Scars and scars can seriously complicate the life of the most confident person in his own attractiveness. Skin damage that does not go away over time does not affect health - a person with traces of acne on the cheeks or with scars from abdominal surgery may have ideal tests and well-being - but they do affect psychology.
Scars attract attention, distinguish us from other people, and prevent us from enjoying our own reflection in the mirror or wearing revealing clothes. That is why at the Cleo Line clinic we use modern methods of laser and other therapy to get rid of scars and scars and restore the skin.
What are scars and scars?
Scars are connective skin tissue that forms after healing of burns, injuries, surgeries, and inflammatory processes. Varieties of scars also include stretch marks (striae) - narrow wavy stripes with grooves of atrophied tissue, which can be white or red-violet. Striae appear in places of greatest stretching of the skin - for example, on the stomach of pregnant women or people who have gained a lot of weight in a short time, on the hips and armpits of teenagers who have sharply increased in height in a short period of time.
Why facial scars after acne cannot be removed with laser
The advertisement claims that the laser removes scars from the skin without leaving a trace. In the case of receding acne scars, this is fundamentally wrong.
Laser peels and resurfacing are effective only against problems of the papillary dermis. Not a single doctor will undertake to smooth out the skin and grind away acne scars to the level of the mesh layer - this is a 100% guarantee of the appearance of new scars (we remember that the mesh layer is restored only by scarring).
Only subcutaneous microsurgical cutting of scars using the subcision method copes with scars of the mesh layer and smoothes the skin. Maxim Vasiliev’s method is based on subcision, which removes scars of any depth.
Subcision is a painstaking method of correcting atrophic post-acne scars.
Review
“In my youth I suffered greatly from acne, I waited a long time for it to disappear on its own. On the advice of a friend, I squeezed out the pimples - it only got worse. As a result, acne left scars and spots all over the body, even on the butt. What to do?
I turned to Platinental in hopes of laser resurfacing, but I was referred to Dr. Vasiliev Maxim. It turns out that acne scars cannot be solved with laser; for such cases, there is another method - subcision.
I am very pleased with the first results, the scars have already been removed from my face, my skin has become much smoother.”
Types of scars
Normotrophic scars are most often located at the same level with the skin, they are less noticeable, easiest to correct and differ mainly in shade - they are somewhat lighter than the skin.
Atrophic scars occur after an inflammatory process or injury; they are not as elastic as normal tissues and have a concave surface. A typical example of atrophic scars is stretch marks and post-acne.
Keloid scars can have different shapes; they are elastic, dense, usually with a smooth surface. The appearance of keloid scars can lead to unpleasant sensations: burning, itching, even pain. Typically, such formations protrude above the surface of the skin. They have clear boundaries. Keloid scars can grow and appear again after removal. Most often they form on the outer surface of the shoulder, in the sternum and upper torso. Difficult to correct.
Hypertrophic scars protrude above the surface of the skin. Most often they have a pink tint, and are formed due to the large area and depth of the wound, contamination of the surface or other unfavorable conditions for the healing of damaged tissue. It is mature connective tissue covered by a layer of epidermis. Within six months after its appearance, hyperkeratosis gradually disappears, and the progression of the scar stops.
Why do acne scars form?
We are accustomed to the fact that acne and pimples are exclusively a teenage problem that goes away on its own. In fact, this is not true: more than 90% of acne scars leave behind.
Of course, acne marks can be expressed in different ways: for some they are almost invisible, while for others the skin is literally pitted.
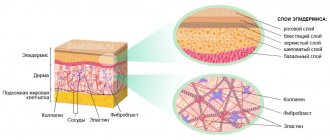
To understand how acne scars form, let's remember the structure of the skin. Under the epidermis is the dermis, which in turn consists of two layers - papillary and reticular.
The upper papillary layer is thin. It got its name because of the papillae that connect it to the top layer of skin - the epidermis. Damage to the papillary layer does not threaten us in any way - it is restored without a scar. Damage to the papillary layer is a banal “water” callus, when a delicate pink skin immediately forms under the blister.
The lower layer of the dermis is reticular. This is a thick layer in which blood and lymphatic vessels, sweat and sebaceous glands, nerve receptors, roots and hair follicles are located. It is the reticular layer of the skin that contains collagen and elastane, which make the skin smooth, elastic and even.
After damage, the mesh layer of the skin is not restored. It heals, but always with the formation of a scar. Inflammation in the reticular layer forms acne scars and the skin loses its smoothness.
Treatment methods
Apart from surgery, there are several ways to treat scars: cryotherapy, wearing compression garments, using silicone preparations, enzyme injections and hormone therapy. But the most effective, safe for the patient and widespread method is laser therapy.
