Fast Facts About General Anesthesia
Here are some key points about general anesthesia. More detailed and supporting information can be found in the main article.
- The anesthesiologist usually administers a general anesthetic before surgery
- There are some risks associated with the use of general anesthetics, but they are relatively safe when used correctly
- Very rarely, a patient may experience unintentional awakening during surgery
- Side effects of general anesthesia may include dizziness and nausea
- The mechanisms by which anesthesia works are still only partially understood.
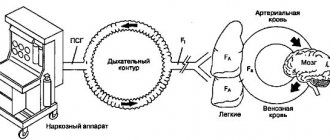
General anesthetics cause reversible loss of consciousness and analgesia necessary for surgery . The mechanism of action of anesthetics is not fully understood. There are several theories about this.
General anesthesia is essentially a medically induced coma, not sleep. Anesthetic drugs make the patient indifferent and turn off consciousness .
They are usually administered intravenously or by inhalation . Under anesthesia, the patient does not feel pain and may also experience amnesia.
The drugs will be administered by an anesthesiologist, who will also monitor the patient's vital signs during the procedure.
In this article, we'll look at a number of topics, including the possible side effects of general anesthesia, the risks involved, and some theories about how they work.
Contraindications for sedation
A permanent form of atrial fibrillation, coronary heart disease, hypertension, bronchial asthma, diabetes mellitus and many other chronic diseases are not a contraindication for dental treatment under sedation. On the contrary, constant hardware and clinical monitoring by an internist will allow timely medication to prevent pathological excess. By the way, monitoring and correcting the condition of a patient suffering from chronic illnesses during dental operations is the main point of the anesthesiologist’s participation in the treatment process. Medication-induced sleep may not be present as a component of the benefit.
Story
General anesthetics have been widely used in surgery since 1842, when Crawford Long prescribed diethyl ether to a patient and performed the first painless operation.
On October 16, 1846, American dentist and surgeon Thomas Morton first administered ether anesthesia to a patient to remove a submandibular tumor.
In Russia, the first operation under anesthesia was performed on February 7, 1847 by Pirogov’s friend at the professorial institute, Fyodor Inozemtsev.
Pirogov himself performed the operation using anesthesia a week later. Over the course of a year, 690 operations were performed under anesthesia in 13 cities of Russia, 300 of which were performed by Pirogov!
Soon he took part in military operations in the Caucasus. Here, for the first time in the history of medicine, he began to operate on the wounded with ether anesthesia. In total, the great surgeon performed about 10,000 operations under ether anesthesia.
Inhalation anesthesia
This is the most commonly used type of anesthesia, which is characterized by ease of implementation, relatively easy control and short duration of action, which is important for minor surgical interventions. Inhalation anesthesia is the administration of drugs through a mask, which ensures their entry into the organs of the respiratory system. Most often, Narcotan, nitrous oxide, Trilene, Ftorotan and Etran are used for this type of anesthesia. There is a certain problem - to achieve the desired result, it is necessary that the effect of anesthesia be deep, and this is fraught with serious complications. Therefore, this type of anesthesia is most often used in pediatric surgery. Children under anesthesia administered by inhalation feel excellent, they do not experience respiratory dysfunction, and complications are extremely rare.
Side effects
Nausea is a common side effect of general anesthesia.
There are a number of potential side effects of anesthesia.
Some people may experience none, others several. None of the side effects are particularly long-lasting and usually occur immediately after anesthesia.
Side effects of general anesthesia include:
- temporary confusion and memory loss, although this is more common in older people
- dizziness
- difficulty urinating
- bruising or soreness from the IV
- nausea and vomiting
- trembling and chills
- sore throat due to breathing tube
Risks
In general, general anesthesia is safe. Even very sick patients can be safely anesthetized. The surgical procedure itself involves much greater risk.
Modern general anesthesia is an incredibly safe procedure.
However, older adults and those undergoing lengthy procedures are most at risk for complications . These findings may include postoperative confusion , heart attack, pneumonia, and stroke.
Some specific conditions increase the risk for a patient undergoing general anesthesia, for example:
- obstructive sleep apnea, a condition in which people stop breathing while sleeping
- seizures
- existing heart, kidney or lung disease
- high blood pressure
- alcoholism
- smoking
- previous negative reactions to anesthesia
- medications that may increase bleeding - aspirin, warfarin , for example
- drug allergy
- diabetes
- obesity or overweight
Rehabilitation after the use of combined anesthesia
Modern anesthesia techniques require postoperative observation for approximately two hours. After completion of surgical treatment, under combined anesthesia, the patient is transferred to a specialized ward for dynamic observation. An hour or two after the end of sedation, the patient can perform almost all activities except driving, but this is a standard limitation. The patient may be sent home with an accompanying person. During the postoperative period, dental specialists should monitor the patient’s condition by regularly contacting him by telephone.
Unintentional intraoperative awakening
This refers to rare cases where patients report remaining conscious during surgery, long after the anesthetic should have taken effect . Some patients are aware of the procedure itself, and some may even feel pain.
Unintentional intraoperative awakening is incredibly rare, affecting approximately 1 in every 19,000 patients under general anesthesia.
Because of the muscle relaxants used at the same time as anesthesia, patients are unable to let their surgeon or anesthesiologist know that they still know what is happening.
