Pathogenesis
It is believed that melasma is based on genetically determined photoaging disorders (family history in 60% of cases) and exposure to external phototoxic factors - ultraviolet radiation, components of various medications, flavored products, perfumes, toiletries and cosmetics. The role of nerve, vascular, stem cells, and local hormonal factors on the stimulation and activation of melanocytes has not been fully studied. However, the pathological mechanism underlying the formation of melasma spots may include genetic, endocrine, metabolic, physical, drug, chemical and inflammatory aspects, as well as a combination of these.
The basis of melanogenesis is oxidative polymerization from the protein matrix of tyrosine , dihydroxyphenylalanine or catecholamines . The normal course of biochemical reactions of melanogenesis is determined by the presence of tyrosine, molecular oxygen, copper and zinc ions. Under the action of tyrosinase, tyrosine is oxidized into DOPA, from which eumelanins, black-brown pigments, are formed as a result of oxidation and polymerization reactions. The combination of DOPA with cysteine (cysteinol-DOPA) produces pheomelanins, which range in color from yellow to red.
The processes of increased pigmentation and the formation of chloasma spots are characterized by excessive production of melanin (dark pigment) by melanocytes, absorption by keratinocytes (epidermal melanosis), or its deposition in the dermis in cutaneous melanosis. Melanocyte-stimulating hormone does not participate in this pathological process. The key enzyme in melanin synthesis (melanogenesis) is tyrosinase, so it is the effect on its level that affects pigmentation. In addition, the speed of transfer (transfer) of melanosomes to keratinocytes plays a role, as well as the intensity of the change in cell populations in the epidermis and desquamation.
Introduction
Melasma is an acquired hyperpigmentation that is characterized by bilateral, uneven brown patches on exposed areas (the face and, less commonly, the forearms) [1].
Most often found in dark-skinned women - usually Asian or Hispanic with Fitzpatrick skin types III-IV. The formation of melasma is influenced by various factors including sun exposure, female sex hormones and genetic aspects [2]. The pathogenesis of melasma is complex, although it was initially thought that only melanocytes were involved. However, existing studies indicate a more heterogeneous pathogenesis, including the interaction of keratinocytes, mast cells, gene dysregulation, increased vascularization and destruction of the basement membrane [3]. It is critical that clinicians are familiar with the pathogenesis of melasma, as this may assist in prescribing successful combination treatment options for this notoriously difficult and recurrent condition. The purpose of this review is to summarize newer aspects of pathogenesis and the latest research methods.
Discussion
Publications describing the pathogenesis of melasma were mainly found through a literature search in the PubMed database. Key words: melasma, pathogenesis, melanogenesis, melanocytes, keratinocytes, mast cells, ultraviolet (UV) radiation, basement membrane, vascularization, prostaglandins, estrogen, progesterone, therapeutic agents and tranexamic acid. Several articles were reviewed for relevance from 1981 to 2022, and references to individual articles were also reviewed. A total of 35 articles were included, which included basic science research, randomized controlled trials, commentaries and reviews.
Melanocytes
Melasma is known to increase melanin production. However, whether this is accompanied by an increase in the number of melanocytes is still debated [4, 5]. The specific mechanisms of increased melanin deposition have not yet been elucidated. Ultraviolet radiation has been shown to upregulate melanocyte-stimulating hormone (MSH) receptors, also known as melanocortin-1 receptors (MC1-R), on melanocytes, allowing binds hormones better and therefore increases melanin production [6]. Proopiomelanocortin (POMC) is cleaved to form the peptides a-melanocyte-stimulating hormone (a-MSH) and adrenocorticotropic hormone (ACTH) in response to UV [7].
When these peptides bind and activate MC1-R, they increase levels of protein kinase A (PKA), which phosphorylates the cAMP response element (CREB) (Fig. 1). The cAMP response element is a transcription factor for another microphthalmia associated transcription factor (MITF), a key regulator in the melanin synthesis pathway. MITF controls the expression of tyrosinase, an enzyme responsible for several steps of melanogenesis [8]. UV radiation has also been shown to endogenously generate 1,2-diacylglycerols (DAG), a type of second messenger, from melanocyte plasma membrane phospholipids through the phospholipase C and D (phospholipase, PLC and PLD) pathways. These DAGs continue to activate tyrosine and consequently enhance melanogenesis (Fig. 1), [9].
