The introduction of drugs into the patient's body that cause inhibition of the central nervous system is intravenous anesthesia. In addition to the above, it helps:
- turn off consciousness;
- block or significantly weaken some reflexes;
- completely relieve pain.
At the DentalHouse clinic we use only modern drugs of the latest generation, which ensure the safety and comfort of the patient.
What is special about intravenous anesthesia?
Perhaps the main advantage of intravenous anesthesia is its immediate effect, as well as the rapid recovery of a person from an unconscious state, especially in comparison with other types of general anesthesia. The duration of anesthesia depends on the drug chosen and the volume of administration. Therefore, if the doctor needs more time for the operation, the anesthesiologist will gradually add medication to prolong it.
Intravenous anesthesia is the best choice for patients who are afraid of dental treatment. Complete muscle relaxation does not occur; the patient breathes on his own the entire time he is working under intravenous anesthesia. In case of long and complex operations, experts recommend a combination of several types of anesthesia.
Intravenous anesthesia over 30 minutes
prevents the patient from deep sleep, and not through the administration of muscle relaxants, as with endotracheal anesthesia. Therefore, during intravenous anesthesia, the patient breathes on his own and in most cases does not need a ventilator (artificial lung ventilation).
This type of anesthesia is widely used due to its simplicity, ease of dosing and management of anesthesia. It is used in cases where short-term and low-traumatic surgery or research is intended, since the effect of the drugs used for this type of anesthesia is short-lived and has a weak analgesic (pain-relieving) effect. Their main property is to turn off consciousness.
On average, depending on the type of drug used, one dose of the drug provides up to 20 minutes of unconsciousness. Therefore, if it is necessary to prolong anesthesia (in connection with an operation), regular addition of an anesthetic to a vein is carried out to maintain a state of drug-induced sleep.
Its main advantages include:
- — unnoticeable for the patient, but fairly quick introduction to anesthesia;
- — a pleasant fall asleep for the patient, practically without the stage of excitement;
- — rapid recovery of the patient from an unconscious state;
- - no irritation of the mucous membrane of the respiratory tract, as with inhalation anesthesia;
- — minimal impact on internal organs;
- - low incidence of nausea and vomiting.
Indications and contraindications.
Intravenous anesthesia is used everywhere today for short-term surgical operations and some instrumental research methods.
Indications for intravenous anesthesia:
- - hysteroscopy;
- - abortion;
- — obstetric manipulations (including suturing perineal tears after childbirth);
- — minor proctological operations (excision of anal fissure, hemorrhoids, polyps);
- - hiding abscesses;
- — short-term operations in urology;
- — in traumatology (reduction of dislocations, subanesthetic dressings in burn patients, osteosynthesis);
- - with instrumental research methods (fibrogastroduodenoscopy - FGDS, fibrocolonoscopy - FCS, bronchoscopy, MRI under sedation in pediatrics, etc.)
- — in dentistry (dental treatment under anesthesia).
In the case of planned operations, contraindications to intravenous anesthesia are:
- — Failure to follow a diet before surgery. A full stomach can cause regurgitation and aspiration (choking) of its own stomach contents (vomiting). The patient's stomach must be completely empty before anesthesia! Therefore, in the evening before the operation and in the morning, for the safety of the patient, eating and drinking is strictly prohibited!
- — Cardiac dysfunction (myocardial infarction, less than a month has passed since its onset, unstable angina or severe stable angina, uncompensated heart failure, severe heart rhythm disturbances);
- — Untreated hypertension or hypertensive crisis;
- — Acute neurological diseases, including coma;
- — Severe hepatic and/or liver failure;
- — Acute respiratory tract infections (pneumonia, acute or chronic bronchitis in the acute stage, exacerbation of bronchial asthma, ARVI), which can make it difficult for a patient to breathe independently under anesthesia;
- — Infectious diseases, including intestinal infections;
- — Also, each specific drug used for anesthesia has its own list of contraindications.
Important!
- — To avoid possible complications, the patient must undergo all necessary examinations and consultations with specialists before surgery/anesthesia.
- — You need to have an interview with an anesthesiologist who will explain to the patient the essence of the anesthesia; will help you choose the most appropriate and safe type of anesthesia in each specific case; will give recommendations on preparing for surgery under anesthesia.
- — During any procedure/operation under anesthesia, the anesthesiologist conducts careful monitoring with the measurement of basic vital parameters: blood pressure, pulse, heart rate, oxygen saturation, analysis of the gas mixture that the patient breathes, etc.
- — Modern anesthesia and monitoring equipment allows you to promptly correct emerging deviations and avoid complications.
Who is this method suitable for?
Intravenous anesthesia is recommended if:
- there is dental phobia (stomatophobia) – fear of dentists and appropriate treatment;
- a person has increased excitability.
- Difficulty in pain relief
There are no absolute contraindications for intravenous anesthesia - DentalHouse anesthesiologists will select the optimal drug with the maximum possible gentle effect on the patient’s body. Before intravenous anesthesia, the patient is given a list of tests that must be submitted to the clinic. The anesthesiologist must examine and consult the patient. Specialists may refuse to administer intravenous anesthesia if the concomitant general somatic disease is in the stage of exacerbation or decompensation.
