Those who do not follow a sleep schedule, abuse alcohol and do not adhere to a healthy diet , bags appear under the eyes with age. This problem also affects quite young people. But sometimes such swelling and swelling occurs even in people leading a healthy lifestyle .
In such cases, you should pay more attention to this symptom, since these may not be easily removable bags, but fatty hernias, which are much more difficult to get rid of.
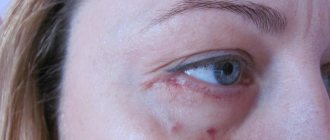
Symptoms
Hernias under the eyes can be recognized by the following signs:
- decreased visual acuity;
- increased lacrimation;
- swollen areas of skin under the eyes do not decrease or increase during the day or when drinking large amounts of water;
- the skin of the eyelids, under which hernias form, takes on a bluish or reddish, plum color;
- the vascular network may more or less appear on the skin of the eyelids.
such hernias also form above the eye - then from the outside it seems that the person’s eye shape is reduced and the swelling affects the periocular area in a circle.
Keep in mind! For the vast majority of people, this problem appears only under the eyes.
About pathology
A vitreous hernia is an ophthalmic abnormality that very often (though not always) occurs as a complication of cataract surgery. Today, thanks to the introduction of high technologies, there has been a significant decrease in the prevalence of secondary vitreal hernias. However, a number of other modern surgical interventions are associated with a high risk of their development. Thus, intraoperative leaching of viscoelastic in 20% of cases leads to the occurrence of a hernia. Hernia defects are formed during cryoextraction of cataracts in 5-55% of cases.
How to distinguish hernias under the eyes from swelling?
Know! A person can make sure that there are indeed fatty deposits under the eyelid independently at home.
It is enough to press your finger on your closed eye - and you will be able to see with your other eye or feel how the bags under the eyes harden, swell and noticeably increase in size.
Also, a person himself can feel how a feeling of skin tension is created due to sagging.
Another reason to suspect a hernia is the fact that there are no ophthalmological diseases .
At the same time, the daily routine, diet and the amount of stress and nervous shocks have recently remained unchanged and there are no physiological prerequisites for the development of bags and swelling.
Cosmetological methods for correcting fat bags
Wellness center Face&Body specialists successfully correct bags under the eyes using injection techniques:
- mesotherapy and biorevitalization;
- contour plastic surgery.
Mesotherapy . The essence of the procedure is the introduction under the skin of drugs that relieve swelling in the periorbital area and increase skin turgor. Most of these drugs contain drugs with lymphatic drainage action as active substances.
Face&Body cosmetologists work with the new generation biorevitalizant MesoEye C71™, which, in addition to hyaluronic acid, includes the PeriOrbital peptide complex. Its task is to activate lymph circulation in the periorbital zone and reduce vascular permeability. Biorevitalization with MesoEye C71™ is effective for severe swelling of the face and gives long-term results. Lymphatic drainage massage helps to strengthen and prolong the effect of the procedure.
Contour plastic . This correction method involves camouflaging the bags by changing the texture of the skin around them. To do this, fillers (again based on hyaluronic acid) are injected into the nasolacrimal and eyelid buccal grooves. They even out the relief between the cheek and the fat packet, making the latter invisible. Face&Body cosmetologists work with fillers from popular brands: Yvoire, Juvederm, Belotero, etc., which have proven themselves best in correcting bags under the eyes.
Bags under the eyes: before and after correction
Causes
Need to know! The causes of the formation of infraorbital hernias can be:
- severe and/or frequent stress and nervous exhaustion;
- genetic predisposition;
- constant long-term exposure to the sun;
- hormonal disorders in the body;
- large lacunae due to the atypical structure of the skull;
- constant consumption of large amounts of salt, fats and smoked foods;
- smoking and frequent drinking;
- work associated with constant strain on the visual organs;
- chronic lack of sleep and constant overwork.
For most people, even in the absence of the above problems, hernias under the eyes still appear sooner or later.
But if you notice these changes in time, you can take appropriate measures to significantly slow down such pathological processes.
What to do if a defect occurs?