The tumor suppressor protein p53 may also play a role in UV-induced melanogenesis. This protein enhances the production of POMC in keratinocytes after UVB damage, which leads to an increase in melanin synthesis. In addition, the tumor suppressor protein p53 also increases the transcription of hepatocyte nuclear transcription factor-1alpha (HNF-1 alpha), which induces tyrosinase, which in turn activates melanin production even in the absence of keratinocytes ( Fig. 1) [8]. Although the above pathways activate melanogenesis throughout the skin, the response to ultraviolet radiation is exaggerated. In melasma, increased expression of a-MSH is maintained, increasing melanin production [7].
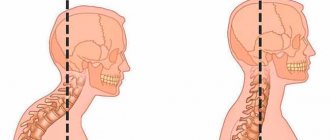
Solar elastosis and photoaging
Solar elastosis refers to the accumulation of abnormal elastic tissue in the dermis as a result of chronic sun exposure or photoaging. Patients with melasma have been found to have high levels of solar elastosis in the affected skin. In addition, histological examination shows that melasma skin contains thicker and more twisted fragmented elastic fibers compared to normal skin [3].
Exposure to ultraviolet B can stimulate keratinocytes and lead to an increase in the number of melanocytes and, consequently, melanin production due to the secretion of various growth factors, cytokines and hormones, including inducible nitric oxide synthase (iNOS [10]. UV-B radiation also increases the production of plasmin by keratinocytes. This enzyme leads to increased levels of arachidonic acid and a-MSH and therefore stimulates the melanin synthesis pathway [11]. All these factors lead to hyperpigmentation of the affected skin. In addition, it has been suggested that even visible light may play a role in the pathogenesis of melasma, especially in dark skin types (Fitzpatrick types IV-VI), through interaction with opsin 3 sensor (Fig. 1) [12].
Mast cells and neovascularization
The number of mast cells in the skin with melasma is higher than in intact skin [8]. Ultraviolet irradiation causes the release of histamine from these mast cells, leading to downstream effects [13]. The binding of histamine to the H2 receptor activates the tyrosinase pathway and stimulates melanogenesis. This finding may help elucidate the relationship between inflammation caused by ultraviolet radiation and subsequent hyperpigmentation [14].
In addition, UV radiation also increases the production of mast cell tryptase, which activates matrix metalloproteinase (MMP) precursors. These active enzymes then break down type IV collagen and damage the basement membrane. Granzyme B, released directly from mast cells, further damages the extracellular matrix (ECM). Tryptase may also promote solar elastosis by inducing elastin production [3].
Finally, mast cells induce hypervascularization, another important clinical finding in melasma, by secreting proteins such as vascular endothelial growth factor (VEGF), fibroblast growth factor-2 , FGF-2) and transforming growth factor-B (from English transforming growth factor-B, TGF-B). These angiogenic factors increase the size, density, and degree of vascular dilatation in affected skin and represent another therapeutic target in the treatment of melasma (Figure 1) [2, 3].
Damage to the basement membrane
Damage to the basement membrane plays a key role in the pathogenesis of melasma. As described above, UV damage activates MMP2 and MMP9, leading to the destruction of type IV and VI collagen in the basement membrane [3]. Cadherin 11, an adhesion molecule that is elevated in melasma skin, may then mediate interactions between fibroblasts and melanocytes and promote melanogenesis [15].
Cadherin 11 is also responsible for upregulating the expression of MMP1 and MMP2, leading to further collagen breakdown and elastin accumulation in melasma skin. These effects may even be independent of ultraviolet radiation [15]. Damage to the basement membrane also promotes the migration of melanocytes and melanin granules down into the dermis, resulting in the persistent nature of melasma. Thus, trauma caused by lasers or any therapy that further damages the basement membrane may aggravate the disease. Similarly, restoration of the basement membrane may lead to decreased recurrence (Figure 1) [3].
Skin inflammation
Prolonged ultraviolet radiation causes inflammation of the skin and activates fibroblasts. These cells then secrete stem cell factor (SCF), which can diffuse and activate melanogenesis in the overlying epidermis [16].