Anesthesia and anesthesia
Anesthesia and anesthesia
We consider it extremely important to inform patients as much as possible about everything that awaits them during and after surgery. It is necessary that the patient can best prepare for a rather complex ordeal - surgery. It’s not for nothing that they say – forewarned is forearmed. Many years of experience show that well-informed patients undergo surgery easily, recover quickly and return to active life.
Will it hurt during the operation?
Such a question for modern medicine sounds somewhat naive, because back in the second half of the 19th century, pain during surgery was over. Since then, anesthesiology (a branch of medical science that studies various types of anesthesia and anesthesia) has come a tremendous way in its development and today has everything necessary to ensure that any, even the most complex and extensive operation is painless, safe and comfortable for the patient. But even the most knowledgeable patient sometimes worries and asks a similar question: will it hurt me during and immediately after the operation, when the anesthesia wears off? The answer in this case may sound like this: if the anesthesiologist (a specialist in pain relief and monitoring the patient’s condition during surgery and in the immediate postoperative period) is a highly qualified specialist and performs his work professionally, there will be no pain during the operation and after the end of the surgical anesthesia.
What types of pain relief exist in modern medicine? What types of anesthesia are used for which operations?
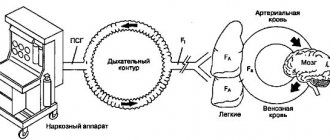
Pain relief or anesthesia can be general or local. For minor operations (in urology these are many operations on the penis and scrotal organs, in gynecology - minor interventions on the labia, vagina, area of the external urethral opening, etc.), local anesthesia . It consists of introducing a special substance, a local anesthetic (lidocaine, xylocaine, marcaine, etc.), using a syringe into the area of the operation being performed or into the area of the peripheral nerves that control the pain sensitivity of the operation area, which temporarily turns off the pain sensitivity. Local anesthesia can be infiltration (injection of an anesthetic directly into the area of incision and surgical manipulations), conduction (injection of an anesthetic into the area of large nerves that provide pain sensitivity in the operation area, but are themselves located outside this zone) and combined. During an operation under local anesthesia, the patient is conscious, he sees and hears everything that happens in the operating room, he can also feel all the touches of the surgeons (not pain), and sometimes experience minor pain. General anesthesia or anesthesia (the word anesthesia means only general anesthesia with the switching off of consciousness and pain sensitivity at the level of the brain, the colloquial expression “general anesthesia” is meaningless) consists of temporarily switching off the central zones of pain sensitivity and the transmission of pain impulses in the brain or spinal cord . Anesthesia can be intravenous or intubation. During intravenous anesthesia, a drug is injected into the patient’s vein, causing the pain sensitivity centers of the brain to be turned off and at the same time turning off the patient’s consciousness, usually maintaining spontaneous breathing. Intravenous anesthesia is used for minor and medium-sized operations when local anesthesia cannot provide adequate pain relief. This type of anesthesia is also used at the request of the patient, when he would not like to be conscious during the operation, to see, hear and feel everything that happens in the operating room. Intubation anesthesia consists of a preliminary temporary shutdown at the level of the brain of the patient’s central pain sensitivity and consciousness, temporary paralysis of the muscles, followed by intubation (insertion of a breathing tube into the trachea) and artificial ventilation of the lungs (artificial respiration) using special breathing equipment for the entire duration of the operation. This type of anesthesia is used for extensive operations on the abdominal and thoracic cavities, pelvic organs and retroperitoneal space (abdominal surgery). Such operations require that the patient's muscles are relaxed and involuntary or voluntary movements do not interfere with the surgeon and are completely excluded. Intubation anesthesia can also be used in cases where intravenous anesthesia or local anesthesia may be insufficient to provide the necessary pain relief and control the patient’s condition during medium-sized operations, as well as for medical reasons related to the presence of certain diseases of the person being operated on. A special place among methods of general anesthesia is occupied by spinal (epidural) anesthesia, which consists of the introduction into the spinal canal of local anesthetics of varying duration of action (lidocaine, xylocaine, marcaine, etc.), which leads to a temporary shutdown of pain and tactile sensitivity, as well as motor function below the injection site.
Spinal anesthesia is usually supplemented with so-called intravenous sedation (medication sleep) and the patient sleeps during the operation. This type of anesthesia is used for various operations on the pelvic organs and external genitalia.
What are the characteristics of the patient’s recovery from various types of anesthesia and the immediate postoperative period? What needs to be done to speed up the patient’s recovery and recovery after surgery?