Unintentional intraoperative awakening is more likely during emergency surgery.
Patients who experience unintentional intraoperative awakening may suffer from long-term psychological problems. Most often, awareness is short-lived and only sounds, and occurs before or at the very end of the procedure.
According to a recent large-scale study of this phenomenon, patients experienced involuntary twitching , stabbing pain, pain, paralysis and suffocation, among other sensations.
Because unintentional intraoperative awakening is rare, it is unclear exactly why it occurs.
Endotracheal anesthesia
One of the most commonly used methods of anesthesia when performing complex surgical interventions is endotracheal anesthesia, which involves immersing the body in a state of deep narcotic (medicinal) sleep. At the same time, the muscles completely relax, and the patient does not breathe independently. To achieve the desired state, doctors carry out a set of measures for the patient:
- Tracheal intubation is the insertion of an endotracheal tube into the lumen of the trachea, which is needed to provide artificial ventilation of the lungs.
- Intravenous administration of narcotic anesthetics, sedatives and tranquilizers.
- Administration of muscle relaxants – they block neuromuscular transmission.
- Artificial ventilation.
The quality of endotracheal anesthesia depends not only on the experience of the anesthesiologist, but also on how correctly the patient’s condition is monitored. It is imperative to monitor blood pressure, pulse, and oxygen saturation.
Types
There are three main types of anesthesia . General anesthesia is just one of them.
Local anesthesia is another option. It is done before minor surgeries such as toenail removal. This reduces pain in small, focused areas of the body, but the person receiving treatment remains conscious.
Regional anesthesia is another type. It numbs the entire part of the body - the lower half, for example, during childbirth. There are two main forms of regional anesthesia: spinal anesthesia and epidural anesthesia.
Spinal anesthesia is used for operations on the lower extremities and abdomen. The anesthetic is injected through a special very thin needle into the intervertebral space of the lumbar region . Epidural anesthesia is used for long-term pain relief. Can be used for operations on the chest, abdomen, and lower extremities. During an epidural, a thin plastic catheter is inserted through which a local anesthetic is injected. Pain relief can last as long as needed.
Local vs General
There are a number of reasons why general anesthesia may be chosen over local anesthesia.
This choice depends on age, health and personal preference.
The main reasons for choosing general anesthesia are:
- The procedure will likely take a long time.
- There is a possibility of significant blood loss.
- This may affect breathing, for example during breast surgery.
- The procedure will make the patient feel uncomfortable.
- It is difficult for the patient to maintain a forced position during surgery.
The purpose of general anesthesia is to induce:
- pain relief or elimination of the natural response to pain
- amnesia or memory loss
- immobility or elimination of motor reflexes
- dream
- relaxation of skeletal muscles
However, the use of general anesthesia poses a higher risk of complications than local anesthesia. If the surgery is minor, then the patient is offered local anesthesia, especially if he has a condition such as sleep apnea or other risk factors.
Preoperative assessment
Before undergoing general anesthesia, patients should undergo a preoperative assessment to determine the most appropriate medications, their amount and combination.
Some of the factors that should be examined in the preoperative assessment include:
- body mass index (BMI)
- disease history
- age
- medications taken
- time before anesthesia
- alcohol or drug use
- use of pharmaceuticals
- examination of the oral cavity, teeth and respiratory tract
- cervical spine mobility study
It is important that you answer these questions accurately. For example, if a history of alcohol or drug use is not mentioned, insufficient anesthesia may be given, which could lead to dangerously high blood pressure or unintentional intraoperative awakening.
Stages
The Gödel classification, developed by Arthur Ernest Gödel in 1937, describes four stages of anesthesia. Modern anesthetics and updated methods of drug have improved the speed of onset of anesthesia , overall safety and recovery, but the four stages remain essentially the same:
General anesthesia is similar to a comatose state and different from sleep.
Stage 1 or induction . This phase occurs between the administration of the drug and loss of consciousness. The patient moves from analgesia without amnesia to analgesia with amnesia.
Stage 2, or arousal stage . The period after loss of consciousness, characterized by agitated and delirious activity. Breathing and heart rate become erratic, and nausea, dilated pupils, and holding your breath may occur.
Due to irregular breathing and the risk of vomiting, there is a danger of suffocation. Modern fast-acting drugs are aimed at limiting the time spent on the 2nd stage of anesthesia.
Stage 3 or surgical anesthesia : muscles relax, vomiting stops, breathing is suppressed. Eye movements slow and then stop. The patient is ready for surgery
Stage 4, or overdose : if too much anesthetic has been administered, then depression of the brain stem occurs . This leads to respiratory and cardiovascular collapse.
The anesthesiologist's priority is to get the patient to stage 3 anesthesia as quickly as possible and keep him there throughout the operation.
How often can sedation be used?
During sedation, all the patient’s reflexes (cough, gag) are preserved, verbal contact is preserved: the doctor may ask you to follow simple commands like “open your mouth wider.” Sedation can be done as many times as you like. Every other day and every day. The drugs used to achieve sedation (no narcotic drugs are used) are eliminated from the body very quickly - within a few minutes. The anesthesiologist constantly adds them during the sedation process. A few minutes before the end of the operation, the administration of sedatives is stopped, and the patient wakes up on his own.