Friday, April 2, 2021
There are many factors that influence the expansion of the vagina and the prolapse of its walls. As a result, the woman not only experiences discomfort along with painful sensations, she is deprived of the joys of sexual life and the opportunity to engage in even ordinary daily duties. As a result, the victim is left with only one thought - how to make the vagina smaller. This task does not belong to the series of impossible ones and is solved with the help of colporrhaphy. Below we will look at what it is, in what cases it is prescribed and why it may be contraindicated and other subtleties of the procedure.
Types of colporrhaphy
Colporrhaphy is a surgical procedure that changes the size of the vagina. Most often, problems with stretched vaginal walls, excessive width of the organ, prolapse, and urinary incontinence arise as a result of labor or age-related changes. Depending on the factors that caused the changes, the types of colporrhaphy are selected:
- Anterior colporrhaphy . This type of operation is a plastic transformation of the anterior vaginal wall. The intervention is prescribed for prolapse - prolapse - of the anterior wall of the organ, when it falls out simultaneously with the posterior wall of the bladder.
- Posterior colporrhaphy . Plastic surgery affects the posterior vaginal wall and becomes necessary when there is prolapse of the posterior portion of the organ, caused by insufficient tone of the pelvic floor tissues or ruptures formed during labor. Such intervention may become necessary if there is a threat of uterine prolapse or if there is a hernia in the rectum.
- Median colporrhaphy . Most often, surgery is prescribed for final organ loss in older women who are not sexually active. This approach is based on possible complications of the operation - the consequence may be the impossibility of sexual intercourse and loss of access to the uterine cervix for examinations. A prerequisite is a preliminary examination to exclude a predisposition to cervical cancer.
When prescribing colporrhaphy, they are guided by secondary changes associated with prolapse of the vaginal walls, both anatomical and functional. For the most part, the decision to undergo surgical intervention is based on the development of complications in adjacent organs.
Important. For first-degree vaginal prolapse, surgery is not an immutable solution; conservative treatment can be prescribed, based on special gymnastic exercises to strengthen the muscular system of the vaginal area and pelvic floor.
Anterior colporrhaphy
Anterior colporrhaphy is plastic surgery of the anterior vaginal wall.
Indications for anterior colporrhaphy:
- Prolapse of the anterior vaginal wall
- Prolapse and prolapse of the anterior vaginal wall along with the posterior wall of the bladder
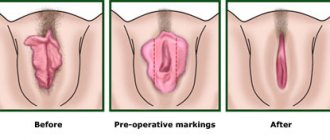
Anterior colporrhaphy surgery technique:
- An extra section of mucous membrane is isolated on the anterior wall of the vagina
- This area is excised
- Deep sutures are applied
- A continuous suture connects the edges of the vaginal mucosa
Indications for colporrhaphy
Kegel exercises do not have the desired effect in the second and third degrees of pathology, accordingly, surgical intervention becomes a reasonable necessity. In addition to the reasons listed above, indications for organ plastic surgery occur when:
- Urinary incontinence caused by a displaced urethra, excessive stretching of its mouth.
- Gas incontinence due to incompetence of the anal sphincter due to a displaced rectum, which occurs as a result of prolapse of the posterior vaginal wall.
- Difficult or uncomfortable defecation, despite the fact that there is no constipation as such.
- Pain during physical exertion, intercourse, which is explained by the unstable position of the organs of the genitourinary system.
In addition to all of the above, plastic surgery can be performed at the patient’s request even in the absence of organ prolapse. A fairly common reason is the deteriorated quality of sexual relations after childbirth; in some cases, surgery is required in the presence of anatomical features, when partners have a discrepancy in the size of the genital organs. Surgery may also be required for patients who are not satisfied with the aesthetic appearance of an enlarged vaginal slit, even to the point of gaping, which is usually observed in those who have given birth multiple times.
Preparing for colporrhaphy
Preparation for surgery does not depend on the type of colporrhaphy performed. It is influenced only by the characteristics of a particular woman’s body, which require additional diagnostics. The examination allows you to identify diseases that are a contraindication to vaginal plastic surgery.