The laser has a highly precise impact with controlled depth, allowing it to avoid damaging healthy tissue. The procedures cause virtually no discomfort, and the recovery period is minimal. The laser removes “extra”, that is, scar tissue and stimulates the production of collagen - the irradiation site heals, and after several procedures not even a trace remains of the scar. The number of procedures is individual, depending on the age of the scar and your characteristics.
To enhance the effect of the laser and stimulate the smoothing of skin relief, plasma lifting is used. The patient is injected with plasma from his own blood into the scar area. This procedure allows the skin to recover faster and stimulates the production of natural collagen and elastin. Plasmolifting is also effective in the treatment of acne. The second option for injection “assistance” with laser is mesotherapy. We use only drugs that are approved by the Ministry of Health of the Russian Federation and have all the necessary quality certificates.
Chemical peeling will also help smooth out small scars - it is effective in working with small atrophic scars. A series of peelings allows you to even out the texture of tissues and skin color.
Special medications can be used to treat keloid scars. They are prescribed only by a doctor - consultation is required!
Damage to the soft tissues of the maxillofacial area occurs in 70% of all maxillofacial trauma. Defects and deformations of the face cause not only anatomical and functional disorders, but also cause severe psychological distress for patients. The degree of these disorders and the nature of reconstructive operations depend on the size and location of the defect, as well as on the combination of damage to individual organs and tissues of the face. Depending on the severity of the damage, destruction of the skeleton of the maxillofacial area, soft tissues, muscles, nerves, as well as organs of the oral cavity, victims need various methods of reconstructive interventions: from small local plastic surgeries to long-term and multi-stage plastic surgery with Filatov stems, bone grafts, adipose tissue and allo- and xenoimplants. Surgical treatment of wounds in the maxillofacial area must be carried out in the early stages. This allows you to reduce the risk of developing wound infection and achieve primary wound healing. Depending on the time factor, primary surgical treatment of wounds is divided into early (in the first 24 hours), delayed (after 24-48 hours) and late (after 48 hours).
According to the general principles of suturing wounds in the maxillofacial area, surgical interventions include: careful treatment of the edges of the wound being sutured; precision - exact comparison and adaptation of the same layers of the wound being stitched; slight elevation of the wound edges to prevent scar retraction during contraction; providing prolonged dermal support to prevent scar expansion in the postoperative period; exclusion of strangulation marks from ligature pressure sores on the skin surface.
There is a primary suture, applied immediately after surgery or injury, and a secondary suture, applied to a granulating wound. A delayed primary suture is applied 2-4 days after the initial surgical treatment of the wound. Removable sutures are placed on the skin, which are removed after the wound has healed. Surgical sutures made of non-absorbable material placed in deep tissue are usually left in the tissue permanently.
Types of seams
Interrupted seams.
The technique for performing them requires passing the needle in two stages. Stitching both edges of the wound in one movement is only possible if small superficial wounds are closed. It is necessary to bring the edges of the wound together atraumatically, using your fingers. If the surgeon uses ophthalmic surgical tweezers for this purpose, they should not press on the edges of the wound, but can only lift the edges from the inside, or support the skin from the outside opposite the needle insertion.
Requirements for tying a knot: 1) each surgeon must know the basic methods of tying knots; the ends of the ligatures in the hands of the surgeon must be constantly and evenly stretched. If the pulling force on one end predominates, a slip knot will result that may come undone; 2) the knot should be tightened until the thread stops sliding, but not too much, since the thread may break or ischemia of the tissue being stitched will occur, which will lead to excessive scarring and a decrease in the aesthetic effect; 3) when using the fingerprint method of tying a knot, it is necessary to help its movement with the index finger; 4) the node should not be left on the line of compared tissues, as it can provoke additional ischemia; 5) the ends of the ligatures on the skin should be no more than 0.5-0.8 cm. If their ends are shorter, the knot may come undone; if they are longer, the surrounding tissue may be injured; 6) the number of nodes is determined by the manipulative properties of the suture material. As a rule, suture material manufacturers indicate the optimal number of knots.
Surgical knot
is a combination of two horizontal crossings of threads and one vertical crossing. The application of this knot is necessary when there is some tension in the tissues, since the first cross prevents the knot from weakening before the second cross.
A simple (female) knot is a combination of two threads crossing vertically.
Knot
- quite reliable, however, in the case of increasing swelling of the tissue, it is delayed, which leads to severe ischemia of the connected edges of the wound.
The application of interrupted sutures to the oral mucosa has some features. Thus, if a surgeon connects mucoperiosteal flaps, he is faced with the problem of tissue tension, even when mobilizing the periosteum. In this case, it is optimal to apply U-shaped sutures, and in areas without tension - interrupted ones.
