From this article you will learn:
- keloid scar and hypertrophic scar - what is the difference,
- laser resurfacing of scars: before and after photos, video,
- what is the best ointment for scars?
A keloid scar is the result of excessive growth of scar tissue. It looks like a hard, smooth, tough, nodular growth, often in various shades of red. Many people mistakenly refer to it as “colloidal scar,” which is a grammatically incorrect name.
Keloid scars (keloids) can begin to form immediately after injury or several months later. They can be significantly larger than the original wound itself. Unlike other types of scars, this type of scars/scars never lighten or become invisible over time.
Keloid scar: photo
They occur on any part of the body where there has been damage to the skin, but the following parts of the body are most susceptible to the formation of keloids: chest, shoulders, neck, knees, ankles, earlobes.
Keloid scar and hypertrophic scar - what is the difference?
Usually, after an injury, the body starts the healing process, as a result of which a regular flat scar forms on the surface of the skin (at the site of the former wound). For reasons still unknown to science, the scar may suddenly begin to thicken, i.e. hypertrophy of scar tissue occurs. Hypertrophy can be of two types, and depending on its type, either a hypertrophic scar or a keloid scar occurs.
- Hypertrophic scar (Fig. 7-9) - is formed if hypertrophy is limited to the area and size of the wound itself.
Most often, hypertrophic scars begin to develop within the first two months after injury, and quickly turn red. The growth occurs for up to 6 months, after which spontaneous regression usually occurs (it stops growing or even decreases slightly). This whole process usually takes 1 year, no more. Timely treatment (cortisone injections or steroids) can speed up the regression process. - Keloid scar (Fig. 1-6) - if the hypertrophy of scar tissue extends beyond the area of skin damage, capturing healthy undamaged tissue - such a scar is called keloid.
This type of scar develops over several years after injury, but can sometimes occur completely spontaneously even without previous injury, such as on the chest. A keloid scar can grow for many years and never regresses like a hypertrophic scar. Moreover, keloid scars often grow again if they were previously removed surgically. This never happens with hypertrophic scars (24stoma.ru).
Other symptoms of keloid scars are:
Keloid scars can be either flesh-colored or red, pink, or darker colors. They can be smooth, nodular or spherical, or simply protrude above the skin in lumps. If the keloid is exposed to sunlight during the first year of formation, the scar may permanently become darker than the surrounding skin. Sometimes a keloid scar will cause itching, irritation, or pain (and these symptoms may be worsened by rubbing clothing).
Scar treatment from the first days
In many clinics, scar treatment begins a few months later - after it has fully “ripened”. Of course, if the suture is applied correctly and you do not have a tendency to keloid scars, you can follow this advice, but even in this case it is necessary to properly care for the scar: use special silicone gels, avoid any mechanical trauma and irritation of the skin around the scar, do not sunbathe and carefully monitor the healing process. But it is still better to contact specialists who will carry out the necessary procedures and ensure that no complications arise that can lead to the formation of a rough scar.
In the first days, the following procedures may be prescribed:
- Preventive procedures - intravenous drip infusion of ozonized saline solution to saturate the blood with oxygen reduces the risk of pathological growth of connective tissue (keloid) by ten times or more,
- Rehabilitation procedures. Decongestant procedures and measures to restore microcirculation of blood and lymph: magnetic therapy, phonophoresis, microcurrent therapy, endermology, d'arsonval and cryotherapy.
To soften and absorb rough connective tissue, injections of collost, longidase, and diprospan are used. This effectively promotes the formation of the thinnest and most elastic scar possible.
Attention! Dangerous period!
Week 3-4 is characterized by an increased risk of fibrous tissue proliferation. This is often accompanied by itching and appears as a sudden proliferation of keloid cells. The scar quickly swells, thickens and turns red. At this time, it is necessary to take urgent measures to stop the avalanche-like growth of fibrous tissue and prevent the formation of a keloid scar.