First, a gynecological examination is performed, during which the doctor asks about existing complaints and determines the tactics of intervention. Smears are taken from the vagina, urethra and cervix for flora, sexually transmitted infections, cancer and precancerous diseases. In case of displacement of the bladder and rectum, accompanied by a violation of its function, the woman is additionally consulted by a urologist and proctologist.
Gynecological smear
The patient undergoes tests:
- General blood and urine tests.
- Blood for HIV, hepatitis BC, syphilis.
- Blood for clotting time and bleeding duration.
- Biochemical blood tests.
Blood type and Rh factor are donated if a woman does not have information about them confirmed by an official document.
The patient undergoes fluorography and does an ECG. If necessary, a pelvic ultrasound, additional tests, consultations with specialists and other studies may be prescribed to clarify the state of health.
Contraindications for surgery
Unfortunately, in some cases, medical indications and the wishes of the patient themselves do not play a role, since there are a number of contraindications to plastic surgery. General prohibitions are very similar to restrictions when performing any surgical intervention for which general anesthesia is used. This list includes:
- Complicated decompensated somatic pathologies in which damage affects the vascular system, kidneys, heart muscle and liver.
- The presence of infectious diseases in acute form.
- Development of acute thrombophlebitis.
- Clearly impaired blood clotting.
- Recovery period (acute or early) after a heart attack or stroke.
- In case of a dangerous combination of various injuries.
- During the postpartum period.
- Plastic surgery is not advisable in the case of the formation of malignant pathology and in the presence of diseases that are transmitted through sexual contact.
There are also relative contraindications, which include age. Colporrhaphy is not indicated for patients under 18 years of age, but such a prohibition applies only to situations where the changes performed are of an aesthetic nature. If the reason for the operation is abnormalities that interfere with the functionality of the organs, or there are medical prescriptions for changes, the intervention is carried out regardless of age.
Contraindications
The list of contraindications to colporrhaphy includes:
- Acute inflammation . Due to the risk of spreading infection, intervention is not performed for colpitis, endometritis, adnexitis, and other inflammatory diseases of the pelvis and other organs.
- Decompensated systemic pathologies . Due to the high probability of vascular complications, colporrhaphy is not performed in cases of uncontrolled severe diabetes mellitus, decompensated arterial hypertension, or blood clotting disorders.
- Pregnancy . Colporrhaphy is not performed on pregnant women due to subsequent tissue stretching during childbirth. A relative contraindication is planning a pregnancy; the operation is postponed for several months after the end of the postpartum period.
Technique of the operation
Colporrhaphy is carried out exclusively in a hospital; before the operation itself, it is necessary to conduct a comprehensive examination aimed at identifying contraindications and clarifying existing disorders. The patient is hospitalized several days before surgery. Preoperative preparation, in addition to examination, includes preventive measures aimed at cleansing the intestines and vaginal sanitation. On the eve of the operation, if necessary, the patient should review the menu - food should be well digestible and fairly light. The last meal and liquid intake is allowed 12 hours before surgery, taking into account the need for general anesthesia. As for the treatment technique, any manipulations during surgery are performed vaginally:
- The cervix is fixed with special clamps and moved to the side.
- Excision of the vaginal walls is performed.
- In this case, a diamond-shaped flap is isolated, and the underlying muscle tissue is sutured and fixed.
- The position of the incision depends on the type of intervention prescribed.
- After the main stage of the procedure is completed, layer-by-layer suturing begins.
- Separate sutures are placed on the muscle tissue and fascia, which dissolve over time.
- The mucous layer is closed with a continuous suture.
- To avoid the formation of “pockets”, the surgeon has to exercise strict control over the position of the wound edges.
- To prevent the formation of rough scars, it is necessary to exclude the appearance of deformations in the seam area in the form of rollers.
- If a median colporrhaphy is performed, sutures are placed simultaneously on the back and front walls to connect them, forming two channels on the sides intended for removing uterine secretions.
The final stage of the operation is draining the vagina, followed by treating the walls of the organ with alcohol. Then a tampon soaked in disinfectant ointment, most often Synthomycin emulsion, is inserted into the vagina. The accumulated urine is removed using a catheter.