When suturing areas such as the tongue, palate, buccal area along the line of closure of the teeth, leaving the knot and the ends of the ligatures directed into the oral cavity can lead to trauma to the suture line (biting with teeth) and the contacting surfaces (tongue-palate). Therefore, in such cases, it is necessary to give preference to the use of absorbable suture material and a screw-in suture.
When applying a conventional interrupted suture to a deep wound, a residual cavity may be left. Wound discharge can accumulate in this cavity and lead to suppuration of the wound. If it is difficult to compare the edges of the skin wound, a horizontal mattress U-shaped suture can be used. This can also be avoided by suturing the wound in several layers. Stage-by-stage suturing of the wound is possible with both interrupted and continuous sutures.
Continuous seam
. A continuous suture is applied with one thread. First, a simple knotted suture is placed on one edge of the wound. The knot is tied. Then the entire wound is sutured, making sure that the edges of the wound fit carefully and tightening the thread after each stitch. Having reached the end of the wound, tie the end with a loop formed from incomplete tightening of the last stitch. Sutures are removed on the 7-8th day, and on the face - after 4-6 days.
In addition to floor-by-floor suturing of the wound, a vertical mattress suture is used (according to Donatti). In this case, the first injection is made at a distance of 2 cm or more from the edge of the wound, the needle is inserted as deep as possible to capture the bottom of the wound. A puncture on the opposite side of the wound is made at the same distance. When passing the needle in the opposite direction, the injection and puncture are made at a distance of 0.5 cm from the edges of the wound so that the thread passes through the layer of skin itself. When suturing a deep wound, the threads should be tied after all the sutures have been applied - this facilitates manipulation in the depths of the wound. The use of the Donatti suture allows the edges of the wound to be compared even with their large diastasis.
Surgical sutures applied to the wound, but not tightened, are called provisional. They are tied on the 3-4th day after application in the absence of an inflammatory process in the wound.
An extradermal continuous suture is not used to bring the edges of the wound closer together, but only to accurately align them without tension on the suture line. When applying such a suture, thin suture material and optical magnification are used.
Double row continuous seam
. Deep wounds can be closed with double-row continuous sutures. The first row runs in the subcutaneous fatty tissue, approximately in the middle of the plane of the cut of the adipose tissue, the second row in the skin itself (dermis). The ends of the threads of each row of sutures are brought to the surface of the skin and tied to each other.
When applying an intradermal suture, the needle is injected into the area of the middle of the dermis. In the future, to obtain an optimal postoperative scar, the stitch radius is maintained to 2 mm. You should always prick the needle opposite the point where it was inserted so that when the thread is tightened, these two points coincide. Having completed the seam, the two ends of the thread are grabbed with a tool and pulled until the edges of the wound are completely brought together. A necessary condition when applying such a seam is to avoid tension on the edges. Intradermal suture is not recommended for wounds less than 2 cm in length.
Stitching wounds with staples
. The brackets consist of metal plates several millimeters wide and 1 cm or slightly longer in length. The ends of the staples are bent in the form of rings and equipped with a tip on the inside, which penetrates the tissue when applied and prevents the staples from slipping.
Bracketing technique. To apply staples, grab the edges of the wound with special tweezers, bring them together, fitting them well together, then hold the edges of the wound with one tweezers, and with the other, in the right hand, grab the staple, place it on the suture line and forcefully compress the ends of the tweezers, resulting in the staple bends and grasps the edges of the wound. The staples are placed at a distance of 0.5-1 cm or more from each other.
Removing brackets. The staples are removed, just like the sutures, after 6-8 days using special tweezers or hooks. If special tweezers are not available, the staples can be removed using surgical tweezers by grasping the rings of the staples.
The most important role in the wound healing process is the absence of significant tension on the suture line. Neglect of this principle leads to impaired blood circulation in the edges and walls of the wound, causing their necrosis, which is a prerequisite for wound suppuration. Rough and traumatic surgical technique, extensive detachment of the wound edges to reduce the tension of the suture line, also causes the formation of marginal necrosis. All this largely depends on the training of the surgeon and on the availability of the necessary equipment. Maintaining sufficient blood circulation in the tissues forming the walls of the wound ensures primary healing of the wound with the formation of a thin, delicate scar.
Maintaining all layers of the wound in a position of close contact during the formation of a durable scar largely depends on the correct choice of suture material. An optimal scar is achieved by using special types of sutures, applied with suture material, the biodegradation of which occurs at a later stage.
Care and recovery
After laser resurfacing, the skin recovers quite quickly. However, in the first few hours after the procedure, redness and discomfort may appear. If they cause you discomfort, you can apply a cooling compress to the treatment area.
For 3 days after the removal procedure, you should not wipe the treated areas of the skin with alcohol-containing substances. It is prohibited to visit the sauna and swimming pool, take a hot bath, or sunbathe.