Likewise, levels of stem cell growth factor receptors, also known as c-kit, are also increased in melasma. When c-kit binds to SCF, the tyrosine kinase pathway responsible for melanogenesis is activated [17]. Skin inflammation is also characterized by increased levels of COX-2 and prostaglandins, which further stimulate melanocytes (Fig. 1) [18].
Hormonal influence
Estrogen has also been shown to play a role in the pathogenesis of melasma, which explains the increased prevalence among postpubertal women, patients taking oral contraceptives, and pregnant women. Studies have shown an increase in the number of estrogen receptors in the dermis and progesterone receptors in the epidermis in melasma [19, 20].
Binding of estrogen to its receptors on melanocytes and keratinocytes can activate the tyrosinase and MITF pathways, inducing melanin synthesis [21]. In addition, increased expression of the PDZK1 protein (PDZ domain protein kidney), which regulates ion exchange, in melasma may mediate the interaction between estrogens and ion exchangers to increase melanogenesis and melanosome transfer [22]. The influence of estrogen represents another important target in melasma therapy.
New approaches to therapy
The complex pathogenesis and recurrent nature of melasma make its therapy difficult [1]. Traditionally, melasma has been treated with topical treatments including hydroquinone (which inhibits tyrosinase), tretinoin, corticosteroids, and combination creams with various formulations (Table 1). Hydroquinone has long been an accepted treatment option, but concerns about its side effects have prompted the use of potentially safer alternatives. Current treatment methods include topical agents, chemical peels, laser and light treatments, and systemic agents [23].
Tranexamic acid (TXA), a plasmin inhibitor, has gained popularity as a systemic therapy for melasma and is available in oral, topical, and injectable forms. Plasmin increases arachidonic acid and prostaglandin levels in keratinocytes, leading to increased melanogenesis. In addition, plasmin releases ECM-bound VEGF, promoting angiogenesis [24].
Thus, tranexamic acid is one of the few treatments for neovascularization present in melasma. A recent double-blind clinical trial found that topical TXA was as effective as hydroquinone in reducing the mean Melasma Area and Severity Index (MASI) score with fewer side effects [25]. Another placebo-controlled, double-blind study showed that oral TXA was superior to placebo in the treatment of moderate to severe melasma with minimal side effects [26].
Recent developments in melasma therapy include specific agents targeting different aspects of melasma pathogenesis. Therapeutic alternatives to traditional topical agents, such as small ribonucleic acid (siRNA) agents, have been explored. Microphthalmia-associated transcription factor-siRNA as a transdermal target peptide inhibits the tyrosinase pathway of melanogenesis without significant side effects. This new option also shows promise in the treatment of melanoma and is safe enough for daily use [27].
Metformin, an antidiabetic drug that acts by reducing cAMP levels, has been shown to reduce melanin content in melanocytes by inhibiting downstream synthesis pathways [28]. Proton pump inhibitors (PPIs), such as omeprazole, can also inhibit melanogenesis when applied topically. PPIs are thought to interfere with ATP7A by blocking copper uptake by tyrosinase, leading to its destruction and therefore reducing melanogenesis [29]. More recently, topical combination therapy has been proposed that combines estrogen and VEGF antagonists. This therapy is aimed at both melanogenesis and angiogenesis [22].
Laser and light treatment for melasma, including intense pulsed radiation, targets excess pigment in the skin, but does not affect the main links in the pathogenesis of the disease. As a result, relapses are common, especially when laser is used as monotherapy. In addition, high-intensity lasers can further damage the basement membrane and “dump” melanin into the dermis, as mentioned above [3].
Regardless of the treatment method chosen, sun protection is critical to prevent the development of new lesions and prevent the worsening of existing melasma [23]. Melasma patients are advised to use a broad-spectrum UVA/UVB sunscreen with SPF30, preferably with a physical blocking agent such as zinc oxide or titanium dioxide. Wearing wide-brimmed hats and avoiding peak sunlight hours will also help [23]. Recent research suggests that sunscreen that blocks visible light in addition to ultraviolet radiation results in even greater therapeutic benefits and can also enhance response to traditional lightening agents such as hydroquinone [30].