Posterior colporrhaphy
Posterior colporrhaphy (colpoperineorrhaphy) is plastic surgery of the posterior vaginal wall.
Indications for posterior colporrhaphy:
- Prolapse and prolapse of the posterior wall of the vagina, caused by ruptures of the perineum (during childbirth), decreased tone of the peripelvic tissues
- Threat of uterine prolapse
- Rectal hernias
Posterior colporrhaphy surgery technique:
- A triangle is separated on the back wall of the vagina
- Within this triangle, the mucous membrane is cut off
- The levators are exposed and connected with catgut sutures
- Several separate stitches are placed between them
- The membrane of the posterior surface of the vagina is sutured with a continuous suture.
Carrying out colporrhaphy
Colporrhaphy is a surgical procedure performed on the vaginal wall to correct defects including cystocele (prolapse of the bladder) and rectocele (protrusion of the anterior wall of the rectum). Colporrhaphy can be performed on the anterior and/or posterior walls of the vagina. Anterior colporrhaphy is performed for cystocele or urethrocele, while posterior colporrhaphy is used for rectocele. The price for anterior and posterior colporrhaphy is practically the same. The main reason for prescribing colporrhaphy is prolapse. Prolapse is any protrusion of an organ or a specific part of it, in this case through the vagina. At the slightest suspicion of prolapse, you must make an appointment with a specialist. The pelvic organs usually have tissue (muscles, ligaments, etc.) that help hold them in place. Several factors can cause these tissues to weaken, leading to organ prolapse. A cystocele is defined as a protrusion or prolapse of the bladder into the vagina; Urethrocele - prolapse of the urethra. A rectocele occurs when the rectum bulges out. It is caused by a defect in the rectovaginal fascia. When part of the small intestine bulges into the vagina, the condition is called enterocele. Uterine prolapse occurs when the uterus moves downward. Vaginal wall surgery is usually not prescribed unless symptoms of prolapse begin to interfere with daily life.
Make an appointment for a consultation Vaginal surgeries are surgeries performed on the external and internal genitalia through an incision in the vagina. Indications for operations see Vaginal wall prolapse, Bartholin gland cyst Before operations, standard preparation is carried out. For more information about preparing for surgery, see Preoperative preparation. These operations can be performed under intravenous, infiltrative or spinal anesthesia using modern drugs that ensure the absence of side effects after anesthesia. The patient sits on the operating table in the form of a gynecological chair. The doctor inserts a Foley catheter into the patient's bladder to empty it, after which the medical staff treats the surgical field with a special solution. The gynecologist surgeon performs the main stage of one of the above operations after the anesthesia has taken effect, so the most unpleasant moment is the installation of an IV; all other manipulations are carried out during anesthesia sleep. Vaginal hysterectomy or extirpation is an operation to remove the uterus through the vagina. This operation guarantees complete cure and prevention of any uterine disease. A hysterectomy involves removing the cervix and, in some cases, one or both ovaries and fallopian tubes. The main advantages of vaginal hysterectomy compared to abdominal hysterectomy are minimal trauma, good cosmetic effect, the possibility of spinal anesthesia, early discharge and a short rehabilitation period. After vaginal surgery, the wounds are sutured using self-absorbing threads. Depending on the complexity of the operation, the hospital period lasts from 2 hours to 1 day, after which the patient is discharged and can go home. Rehabilitation after vaginal surgery takes from 10 to 30 days and is carried out under the supervision of the operating doctor. After the operation, it is not recommended to sit down for 7 to 10 days and have sexual activity for a month. Full recovery occurs 2 months after surgery. Indications for hysterectomy: • uterine fibroids in combination with severe cervical dysplasia; • uterine fibroids in combination with uterine bleeding; • severe adenomyosis; • cervical cancer in combination with prolapse; • complete or incomplete uterine prolapse; • atypical endometrial hyperplasia. Bloodlessly and carefully, the gynecologist surgeon dissects the ligaments that support the uterus and carefully coagulates the bleeding