If there is a hernia in the upper eyelid
or below, then the best thing to do would be to make an appointment with a doctor. The ophthalmologist will determine:
- Is the problem really an accumulation of adipose tissue;
- how serious changes have occurred in the structure of the skin;
- Is surgical removal required or is it better to use other techniques.
To make a diagnosis, a specialist usually only needs a visual examination, medical history, biochemical blood test and ultrasound examination. Additional types of examinations are prescribed if there is a suspicion of diseases of internal organs and systems. Before receiving an appointment for surgery or other recommendations regarding further therapy, the patient should refuse to use cosmetics, get more rest, avoid stress, eat a balanced diet, and under no circumstances try to be treated with folk remedies.
How to remove: methods of treatment and elimination
Modern medicine and cosmetology offer several different ways to get rid of hernias under the eyes without surgery or surgical treatment .
Stay up to date! Depending on the severity and age of the patient, they will be more or less effective.
But experts warn: the only truly effective method of treatment will be surgical removal .
All other methods can only hide the problem, stop the development of hernias or eliminate them partially.
Surgery
Elimination of hernias surgically is possible only through blepharoplasty , which is performed in two ways : scalpel and transconjunctival.
In the first case, general anesthesia is used, after which an incision is made with a scalpel along the edge of the eyelashes of the lower eyelid .
Treatment methods for eyelid hernia
An ophthalmologist must diagnose a hernia of the eyelid. When this disease is detected, we most often recommend surgery to the patient.
Although hernias themselves do not pose a health hazard and can only in exceptional cases contribute to vision impairment, they are an unpleasant cosmetic problem. Surgery to eliminate an eyelid hernia eliminates this pathology and helps correct age-related skin changes.
Surgical treatment of eyelid hernia is carried out in two main ways:
- Percutaneous approach
- when the surgeon makes an incision along the outer skin surface of the eyelid, excising excess skin and fatty tissue. Small wounds after this operation heal quickly and remain invisible - Transconjunctival access
- excess fat is removed through the conjunctiva, the inner surface of the eyelid. With this method, no external traces are left.
Removal of an eyelid hernia is painless for the patient on an outpatient basis. If you follow all the doctor’s recommendations before and after surgery, the success of the treatment is guaranteed, and the problem will be eliminated forever.
At Dr. Belikova's Eye Clinic, you can undergo a comprehensive vision examination and receive detailed recommendations from our specialists.
Prevention measures
It is impossible to completely prevent the formation of hernias under the eyes.
Remember! But you can prevent their rapid development by following these preventive recommendations:
- from time to time wipe your face with ice cubes , for the preparation of which it is better to use not water, but decoctions of medicinal herbs;
- avoid abuse of alcohol, fatty, smoked and spicy foods and, if possible, quit smoking;
- go to bed on time and not disturb the established daily routine;
- Regularly take at least half an hour walks to improve the overall tone of the body.
PREPARATION FOR PROCEDURES, REHABILITATION
No special preparation is required for cosmetic procedures. You should follow your doctor’s recommendations and avoid overheating the skin in saunas, spa treatments, solariums, etc.
Before eliminating the problem, it is important to reduce eye strain as much as possible and not use irritating cosmetics. It is highly undesirable to drink alcohol and smoke. These measures will also contribute to speedy rehabilitation.
Preparation for blepharoplasty involves the need to undergo tests and consult doctors.
Rehabilitation after non-invasive treatment is based solely on the recommendations of a cosmetologist. The doctor will most likely advise you to refuse:
- from exposure to (long-term) ultraviolet rays;
- protect your eyes with sunglasses;
- apply moisturizing creams to the skin;
- do not use scrubs or peeling.
Reviews from people about hernia removal
“
At the age of 47 , when I had noticeable bags under my eyes , I immediately decided to have surgery. Because, firstly, I have the money for this, and secondly, I don’t believe in cosmetics that only hide such defects.Before the operation, I underwent examinations , during which it turned out that I had fatty hernias .
operation did not eliminate them completely, but they are now much smaller .”
Tatiana Zabolotskaya, Pyatigorsk.
“ Hernias under my were removed three years ago under local anesthesia.
Despite such anesthesia, the sensations were very unpleasant, but I was satisfied with the result : at my age it is difficult to count on an ideal result, but the hernia was removed almost completely .
of them is a painful bluish color , but bringing it back to normal is a less complicated procedure.”