The skin needs to be moisturized. Or use special medical gels and creams that your doctor will prescribe for you.
Each patient at Cleo Line is given detailed care recommendations after the procedure.
How to prevent scar formation?
Before the appearance of herpes, we feel itching and burning at the site of manifestation. If at this moment you use antiviral drugs that stop the spread of herpes, you can avoid the formation of a scar. Start using medications as soon as the first signs of the disease appear. You will help your body and significantly speed up the regeneration of the skin.
How and with what to treat scars from herpes?
If a scar has already appeared, then you can get rid of it in several ways:
- medications;
- cosmetic procedures;
- folk remedies;
- masks and applications;
- innovative Fermenkol gel.
Benefits of ointments and gels
To eliminate scars and crusts from herpes, special products are used. They stimulate skin regeneration and have a number of advantages:
- the highest concentration of active substances is achieved at the site of the lesion;
- the virus does not spread to adjacent areas of the skin;
- you can combine several gels and ointments for scars after herpes, which differ in the principle of action;
- most products do not cause allergic reactions and are easily tolerated by the body;
- you can use healing gels even on old scars;
- there is no need to monitor the dosage.
For example, the innovative product Fermenkol gel has a complex effect on the scar area. Quickly destroys scar marks and gives the skin a natural healthy color. The active components of the gel destroy the basis of the scar - deformed collagen fibers - and restore a healthy skin frame. Fermenkol does not contain hormones and consists of enzymes of natural origin, so it can be safely used on the body and face, including on the scar on the lip after herpes.
After the wounds have healed, use soft cleansing scrubs for the face and body. Cosmetics quickly restore the epidermis. But it is better to use exfoliating creams no more than once a week, so as not to injure the skin.
Result and recovery period
Before and after photos and reviews from the clinic’s patients, which are posted on the Biomed clinic website, will help you evaluate how effective laser resurfacing of facial scars will be. This will allow you to determine how ready you are for the procedure. You will be able to see the results on your face a few days after the session. The skin will noticeably smooth out and pigmentation will even out. Your face will gain a younger, more toned appearance.
To avoid unwanted reactions, after correction you should:
- Avoid exposure to direct sunlight.
- Protect your skin from sun rays using a special cream with a UV filter, Panama hats, and closed clothing.
- Refrain from visiting the solarium, sauna, bathhouse.
- Avoid high physical activity that leads to excessive sweating.
To improve the result, laser resurfacing of facial scars can be repeated after a few months. The number of sessions will be determined by a cosmetologist on an individual basis.
How to get rid of a herpes scar with the help of a cosmetologist?
If you want to eliminate a scar or trace of herpes in visible places, you can use the services of a cosmetologist. You will not get the desired effect in one procedure, but if you complete a full course of manipulations, you can achieve very good results. The following procedures will help eliminate scars after herpes:
- ozone therapy;
- laser therapy;
- deep peeling;
- dermabrasion;
- mesotherapy.
The procedures described above perfectly eliminate fine wrinkles and marks from herpes and acne. Combining several of them at the same time is not recommended. All cosmetic procedures must be carried out under the close supervision of a specialist. Each manipulation has its own contraindications and is allowed only after consulting a doctor. Remember that the procedures are quite painful and require a recovery period.
Preparation for the procedure
If laser removal of facial scars is planned, you should:
- Refuse to visit the beach, solarium, sauna, bathhouse.
- Avoid using cosmetics with high alcohol content.
- Adjust your diet according to your doctor's recommendations.
- Consult on the use of contraceptives, sedatives, vasodilators, hormonal drugs, antibiotics.
- Refrain from chemical peelings and other cosmetic procedures related to skin cleansing and rejuvenation, unless this is agreed upon with the cosmetologist who will perform laser removal of scars on the face.
Your cosmetologist will give you these and other recommendations when drawing up a plan for laser procedures.
How to get rid of a herpes scar on the lip at home?
To eliminate scars, products that we use in everyday life are suitable. They are rich in vitamins and affect not only the scar, but also the skin in general. It is important to use them as additional agents and not as monotherapy. For example, after cosmetic procedures you can additionally use:
- Lemon juice. Brightens the skin and works as a mild acid peel.
- Parsley decoction. A good lightening agent. After preparation, the infusion is poured into an ice tray and placed in the freezer. In the future, cubes are used as pigmentation appears.
- Cucumber juice. Apply a slice to the damaged area to help prevent the skin from drying out.
Herbal infusions
Traditional medicine is rich in recipes that will help get rid of scars. The disappearance of wounds and spots from herpes is accelerated by herbal decoctions:
- chamomile and celandine - heal;
- St. John's wort - starts the regeneration process;
- calendula - helps relieve itching and soothe the skin.
Herbs help lighten the skin and partially eliminate pigmentation formed after herpes.