vessels with a special instrument. The surgeon sutures large vessels that supply blood to the uterus, separates it from the surrounding tissues, removes it and removes it from the abdominal cavity through the vagina. The vagina is sutured with absorbable sutures. After this, posterior colporrhaphy is most often performed. The surgical method is selected by the surgeon individually for each patient and depends on the nature of the pathology, the reasons for changes in the vaginal walls, the age of the patient being operated on, her wishes, the presence of changes in the uterus, rectum, and bladder. Anterior colporrhaphy is a surgical correction of the anterior vaginal wall. The main indication for anterior vaginoplasty is cystocele, that is, a hernial protrusion of the bladder wall in the area of the anterior vaginal wall. Colporrhaphy is plastic surgery of the vaginal walls. Depending on the technical features of colporrhaphy, there are several options for the operation: 1. Anterior colporrhaphy. 2. Posterior colporrhaphy with levatoroplasty. 3. Median colporrhaphy. Operations performed: • transvaginal hysterectomy (hysterectomy); • colporrhaphy and levatoroplasty: • anterior colporrhaphy; • posterior colporrhaphy with levatoroplasty; • median colporrhaphy. • Manchester operation; • removal of Bartholin gland cyst; • marsupialization of Bartholin gland abscess; • installation of a word catheter. Transvaginal hysterectomy Colporrhaphy Manchester operation Removal of Bartholin gland cyst
Installation of a word catheter (word catheter) VAGINAL OPERATIONS Vaginal operations Transvaginal hysterectomy Colporrhaphy Bloodlessly and carefully, the gynecologist surgeon cuts out an oval flap of the mucous membrane, which is a hernial protrusion from the area of bulging of the anterior vaginal wall. The bladder wall is immersed using absorbable sutures using various techniques. In some cases, a polypropylene mesh is fixed in the area of the surgical wound. The edges of the vaginal mucosa are sutured with absorbable sutures.
Often, levatoroplasty and perineorrhaphy (perineal plastic surgery) are performed together with posterior colporrhaphy. In addition, posterior colporrhaphy is often combined with anterior colporrhaphy. After the anesthesia has taken effect, the gynecologist surgeon cuts out a triangular flap of excess tissue from the back wall of the vagina. Then the doctor restores and tightens the pelvic floor muscles. The next stage is perineal plastic surgery, during which old scar tissue is removed and the entrance to the vagina is narrowed. Often, levatoroplasty and perineorrhaphy (perineal plastic surgery) are performed together with posterior colporrhaphy. In addition, posterior colporrhaphy is often combined with anterior colporrhaphy. After the anesthesia has taken effect, the gynecologist surgeon cuts out a triangular flap of excess tissue from the back wall of the vagina. Then the doctor restores and tightens the pelvic floor muscles. The next stage is perineal plastic surgery, during which old scar tissue is removed and the entrance to the vagina is narrowed. Posterior colporrhaphy is a surgical correction of the posterior vaginal wall. The main indication for posterior colporrhaphy is rectocele, that is, a hernial protrusion of the rectal wall in the area of the posterior vaginal wall. Rectocele usually occurs due to decreased tone of the muscular frame of the pelvis and traumatic injuries to the vagina and perineum during childbirth. Median colporrhaphy is a surgical correction of the anterior and posterior walls of the vagina. Features of median colporrhaphy: • recommended for patients over 75 years of age; • the operation excludes the possibility of sexual activity; • contraindicated in case of pathologies of the cervix, since after the operation a visual examination will be impossible. Manchester operation Posterior colporrhaphy Median colporrhaphy
Indications for Manchester surgery are prolapse and partial prolapse of the uterus in combination with an elongated cervix and cystocele. Since amputation of the cervix often excludes pregnancy, the operation is not recommended for women of childbearing age. Before the Manchester operation, the cervical canal is dilated and a diagnostic curettage of the uterine mucosa is performed to exclude a malignant tumor. The Manchester operation is an operation that combines amputation of the elongated cervix and anterior colporrhaphy, as well as suturing of the cardinal ligaments to the anterior wall of the cervix and colpoperineoplasty.
