib is the oldest method. Reconstruction using pectoral cartilage has been the traditional method of reconstruction for the past 55 years. It involves taking a piece of cartilage from the patient's rib to form the frame of the outer ear. This is a multi-stage operation, quite painful for the patient and requiring a long stay in the clinic.
In Israel, Professor Duvdevani has the most experience in carrying out this type of reconstruction.
- A more modern and less traumatic method for the child is reconstruction of the auricle using MEDPOR material.
Medpor porous polyethylene implants provide surgeons with a wide range of reconstruction options. MEDPOR is a biocompatible porous material based on polyethylene. The interconnected and omnidirectional pore structure allows the growth of fibrovascular tissue and fusion with the patient's tissues.
Risk of development and provoking factors
Science cannot accurately explain the reasons why an embryo develops such a deviation, however, in some cases, the anomaly becomes the cause of a genetic predisposition, rubella during pregnancy, poor lifestyle and the influence of teratogenic factors on a woman during gestation.
Drinking alcohol, smoking, staying in places of increased radiation and other harmful effects during pregnancy increases the risk of developing not only microtia, but also other anomalies in the development of internal organs and tissues.
What to expect after reconstruction?
Microtia - result 6 months after surgery
During the Medpor operation, the ear is initially made to “grow”, approximately 10-15% larger than a healthy one. So that in adulthood the sizes of both ears are equal. The ear is literally constructed from an implant to mirror the second ear. The recovery process takes several months, and the final result is visible 6 months after the operation. The operation takes place in one stage and its duration is 5-6 hours.
Medpor is a porous implant; the interconnected and omnidirectional structure of the pores allows the growth of vascular-fibrous tissue and fusion with the patient’s tissues, thereby allowing the body not to perceive the implant as a foreign body. MEDPOR two-piece ear implants allow the height and projection of the helix to be sculpted to match the height and projection of the opposite ear. During the operation, the medpor is covered by the temporal fascia and then by the skin... so after healing, the new ear looks identical to a healthy ear.
For unilateral microtia and atresia, is hearing surgery necessary if my child is developing normally? Will unilateral atresia affect my child's speech development?
Children with unilateral microtia and atresia will have trouble finding the direction of the sound source and experience discomfort in noisy environments. However, the need for hearing restoration or BAHA placement is controversial. When a child with this problem goes to school, you must ensure that the child is given the best placement that will allow him to hear the teacher better. If your child has microtia with hearing loss on both sides, it is important to improve hearing with a bone conduction hearing aid such as BAHA. It must be installed before 6 months of age. The sounds that children hear in the first year of life are very important for the development of speech and language.
At what age is it better to have surgery?
Currently, there are techniques that allow reconstruction of an underdeveloped auricle as early as 1.5-2 years. But it is often recommended to carry out such an operation no earlier than 5-6 years, since as the child grows, the formed auricle may lose symmetry and lag behind in growth. If a child notices that he is different from other children and is worried about this, then the operation can be done a year before school.
What is reconstructive rhinoplasty and how is the operation performed?
How to perform gluteoplasty - surgery to enlarge the buttocks with implants, read the link.
Find out what the consequences may be after otoplasty here.
What additional specialists may be needed?
For children with different types of microtia, the following specialists may be needed:
- A craniofacial plastic surgeon who provides information on mandibular reconstruction in the presence of associated syndromes.
- An ENT surgeon who specializes in hearing problems. His job will be to determine if your child is a candidate for ear canal reconstruction. Depending on what treatment you decide for your child, you may need a canal made before, or in some cases during, ear reconstruction.
- Geneticist
Disease prognosis
Modern medicine is advancing by leaps and bounds, and every year the chances of a favorable outcome of the disease increase. The development of scientific and technological progress makes it possible to easily shape the auricle and restore auditory function in cases of mild to moderate disease, as well as successfully perform plastic surgery in cases of severe microtia disease, as well as in cases of anotia.
Russia's leading ENT surgeons proudly talk about their achievements in the treatment of the disease, and every year more and more young patients return to normal life.