Marina Oshanina, 48 years old.
“I
had a difficult time undergoing blepharoplasty to remove infraorbital hernias : local anesthesia did not provide complete pain relief. Therefore, during the operation, which lasted an hour and a half, I experienced very unpleasant and at times painful sensations.But overall, I was satisfied with the result , and although the skin doesn’t look like it did in my youth, at least now I don’t have those huge bags .”
Sofia Bashkeeva, Kazan.
Pathogenesis
A perforated injury to the eye causes a rupture of the border plate of the vitreous, which is why a hernia is formed. The area of the hernial protrusion is directly related to the size of the wound canal, the level of (IOP), and the condition of the adjacent tissues. A complicated hernia is formed due to the migration of vitreal masses and blood clots into the anterior chamber area. In the case of eye contusion, this occurs due to mechanical pressure that deforms intraocular structures and a sharp increase in IOP. The vitreous body shifts to the anterior pole of the eye and partially extends beyond the pupil. Contact of the anterior surface of the hernia and the endothelium of the cornea causes swelling of the latter. This leads to visual impairment.
Diagnostics
When the formation of a hernia occurs at the time of surgery, it is detected with the naked eye of the surgeon intraoperatively. In case of a traumatic variant of its origin or if the hernial protrusion formed in the postoperative period, studies clarifying the diagnosis are required. These include:
Biomicroscopy. The protrusion in a primary hernia has the appearance of a pathological formation hanging over the pupillary edge. At the anterior limiting membrane, the surface appears smooth and uniform without damage. No decrease in the transparency of optical media is observed.
Gonioscopy. Rupture of the border plate leads to the appearance of individual fragments of the vitreous in the anterior chamber. These fragments are represented by gelatinous structureless masses that are found in aqueous humor. In the case of a severe pathological process, fragments of the vitreous fill the entire anterior chamber of the eye.
Ultrasound. Ultrasound examination is prescribed to differentiate primary and secondary forms of pathology. The primary form is a homogeneous hernia formation with clear edges. The secondary form is accompanied by signs of crushing of the vitreous body of the eye.
OCT. The study is performed to assess the condition of the inner lining of the eye. With its help, even with a severe penetrating wound or massive endovitreal hemorrhage, it is possible to detect the first signs of retinal detachment.
Visometry. Visual functions do not suffer with an uncomplicated hernia. A pronounced decrease in visual acuity is observed only in the secondary form of the disease. Surgical treatment, in this case, is the only way to restore visual functions.
In differential diagnosis, comparison is made with fibrinous exudate of the anterior chamber. The exudate is organized or resolved over time, but the hernia does not change during dynamic observation and remains the same.
Complications of vitreous hernia
A frequent complication of the pathology is rupture of the limiting membrane. Hemorrhages into the hernial sac and its delamination are not uncommon. If the origin of the hernia is traumatic, foreign bodies may enter the eye, and destructive changes increase. When the iris is simultaneously damaged, blood and pigment fragments may be detected in the vitreous. The most unfavorable complications in this case are secondary glaucoma and retinal detachment. Distortion of the shape of the pupil often occurs. Intraocular hydrodynamics are disrupted, which leads to the development of ocular hypertension. Contact of the hernia with the cornea can lead to the development of its endothelial-epithelial dystrophy.
Classification of pathology
As a rule, a vitreous hernia is an acquired disease. Its congenital form is extremely rare, and occurs as one of the complications of eye malformations.
Experts classify pathology as complicated and uncomplicated forms. Postoperative protrusions are divided into early and late according to the time of appearance. In addition, there is a classification of hernias according to clinical signs:
- Primary. Such hernias are considered a particularly favorable variant of the disease. They are not accompanied by destruction of the anterior limiting membrane. The hernial protrusion itself has the appearance of a small “bubble” deviating towards the pupillary edge of the iris; the anterior chamber of the eye is not involved in the pathological process.
- Secondary. This type of hernia is characterized by destruction of the anterior border plate. The strength of the membrane decreases due to liquefaction of the vitreous. A linear break is formed in the thinnest area. Masses of vitreous substance penetrate into the anterior chamber, where they remain.