Before the Manchester operation, the cervical canal is dilated and a diagnostic curettage of the uterine mucosa is performed to exclude a malignant tumor. Bloodlessly and carefully, the gynecologist surgeon, in the case of elongation (lengthening) of the cervix, removes part of the cervix with strengthening of the ligamentous apparatus. Then the surgeon performs plastic surgery of the anterior and posterior walls of the vagina, tightening the pelvic floor muscles, as well as plastic surgery of the perineum, during which old scar tissue is removed and the entrance to the vagina is narrowed. Removal of Bartholin gland cyst
The main advantage of the radical method of removing the Bartholin gland cyst is only one thing – the absence of relapses. This operation is quite traumatic and requires a long period of rehabilitation. Despite its simplicity, surgery to remove a Bartholin gland cyst requires the surgeon to have appropriate qualifications, patience and accuracy.
The technique was developed in the USA about 50 years ago and today is the main method of treating Bartholin gland cysts there. Treatment by installing a word catheter is low-traumatic and bloodless, but does not exclude the possibility of relapse, the likelihood of which is very low. Therefore, an individual examination and treatment program is developed for each patient. The operation is performed under intravenous anesthesia. After the anesthesia has taken effect, the gynecologist-surgeon carefully treats the surgical area and makes an incision in the area of maximum protrusion of the cyst, at the border of the mucous membrane and the skin. The cyst capsule is carefully separated from the surrounding tissue. Healthy tissue of the gland is minimally injured - during the operation only the cystic formation is removed. The external genitalia are very well supplied with blood, so bleeding vessels are carefully coagulated and sutured. The operation is low-traumatic, performed under local or intravenous anesthesia and is completely painless. After the anesthesia has taken effect, a mucosal incision of about 3 mm in length is made in the projection of the cyst in the area of the exit of the Bartholin gland duct. The contents are aspirated and the cyst cavity is washed with an antiseptic solution. The cyst bed is sutured with absorbable sutures. The operation is completed by suturing. The removed cyst is sent for histological examination. Discharge from the hospital after removal of a Bartholin gland cyst is carried out on the first day. The recovery period lasts from 10 to 30 days. Installation of a word catheter (word catheter)
What is a Ward catheter? This is a silicone sterile tube 55 mm long and 5 mm in diameter, inside of which there is a channel with thin walls at the end. Depending on the size of the cyst, 2 to 3 ml of physiological solution of 0.9% sodium chloride is injected into the lumen of the canal; the ball at the end of the catheter is inflated and fills the cyst cavity.
Two absorbable sutures are placed at the edges of the incision to prevent the catheter from falling out. The free end of the catheter is inserted into the vagina.
The operation is performed at the patient’s request under local or intravenous anesthesia and is completely painless. The duration of the operation is about 30 minutes. After the anesthesia has taken effect, a small incision is made in the projection of the cyst at the border of the mucous membrane, the contents of the cyst are removed, and the cavity is washed with an antiseptic solution. The wall of the cyst is sutured to the mucous membrane of the labia with separate absorbable sutures; the cavity of the cyst remains open. After 1-2 hours the patient is discharged from the hospital. In the first days after installation of the catheter, a woman may experience slight discomfort. The catheter remains in the cyst cavity for six weeks. The only restriction is refusal to have sex. During this time, epithelization of the edges of the wound occurs and a new channel for the passage of secretions is formed. After 6 weeks, during an outpatient appointment, the liquid injected into the catheter is evacuated with a syringe, and it is painlessly removed; in the future, the catheter is practically not bothered, the only limitation is abstinence from sexual activity. Marsupialization of Bartholin gland cyst
Are you looking for a specialist to perform vaginal surgery? Carefully check the reputation of the chosen specialist: study his website and reviews on resources that inspire you with confidence. The Internet allows you to get all the necessary preliminary consultations with a gynecologist online.
Symptoms of prolapse
A small posterior prolapse may not cause signs or symptoms. Otherwise you may notice:
- A small bump of tissue that can sometimes protrude through the vaginal opening;
- Difficulty during bowel movements;
- Feeling of rectal pressure or fullness;
- A feeling that the rectum is not completely empty after a bowel movement;
- Problems during sexual intercourse (pain);
- Urinary incontinence (especially during physical activity);
- Back pain and difficulty urinating.
