Breast cancer is the most common cancer in women in the world. In Russia, this type of cancer accounts for 20.9% of all malignant diseases. In 2015, more than 66,600 new cases of breast cancer were identified in the country, and the incidence rate was 49.75 per 100,000 population.
Advances in surgery, pharmacology, diagnostic methods, and new knowledge about breast cancer have increased the chances of detecting a tumor at an early stage. Thanks to this, surgical treatment of the disease with preservation of the mammary glands has become much more common. The tactics of examining patients after primary treatment are also changing - now it helps to most effectively and promptly identify possible relapses.
The number of patients who have undergone primary treatment and are under dynamic control is increasing every year. This is why breast cancer recurrence and methods of preventing it are becoming increasingly discussed medical topics.
Recurrence of the disease must be diagnosed at an early stage. Actively monitoring patients helps reduce the risk of relapse and determine the most effective treatment if it does occur. In addition, the recurrence of the disease can be prevented by proper prevention.
Follow-up after breast cancer treatment
In the first 5 years after primary cancer treatment, the risk of breast cancer recurrence is greatest. Therefore, during this period it is necessary to visit the oncologist 1 to 4 times a year (depending on the specific clinical situation). During the appointment, the doctor examines the patient and identifies possible complaints. After 5 years, it is advised to contact a specialist once a year, unless, of course, there are any complaints about the condition.
During the appointment, in addition to the examination, the oncologist will prescribe instrumental research methods that will allow timely detection of breast cancer recurrence or progression of the disease:
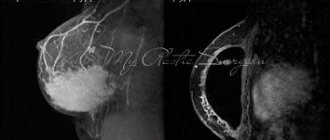
- bilateral (in the case of organ-preserving surgery) or contralateral mammography in combination with ultrasound of regional zones and the area of the postoperative scar - once a year;
- scintigraphy of skeletal bones, ultrasound of the abdominal and pelvic organs, radiography of the chest organs - as prescribed by the oncologist.
In addition, women taking adjuvant tamoxifen in the presence of a intact uterus should undergo a routine examination by a gynecologist annually. The fact is that the drug can cause the development of endometrial hyperplasia, and a specialist will notice this in time.
Women taking aromatase inhibitors for a long time are recommended to undergo annual densitometry. This diagnostic method helps assess bone density and the risk of developing osteoporosis.
Caring for sutures after fibroadenoma removal
The leading complaint after surgery is chest pain at the site of the intervention, which will gradually disappear, but in the first day the woman will need pain relief.
Upon completion of the operation, a bandage is applied to the gland - a gauze sticker. Dressing is usually carried out daily until the wound is completely healed and the stitches are removed. The stitches will be removed in a week or a week and a half on an outpatient basis.
Before the stitches on the chest are completely removed, the wound is treated with an antiseptic solution; there is no need for ointments or powders.
Sutures will be removed only if there is no divergence of the edges of the wound, so the period for their removal varies individually - from 7 to 10 days. After removing the suture, a bandage is not needed. You cannot tear the scab off the wound; a shower will help the scabs come off.
A month after the operation, a doctor’s examination and an ultrasound of the mammary gland are necessary, the next visit to a mammologist is six months later.
For the fastest healing of postoperative wounds and improvement of well-being, rehabilitation programs using physical factors and modern devices and special medications are recommended. Patients undergo correction of hormonal status to prevent relapse and other pathological conditions of the mammary gland.
Book a consultation 24 hours a day
+7+7+78
Bibliography:
- Vysotskaya I.V., Letyagin V.P., Cherenkov V.G. et al/ Clinical recommendations of the Russian Society of Oncomammologists for the prevention of breast cancer, differential diagnosis, treatment of precancerous and benign diseases of the mammary glands // Tumors of the female reproductive system, 2016, 3, T.12
- Lakhani SR, Ellis IO, Schnitt SJ, et al. /WHO classification of tumors of the breast. IARC//World health organization classification of tumors; Lyon, France: WHO Press; 2012.
- Berg VA, Blum DD, Kormak DB, et al./ Combined screening of ultrasound and mammography compared with only mammography of women with an increased risk of breast cancer // 2013 August, 14; 299(18).
- McCavert M., Odonnel M.E., Aruri S., et al./ Ultrasound is a useful addition to mammography in the evaluation of breast tumors in all patients// International Journal of Clinical Practice; November 2009; 63 (11).
- Hung VK, Chan SVV, Suen DTK, et al. /Referral to the clinic for specialists mammologists// Surgical Journal; 2014, May; 70 (3).
Why do relapses occur after mastectomy?
Recurrence of breast cancer after mastectomy in a postoperative scar can occur as a result of poor-quality treatment, chemotherapy, or incomplete tumor removal.