Conclusion
Melasma is a condition of facial hyperpigmentation with various pathogenesis links. Increased melanogenesis, extracellular matrix changes, inflammation, and angiogenesis all play a role in the development of melasma. The multifactorial nature of the disease makes treatment difficult. In addition, melasma can recur. A better understanding of pathogenesis is key to the development of new targeted therapeutics.
Classification
Depending on the differences in skin coloration, melanosis is divided into the following types:
- hyperpigmentation, or in another way - hyperchromia, is characterized by increased coloration of the skin, its limited form is called chloasma;
- hypopigmentation or hypochromia is a weakening of the function of dermal melanocytes and is manifested by a partial decrease in the intensity of skin pigmentation;
- depigmentation or achromia is a complete lack of skin color resulting from dysfunction of dermal melanocytes and blocking the formation of melanin.
Types of chloasma
Taking into account the increased level of melanin, hyperpigmented spots are divided into epidermal, dermal and mixed, affecting both the epidermal and dermal layers.
Depending on the location and characteristics of chloasma, it happens:
- centrofacial - spots are located on the forehead, cheeks, and upper lip;
- mandibular - on the jawline and chin;
- molar – when located in the area of the projection of the molars and on the cheeks (in 50-80% of cases);
- extrafacial – the skin of the forearms, décolleté and other areas exposed to the sun is affected; it is also called lentigo and is characteristic of old age and lovers of solariums .
What is melasma
Melasma is a skin pigmentation disorder that results in gray, bluish or brown spots, usually with a clear outline. They are benign and do not pose any danger to the body. The complexity of the treatment depends on how deep the pigment is. So, for example, if the stains are in the epidermis, the most superficial layer, it will be easiest to get rid of them. But if the pigment penetrates the entire skin or partially affects the deeper layers (such types of disease are called dermal and mixed), it will be much more difficult to lighten these areas.
Instagram content
This content can also be viewed on the site it originates from.
Causes
The causes of pathological changes in skin pigmentation may be:
- External – these include excess solar radiation, as it is a direct catalyst for the formation of apigmentation or hyperpigmentation. Therefore, the frequency of use of photosensitizing agents, for example, those found in external cosmetic preparations, as well as taking oral photosensitizers, is extremely important; such risks exist in pregnant women and during perimenopause, as well as taking hormonal drugs, contraceptives containing estrogen and progesterone , using intrauterine devices , implants or hormone replacement therapy, or suffering from various chronic gastrointestinal diseases and ovarian tumors.
- The internal causes of melasma spots come down to genetic predisposition.
When does chloasma occur?
The cause of chloasma may be a disorder of ovarian function or helminthic infestation. In this case, most often lesions occur on the face and especially around the mouth (chloasma photo on the face). Chloasma is most typical for people who sunbathe easily and have naturally brown skin (Fitzpatrick skin phototypes III, IV); in more rare cases, it can occur in fair-skinned people (Fitzpatrick types I, II), as well as with Asian and African phototypes ( according to Fitzpatrick V, VI).
Phototypes according to Fitzpatrick
Cachexic chloasma (as in the photo on the body) is a severe form of hyperpigmentation, which is based on oncological processes and various debilitating diseases, including malaria , tuberculosis and cirrhosis of the liver .
Chloasma on the body
Table of contents
- Etiology and pathogenesis
- Clinical manifestations
- Principles of treatment
Melasma (chloasma, pregnancy mask, melasma, melasma , chloasma ) is a chronic recurrent acquired dyschromia caused by increased activity of epidermal-melanin units. The epidermal-melanin unit is a union that consists of one melanocyte and several keratinocytes, facilitating the transfer of pigment granules from the melanocyte to the surrounding keratinocytes.
In our company you can purchase the following equipment for the treatment of melasma:
- M22 (Lumenis)
- Fraxel (Solta Medical)
Melasma occurs in areas of the skin that are exposed to severe and/or regular sun exposure, more often in women of reproductive age. It negatively affects quality of life due to its high prevalence, involvement of visible areas of the face and body in young patients, and relative resistance to therapy. Melasma affects mainly women (90% of cases) of any race, but more often with dark skin phototypes (IV-VI). The average prevalence of the disease in the population ranges from 8.8% to 40%. According to some reports, the likelihood of melasma developing during pregnancy is 15–50%.