Often women are prescribed vaginal plastic surgery after childbirth. Factors associated with pelvic organ bulge include age, repeat childbirth, hormonal deficiency, current physical activity, and previous hysterectomy. Some women undergo vaginal tightening surgery not for medical reasons, but for aesthetic reasons.
Rehabilitation
The success of the operation largely depends on the correctness of the postoperative period after colporrhaphy. At the time of discharge from the clinic (on the 2nd day after surgery), the surgeon gives the patient extremely important recommendations for the recovery period after colporrhaphy:
- Avoid sex and sports for 2 months;
- Do not squat for up to 2 weeks (7 days – at a right angle);
- Douching with Chlorhexidine regularly;
- Take medications prescribed by the surgeon;
- Follow a diet that prevents constipation.
If you follow your doctor’s recommendations, rehabilitation after colporrhaphy is easy and without complications.
According to patient reviews, after colporrhaphy the quality of sexual life significantly increases, and the general physical and emotional state also improves. You can learn more about colporrhaphy and sign up for a free consultation and examination with Sarvar Bakirkhanov by calling.
Operation process
Before colporrhaphy surgery, the patient is given general or local anesthesia. A speculum is inserted into the vagina to keep it open during the procedure. An incision is then made in the vaginal skin and a defect in the underlying fascia is identified. The vaginal skin is separated from the fascia and the defect is folded and sutured. Any excess vaginal skin is removed and the incision is closed with stitches. Risks of colporrhaphy include potential complications associated with anesthesia, infection, bleeding, damage to other pelvic structures, dyspareunia (painful intercourse), recurrence of prolapse, and failure to correct the defect.
In most cases, colporrhaphy can be done without complications and the woman can resume normal activities, including sexual intercourse, approximately four weeks after the procedure. After successful intimate repair, symptoms associated with a cystocele or rectocele resolve, although separate therapy or intervention may be required to treat the incontinence. Anterior colporrhaphy has an approximately 66% success rate in repairing bladder prolapse.
After colporrhaphy
The length of stay in the department depends on the patient’s condition and the chosen surgical technique; in some cases, the patient is released for outpatient treatment a few hours after waking up from anesthesia. To improve hemodynamic parameters, drug therapy is carried out. Antibiotics are prescribed to prevent infectious complications.
A woman is recommended to observe sexual rest for 1.-1.5 months. You cannot sit on your buttocks for a week. When using self-absorbable suture material, removal of ligatures is not required; in other cases, the sutures are removed after 14 days.
More detailed information by phone or in one of our branches.
Preparation
A physical examination is required before colporrhaphy. Most often, to diagnose pelvic organ prolapse. A speculum is inserted into the vagina and the patient is asked to tense up or sit upright. The doctor then checks the front, back, top, and sides of the vagina for the presence of a bulge. In some cases, physical examination may not provide a definitive diagnosis. The patient should refrain from eating or drinking after midnight on the day of colporrhaphy. Your doctor may prescribe an enema the night before your procedure if you are having a posterior colporrhaphy. After surgery, the patient will be placed on a liquid diet until normal bowel function is restored. Your doctor will recommend that you avoid activities for several weeks that may put stress on the surgical site, including heavy lifting, coughing, long walks, sneezing, straining your bowels, and sexual intercourse.
Methodology
Posterior colporrhaphy is performed under epidural anesthesia or endotracheal anesthesia. The patient is placed on her back, shifted as far forward as possible (so that the buttocks protrude above the edge of the operating table) with her hips widely separated, which are fixed with leg holders (position for lithotomy). The external genitalia and inner thighs are treated with an alcohol-based antiseptic solution. The surgical field is fenced off with sterile linen. The labia minora are spread apart and fixed with interrupted sutures to the inner thighs.
To safely separate the flap, hydropreparation is performed by infiltrating saline into the submucosal layer. Posterior colporrhaphy begins with excision of a triangular-shaped flap of the posterior vaginal wall. The length and width of the flap are determined by the degree of prolapse and the size of the rectocele. The border between the skin of the perineum and the vaginal mucosa serves as the base of the triangular flap, and its apex is the posterior wall 2 cm below the cervix in the midline. In women who are sexually active, the restored size of the vaginal opening is made passable for two fingers.