Period when relapses may occur after treatment
The first 10 years after initial treatment are considered the most dangerous for the development of local relapses. Moreover, more than half of cases of recurrent disease occur in the first 5 years. The task of patients during this period is to immediately contact an oncologist if there is any suspicion of a relapse. It is necessary to conduct an independent examination of the breast and postoperative scar, as well as know your risk group and the main symptoms of relapses.
Risk groups for breast cancer recurrence
The likelihood of breast cancer recurrence after mastectomy depends on the following factors:
- the presence of metastases in regional lymph nodes;
- molecular genetic profile of the tumor (presence of receptors for estrogen and epidermal growth factor HER/2neu);
- size of the primary tumor;
- patient's age. Breast cancer relapse occurs more often in young patients.
In this regard, there are 3 risk groups.
High risk
- metastases in 1-3 lymph nodes in the absence of HER2/neu overexpression in the tumor;
- metastases in 1-3 lymph nodes in the presence of overexpression;
- HER2/neu in tumor;
- metastases in 4 lymph nodes or more.
Medium risk
The absence of metastases in the lymph nodes in combination with at least one of the following signs:
- tumor size more than 2 cm;
- degree of malignancy 2-3;
- presence of vascular invasion;
- the presence of HER2/neu overexpression in the tumor;
- age less than 35 years.
Low risk
Absence of metastases in the lymph nodes in combination with all of the following:
- tumor size less than 2 cm;
- tumor grade 1 (low);
- no vascular invasion;
- no overexpression of HER2/neu;
- age over 35 years.
How to treat sutures and wounds after a mastectomy at home
To treat sutures and wounds after mastectomy surgery at home, use antiseptics (solution of iodine, brilliant green, potassium permanganate, Chlorhexidine, Miramistin, Dioxidin), ointments (Kontraktubeks, Eplan, Levomekol).
General rules of care after breast removal
After removal of the mammary gland, you must follow the general rules of care:
- inspect the postoperative suture daily, and if any discharge, swelling or redness of the skin appears, see a doctor;
- treat the wound site 2-3 times a day with an antiseptic liquid, it can be alcohol, Chlorhexidine, iodine, brilliant green, pink solution of potassium permanganate, Furacilin, Dioxidin, Miramistin as prescribed by the surgeon;
- apply a sterile bandage.
From the time the dry crusts come off, you need to lubricate the scar with creams, gels and ointments. This helps speed up healing and prevent the formation of too dense tissue. The surgeon may recommend: Actovegin, Solcoseryl, Vulnuzan, Levomekol, Contractubex, Stellanin . The choice of specific drugs remains with the specialist, since upon discharge he determines the stage of healing and the risks of complications.
We recommend reading about breast lift. You will learn about the advantages of this operation, its methodology, indications and contraindications, rehabilitation period, results and price. And here is more information about complications after mammoplasty.
Application of Contractubex on sutures
Contractubex is applied to a formed scar after the sutures are removed and the dense crusts come off . Its properties:
- inhibits the increased proliferation of coarse connective tissue;
- relieves inflammation, irritation and allergies;
- inhibits the growth of bacteria;
- softens;
- soothes itching;
- smoothes the skin.
The drug stimulates healing and at the same time prevents the formation of a keloid, dense scar. Apply 2 times a day with gentle, gentle rubbing into the seam. Treatment lasts from several weeks to 2-4 months.
How to treat the breast if an absorbable suture is applied after surgery
If after the operation a suture is placed with absorbable threads, then antiseptics are used when treating the breast - Chlorhexidine, Miramistin, Dioxidine. When a scar is formed, it is recommended to lubricate it with ointments with a softening and wound-healing effect: Dermatix, Eplan. The basic rules for caring for a postoperative wound do not change, but the threads will not need to be removed.
Symptoms of relapse
To detect recurrence of breast cancer in a timely manner, it is necessary to regularly visit an oncologist and undergo examinations. However, it is equally important to independently monitor the condition of the chest and mammary glands.
Symptoms of cancer returning may not be obvious. Regular breast examination and understanding of its normal condition will help to identify unwanted changes as early as possible and begin treatment.
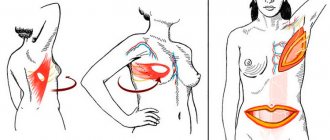
Among the most common symptoms of breast cancer recurrence are:
- the appearance of a lump under the skin of the mammary gland (during organ-preserving surgery) or in the area of a postoperative scar;
- change in the structure of breast tissue (during organ-preserving surgery);
- recurrence of breast cancer in a postoperative scar can cause a change in skin color in the scar area (redness).
If you notice signs of breast cancer recurrence, you should immediately contact an oncologist.
What foods should you eat to help your stitches heal faster after breast surgery?
To speed up the healing of sutures after breast surgery, you need to eat foods containing:
- protein – cottage cheese, fish, chicken, turkey;
- collagen – berry, fruit jelly, jellied meat;
- vitamin C – sea buckthorn berries, black currants, bell peppers, kiwi;
- vitamin A and provitamin carotene – carrots, liver, parsley, tuna, yolk;
- zinc – pine nuts, peanuts, beans, oatmeal.