Patients often wonder what will happen to them and how they will feel when the anesthesia wears off? Of course, this depends on the type of anesthesia used, and on the type and extent of the operation, as well as on the general condition and individual characteristics of the patient’s pain sensitivity. After the cessation of local anesthesia , after minor operations, patients, as a rule, experience slight pain in the area of the surgical wound (the site of the surgical injury cannot help but hurt). To eliminate these pains, it is usually enough to take a non-narcotic analgesic (painkiller) such as analgin, ibuprofen or diclofenac (Voltaren). If the effect of these drugs is not sufficient, more powerful non-narcotic analgesics are used - ketorol, tramadol, ketonal, etc. Typically, postoperative pain during minor and medium-sized operations lasts no more than 1-2 days. If they last longer, this should be brought to the attention of your doctor. After intravenous and intubation anesthesia , patients feel as if they were after a good and deep sleep, sometimes they remember bizarre dreams, occasionally experience a headache, note nausea, and in isolated cases vomiting. After intubation anesthesia, there is a soreness and discomfort in the throat, which is associated with the presence of a breathing tube there during the operation. Some medications used for these types of anesthesia can cause breathing problems. Therefore, in the first hours after surgery, patients are under close supervision of medical personnel of the anesthesiology service (anesthesiologist, nurse anesthetist). Only when there is complete confidence that there can be no breathing problems, the patient is transferred to a regular ward. After medium-sized, and especially after large abdominal operations, the patient may experience fairly intense pain for several days. In these cases, postoperative pain relief becomes a critical part of the patient's treatment in the first days after surgery. There are several postoperative pain relief regimens that are selected strictly individually and guarantee the patient’s comfortable condition in the first days after surgery. In the early postoperative period after major abdominal operations, in order to speed up the patient’s recovery and recovery, three main problems .
The first problem is pulmonary rehabilitation. It is often difficult for the patient to breathe deeply and move in bed. This can lead to pulmonary congestion and even post-operative pneumonia (pneumonia). To avoid this, the patient is placed with the head end slightly elevated, he is recommended to move in bed and regularly (every 1-2 hours) do breathing exercises (inhaling with resistance using a special spirometer or exhaling into a jar of water). The second common postoperative problem associated with prolonged lying down and lack of muscle activity is stagnation of blood in the veins of the legs , the formation of blood clots, which can travel through the veins to the heart and further into the pulmonary artery (thromboembolism) and cause sudden death. To prevent this formidable complication, the patient is given drugs that reduce blood clotting, and constant compression (squeezing) of the legs is also applied using an elastic bandage or, which is much better, simulating natural muscle activity, variable compression using a cuff of a special device. And finally, the third most important postoperative problem is rehabilitation of the digestive system . It is known that after major operations, especially on the abdominal and pelvic organs, there is a temporary decrease in intestinal peristalsis (contractility), which, as a rule, recovers on its own 2–3 days after surgery. To speed up this process, patients are advised to gradually return to their normal diet. On the first day after the operation, you are only allowed to drink water, on the second day you are allowed to consume liquid nutritious foods (jelly, jellies, broths), from the third day pureed boiled vegetables and minced lean meat (young beef) are added to the diet. The solution to all three main problems of the postoperative period is facilitated by early activation of the patient. We try to ensure that by the end of the first day after extensive abdominal operations, the patient sits in bed or in a chair, and by the end of the second day he gets up, washes himself and begins to walk around the ward. On days 3–4 after major abdominal operations, the vast majority of our patients begin to walk along the corridor of the department and prepare for discharge from the hospital.
Similar
Preparing for the injection
In order to minimize discomfort after intravenous anesthesia, we strongly recommend having a conversation with your doctor and anesthesiologist, who will answer all possible questions and talk about the nuances of treatment in your particular case. You should also avoid consuming food and liquids several hours before surgery and perform all necessary hygiene procedures. Doctors will definitely give all recommendations in advance.
An important point is premedication - preparing the patient for anesthesia and surgery using various medications. It is needed for:
- relieving tension, anxiety, fear, panic;
- pain relief;
- prevention of allergic reactions.
Before general anesthesia: preparation
Preparation for surgery under anesthesia has a great influence on the effectiveness and safety of general anesthesia and the course of the postoperative period. You will have to undergo a comprehensive diagnostic examination, including detailed blood tests, coagulogram, and ECG. According to indications, consultations with narrow specialists are prescribed.
The presence of chronic diseases of the respiratory and cardiovascular systems is of great importance. Be sure to tell your doctor about the following diseases:
- bronchial asthma;
- chronic obstructive bronchitis;
- arterial hypertension;
- IHD;
- history of stroke.
Do not under any circumstances hide the fact that you have a history of chronic diseases and acute vascular events (heart attack, stroke). Not only the outcome of the operation, but also your life depends on this! Also provide your doctor with a complete list of medications you take, including “harmless” analgesics for headaches or menstrual pain.
As practice shows, excess weight negatively affects the rate of recovery after operations under general anesthesia. If you are planning plastic surgery in advance, pay attention to weight loss issues. It is advisable to quit smoking in about six months. If you have not done this, stop smoking a week before the operation, but you should not “quit” the day before anesthesia - this may complicate the rehabilitation period.
On the eve of the operation, pay special attention to nutrition and hydration. You should not drink alcohol 24 hours before plastic surgery. On the day before surgery, you should limit yourself to breakfast and lunch. On the day of surgery, eating and drinking is strictly prohibited!