Injections of special drugs and local irradiation of the scar with Bucca rays help stop this unwanted process and reverse it.
Keloid scars: causes of occurrence
During the wound healing process, fibroblasts begin to actively synthesize collagen. Sometimes, for some reason, fibroblasts begin to produce more collagen than is necessary for the normal wound healing process. In this case, the scar begins to grow, forming a keloid. According to studies, collagen synthesis in keloid scars is 20 times higher than in normal scars.
Keloids can develop from a variety of skin injuries, including - → surgical incisions, → wounds on the skin after injury, → vaccination injections, → acne (pimples and pimples), chicken pox, → piercings of various parts of the body (including piercings of the earlobes).
Scar treatment
The main priority of a plastic surgeon is an aesthetic and natural result, therefore our surgeons master new techniques and use minimal incisions or punctures to perform plastic surgery.
We analyzed the world experience of the best specialists and based on it we created our own suturing technique. Our clinic has the best rehabilitation program in Moscow, an important part of which is the treatment of scars and the prevention of pathologies in the development of connective tissue (the fight against keloid scars and fibrosis). We do everything so that the seam we apply is subsequently completely invisible.
Surgical removal of scars and scars –
It is much easier to prevent the appearance of keloid scars by using special ointments or silicone patches than to treat scars that have already appeared.
Surgical treatment consists of excision of the keloid scar using a scalpel or surgical laser. Surgical removal of scars with a laser should not be confused with the procedure of laser resurfacing of scars. The latter is a conservative non-surgical procedure. However, for keloid scars, surgical treatment methods are quite risky, because the operation may cause the formation of a similar or even larger keloid in the place of the previous one. Therefore, if excision is nevertheless used, then immediately after the operation all possible preventive measures are used to avoid relapse -
→ special ointments for scars, → corticosteroid drugs, → long-term wearing of a pressure bandage or compression garments after surgery.
Excision of a keloid using a surgical laser: video
Possible contraindications
Unfortunately, excision of keloid scars and neoplasms is not available to everyone. This is due to some contraindications, such as:
- Serious diseases of the cardiovascular system.
- Blood diseases, clotting disorders.
- The presence of inflammatory or infectious diseases in the acute stage.
- Age under 18 years.
- Pregnancy and lactation period.
Girls are not recommended to have excision of keloid scars and neoplasms during menstruation.
Non-surgical methods for treating keloids -
In addition to surgical treatment, there are other treatment options that can significantly reduce the size of the keloid and also make it lighter.
Laser resurfacing of scars –
This is one of the common methods of dealing with scars, not only keloids, but also hypertrophic ones. Typically, fractional lasers, argon laser, neodymium laser (YAG), CO2 lasers (carbon dioxide), pulsed dye lasers are used for this. Laser scar resurfacing helps make scars appear flatter and less red. The treatment is safe and not too painful, but several sessions are usually required.
The first video shows laser resurfacing of scars: before and after photos. The second video shows laser resurfacing of keloid scars, combined with steroid injections.
Corticosteroid injections –
Corticosteroids reduce excessive scarring through the following effects: → they reduce fibroblast proliferation and activity, → they reduce collagen synthesis, → they reduce the synthesis of glycosaminoglycans, → they reduce the synthesis of inflammatory mediators.
The most commonly used corticosteroid is triamcinolone acetonide (TAC) in a concentration of 10 to 40 mg. For best effectiveness, corticosteroids are used in combination with other scar removal methods (especially cryotherapy), which reduces the risk of recurrence by 50-100%.
Cryotherapy –
Liquid nitrogen causes cell damage. Typically, to achieve the desired effect, 1, 2 or 3 freeze-thaw cycles are carried out, each lasting 10-30 seconds. Repeat treatments may be required every 20-30 days. Studies have shown that the effectiveness of this method is 51-74% without relapse within 30 months of follow-up.
Possible side effects – → pain, → permanent depigmentation of the skin at the site of exposure.