The first stage of posterior colporrhaphy begins with clamping the area of the mucous membrane of the posterior vaginal wall and the skin of the perineum to be removed. Having pulled the edges of the vaginal wall with clamps, the surgeon separates the flap from the bottom up using a sharp and blunt method. After excision of excess tissue in the presence of a rectocele, the doctor’s further actions are aimed at restoring and strengthening defects in the deep spaces of the pelvic floor (levothroplasty).
The final stage of posterior colporrhaphy is the closure of the defect in the vaginal and perineal mucosa. The edges of the vaginal wound are often connected with continuous sutures using a self-absorbing thread. The edges of the skin of the perineum, together with the underlying tissues, are usually restored with separate silk or nylon sutures. After completing all stages of posterior colporrhaphy, the vagina is tamponed with a tight gauze swab, which is removed after a day. The average volume of intraoperative blood loss is 100-150 ml. The duration of the operation ranges from 30 to 60 minutes.
Registration for the procedure
Our clinic’s specialists will advise on all questions regarding the operation and help ensure the highest level of safety and comfort during colporrhaphy.
| Code | Our prices | Price |
| 02.43 | Anterior colporrhaphy | 150,000 rub. |
| 02.44 | Posterior colporrhaphy with levatoroplasty | 170,000 rub. |
When is colporrhaphy indicated?
Indications for vaginoplasty are as follows:
- congenital anomalies of the genital organs;
- loosening and atrophic change in tissues;
- prolapse, prolapse of the uterus;
- enuresis;
- low tone and elasticity of tissues;
- traumatic injury to the vagina.
The above problems may arise due to age-related changes, complications of inflammatory diseases, difficult childbirth, previous surgeries and other factors.
Colporrhaphy can improve the functioning of the genital organs and relieve problems with urination and gas incontinence. Thanks to vaginal plastic surgery, intimate life improves and sensitivity increases.
FAQ
What is the rehabilitation period after colpography?
— For the first 2-3 days after colporrhaphy, the patient remains in the hospital under the supervision of doctors. Then the woman can return home, but for another two weeks she is only allowed to take a horizontal position - sitting is strictly prohibited. The total rehabilitation period is 2 months.
Please tell me, with posterior colporrhaphy, will the suture in the vagina be up to the cervix or only 3-4 cm from the entrance?
— The suture in the vagina depends on the severity of the problem before surgery. The larger the problem, the longer the seam will be. Usually the suture is about 3-4 cm in size, but in each specific case it also depends on the degree of prolapse or stretching of the mucosa.
Ask a Question
Median colporrhaphy
This operation is performed for complete prolapse of the uterus, mainly only for older women who are no longer sexually active. Since the complications of median colporrhaphy are the inability to have sexual intercourse in the future and the lack of access to the cervix for examination. Therefore, before median colporrhaphy, an examination is required to exclude the patient’s predisposition to cervical cancer.
Technique of median colporrhaphy surgery:
- The anterior and posterior lips of the cervix are grabbed with forceps, removing them together with the vagina from the genital slit.
- Equal sections of the mucous membrane are cut off from the anterior and posterior walls of the vagina.
- Sutures are used to connect the front edges of the wound first, then the side and back edges.
- The cervix is immersed into the vagina.
- There are channels left and right for the outflow of secretions from the uterus.
When is vaginal plastic surgery performed?
When the walls of the vagina stretch and fall, complaints of discomfort in the vagina and the feeling of a foreign object may be disturbing. An increase in vaginal volume leads to a change in sexual sensations for the worse. Due to relaxation of the genital diaphragm, organs prolapse and urine leaks. A gaping genital slit contributes to disruption of the normal biocenosis of the vagina and frequent infection.
It is worth noting that it is not only childbirth that leads to vaginal stretching. The cause may be the consequences of severe injuries, chronic constipation, reduced levels of female sex hormones (in particular, estrogens), and a predominantly “sedentary” lifestyle.
The opposite situation happens: after suturing vaginal tears during childbirth or other gynecological operations, the scars deform its walls and a tightening effect is observed when the vagina is narrower than it should be. In such cases, plastic surgery is also indicated.