Chloasma is the name given to melasma that occurs during pregnancy (“mask of pregnancy”). The word chloasma comes from the Greek chloazein (green), while melasma comes from the Greek melas (black). Since chloasma is never green, it is more correct to call it melasma.
Symptoms
Melasma or chloasma are symmetrically located, variously shaped, sharply defined pigment spots of yellow-brown or dark yellow-gray color. They can merge into larger ones over time. Locations: forehead, eyelids, temples, cheeks, up to disfigurement of the entire face. In addition, chloasma patches may appear on the skin around the nipples and on the vulva. Unlike freckles, chloasma spots are clearly defined and larger in size.
In spring and summer, chloasma may look brighter, and in winter it may become somewhat paler. The spots are not characterized by peeling or itching and are generally asymptomatic, but they can become chronic and persist for the rest of life.
Melasma as a result of photoaging
The appearance of pigment spots on the face is a common problem for women after 30. And although they do not cause inconvenience, local or systemic symptoms, as an aesthetic flaw they bring psychological discomfort.
Chloasma on a woman's face
Melasma causes the development of single or multiple spots of irregular shapes of dark brown color and its other shades as in the photo (melasma on a woman’s face).
If melasma is localized on the cheeks and combined with telangiectasia, then this may be evidence of liver damage.
Tests and diagnostics
When diagnosing, clinical history, examination, possibly using a Wood's lamp, as well as dermatoscopy and biopsy are important. The histological picture can be expressed as:
- melanin is deposited in basal and suprabasal keratinocytes, highly dendritic (branched) and intensely pigmented melanocytes are detected;
- melanophages with melanin;
- solar elastosis due to fragmentation of elastic fibers;
- vessels are enlarged, angiogenesis is enhanced.
To monitor response to treatment, a method of serial photographs and various severity indices, including the Melasma Area and Severity Index (MASI) or modified MASI, are used.
Treatment with folk remedies
There are many folk recipes for improving the condition and color of the skin, because since ancient times, pallor was a sign of nobility. Nowadays, to make their face brighter, women use such means as:
- hydrogen peroxide in combination with brewer's yeast and ammonia (2:1:1) is excellent for spot application on stains, the effect occurs in about 15 minutes;
- parsley with lemon juice and honey (15, 5 and 5 g, respectively) - just leave this mask on for 20 minutes to tone the skin, achieve a pronounced anti-aging effect and relieve fatigue;
- fermented milk drinks - kefir, yoghurt, sour cream, etc. together with flakes they have a well-known mild whitening, nourishing and exfoliating effect.
How is melasma treated with fractional laser?
- Treatment of melasma with fractional laser is carried out under local anesthesia with lidocaine cream.
- Before applying the anesthetic to the skin, the face must be cleansed of makeup.
- The numbing cream should remain on the skin for at least 40 minutes.
- After preparation, the affected areas of the skin are scanned with a laser beam.
- The laser treatment procedure is usually comfortable, with no significant discomfort noted.
- The duration of the session is 20-30 minutes.
- After treatment, persistent redness of the facial skin and slight swelling are noted.
Diet for melasma and chloasma
Diet for hormonal imbalance in women
- Efficacy: therapeutic effect after 3 weeks
- Timing: constantly
- Cost of products: 1400-1500 rubles per week
The formation of melasma is significantly influenced by the hormonal background of the body, so in addition to external treatment of the problem, you should get tested, consult an endocrinologist, and also normalize nutrition and sleep - two fundamental aspects of health. It is important to give up bad habits and alcohol.
The menu should be chosen to be balanced and complete, providing the body with the daily necessary proteins, fats, carbohydrates, vitamins and minerals. To make your diet as healthy as possible:
- drink 1.5-2 liters of clean water;
- eat enough proteins, getting them from dietary meat, eggs, milk and seafood, as well as legumes;
- provide yourself with vitamins and fiber - eat more fresh salads, sliced fruits, drink juices, berry fruit drinks and compotes;
- don’t forget about healthy fats - nuts, seeds are considered good snacks, and fish should be on the table 2-3 times a week;
- do not fry, smoke or pepper foods, refuse store-bought sauces and any “packaged products”;
- carbohydrates can be healthy - these are porridge, whole grain baked goods and pasta, natural sweets such as natural marshmallows, marmalade and nougat.