Cryotherapy combined with steroid injections: video
Pressotherapy (pressure bandages) –
It has long been known that pressure has a thinning effect on the skin. A reduction in the number of collagen fibers in hypertrophic and keloid scars under pressure dressings has been demonstrated using electron microscopy data.
Compression treatments include point (button) compression, pressure bandages, elastic bandages, special silicone-based patches... Studies have shown that if you use silicone patches (Mepiform, Spenco) from the very beginning, it improves the condition of scars in 60% patients. However, such patches must be worn 24 hours for several months, which is difficult to maintain.
Scar ointment or scar cream –
Almost any modern ointment for resolving scars contains silicone, which (according to recent research) creates an airtight film, which perfectly moisturizes scars, gives them elasticity and softness. And this, in turn, is a good factor for normal healing and the formation of an unnoticeable flat scar.
Example of external remedies for scars -
- Dermatix (silicone + silicon dioxide) – in Fig. 10,
- Kelo-Kot (contains silicone + polysiloxane) – in Fig. 11,
- Zeraderm ultra (silicone + vitamins E and K + coenzyme Q10 + UV filter 15)
- Skargard (silicone + hydrocortisone + vitamin E),
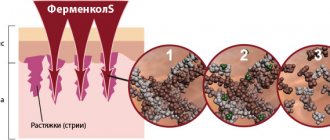
- Fermenkol (contains collagenase of animal origin).
- Contractubex (contains sodium heparin + onion extract + allantoin),
- silicone patches Mepiform, Dermatix, etc. (Fig. 12).
You should start using ointment for scars after surgery only after the suture has healed, that is, the crusts have completely fallen off. Until this time, the crusts can be lubricated with Panthenol, D-Panthenol, Dexpanthenol or other similar products. Keep in mind that under no circumstances should you pick out the crusts yourself; they should fall off on their own!
Preparation
Before the operation, special preparation and examination are required. The patient will need to undergo the following tests:
- General blood and urine analysis.
- Blood test for HIV, hepatitis, syphilis.
- ECG.
- Fluorography.
- If you have chronic diseases, you may need to consult a specialist.
You should also read the following recommendations:
- The operation is performed on an empty stomach, so you should refrain from eating at least 7 hours before the procedure.
- You need to give up alcohol 3-5 days in advance, and on the day of surgery you should limit smoking.
- Tell your doctor about any medications you take on a regular basis. Drugs that affect blood clotting may be discontinued several days before the procedure.
- Nutrition before and after surgery should be balanced, containing the required amount of vitamins and microelements, this will significantly speed up the process of tissue regeneration.
What types of laser are used
To correct grossly healed tissue, cosmetologists use three types of devices:
- Erbium laser - used for classic skin smoothing by evaporating fluid from cells.
- Neodymium laser is the safest, as it allows you to carefully smooth out the scar area.
- Fractional carbon dioxide laser - creates a network of microbeams that evaporate moisture in a targeted manner.
The combined use of such equipment is common. Watching a video about removing keloid scars with each type of laser allows you to understand the difference in the principle of their action.
Collotherapy
Gel Collost is a high-tech biological material, namely collagen of the first type with a completely preserved structure. The drug activates tissue regeneration in the affected area, triggering the formation of new collagen fibers and the replacement of scar tissue with healthy ones. Collost therapy significantly reduces the severity of scars, making them almost invisible.
Correction of scars with Collost is performed in a course of 3-5 procedures, maintaining an interval of two weeks between them. It is especially effective when used with laser resurfacing of the scar area.
How many sessions will it take?
The number of procedures for which it will be possible to completely remove keloid scars with a laser is determined individually. Several factors matter:
- scar size;
- the severity of overgrown tissues;
- the area where the keloid is located;
- time that has passed since the injury occurred.
To get rid of the defect, a course of 2-10 laser therapy sessions is required. Between procedures, cosmetologists prescribe a recovery period of about 1 month, during which the patient follows skin care measures.