Diagnosis for suspected recurrence of breast cancer
If you suspect a relapse, you should immediately consult a doctor. The specialist will conduct diagnostics: examination, palpation, mammography, prescribe ultrasound of the postoperative scar and regional areas and morphological (cytological and histological) examination.
Morphological examination of a recurrent tumor should be carried out similarly to the diagnosis of a primary tumor, including the determination of estrogen receptors (ER), progesterone receptors (RP), HER2/neu, Ki67. Based on the data obtained, further tactics and treatment methods will be determined. If necessary, the oncologist will prescribe additional studies and tests.
How long after breast surgery can the suture be wetted?
It is possible to wet the suture after breast surgery only after a while - usually on the 2-3rd day, since the drainage must be removed. The doctor may then allow the patient to take a warm shower, but the wound must be covered with a bandage. The water temperature should be moderately warm; it is better to use regular baby soap or gel with a neutral pH.
It is important to consider that if there are signs of inflammation, surgeons prohibit water procedures; then you should wipe the body with wet wipes in the area of the mammary glands. Bathing is not recommended for at least 1 month.
Prevention of recurrence of the disease
After a long and difficult treatment, all patients are interested in the question “how to avoid recurrence of breast cancer.” The following methods help prevent recurrence after breast cancer or reduce its risks:
- comprehensive treatment in accordance with international standards;
- for hormone-positive cancer, long-term use of tamoxifen/aromatase inhibitors;
- dynamic observation after completion of the main stage of treatment;
- prevention with agents based on indole-3-carbinol and epigallocatechin-3-galate (Promisan) to restore the activity of tumor-suppressing genes (the gene whose product ensures the prevention of tumor transformation of cells) and BRCA proteins.
In addition to regular monitoring by specialists and systemic therapy, a healthy lifestyle will help prevent breast cancer recurrence. Walking in the fresh air, physical activity, and proper nutrition are the basis of any person’s health. But this is especially important for those who have suffered a serious illness.
You also need to maintain your weight at an optimal level. The fact is that excess adipose tissue is a source of estrogen production. It has been proven that excessive estrogen stimulation negatively affects breast tissue, stimulating the development of proliferative processes. Thus, reducing excess estrogen stimulation also leads to a reduction in the risk of relapse, especially for hormone-dependent types of breast cancer.
Complications during suture healing
With a high-quality operation and good care after it, negative consequences in the suture area are rarely detected. But each organism is unique, in addition, anesthesia and the intervention itself provoke some suppression of the immune system. Therefore, complications cannot be 100% excluded:
- Inflammation . It can occur due to bacteria entering the wound, as well as from the body’s rejection of implants. If the seam is red, swollen and the area around it hurts, this is an alarming sign. Most likely, you will need treatment with antibiotics, possibly dissection, washing the wound and re-fixing the edges of the injured tissue.
- Sometimes you have to remove the implants, undergo treatment and perform the operation again. If after 2 weeks swelling in the suture area persists or reappears, the temperature rises, pain occurs in the problem area and head, the incision oozes purulent fluid and blood, you should definitely consult a doctor.
- Formation of a hypertrophic or keloid scar . Complications can develop due to insufficient care. But sometimes the culprit is a feature of the body that was not previously detected because the woman had not previously undergone surgery at all. Thin, almost imperceptible stripes remain after the intervention for everyone. But hypertrophy must be treated, sometimes surgically.
- Seroma . It can occur not only in the immediate vicinity of the implant, but also in the suture area. Then serous fluid is released from it. If you don't take action, it's not far from here to inflammation.
- Seam divergence . This problem is also not difficult to notice yourself. If the suture breaks after mammoplasty, you need to see a doctor as soon as possible. Until his help arrives, the area of tissue damage should be treated with an antiseptic (iodine or brilliant green).
The seam hurts, pulls, tingles - is this normal?
If the suture pulls or tingles, or there is pain, this means that the healing process is taking place. These symptoms are not cause for concern if:
- localized only in the wound area;
- gradual subsidence of pain;
- reducing swelling;
- absence of fever, headache, chills, twitching pain;
- availability in the first weeks.
Moderate pain occurs for at least 2 months, but in some women it is felt in the first six months after surgery.
The seams do not heal
If the sutures do not fuse after surgery, it is recommended:
- wear special adhesive plasters that hold the edges of the wound - strips (you may need to stick them on for several months);
- wear retaining underwear for at least 4-6 weeks;
- include protein products in the menu (chicken, fish, turkey, cottage cheese), gelatin-based jelly, fruits and berries with vitamin C - sea buckthorn, rose hips, citrus fruits;
- do not allow the seam to get wet, dry thoroughly after water procedures;
- apply ointments with a wound-healing effect - Solcoseryl, Contractubex.
Suture oozing after mammoplasty
The suture after mammoplasty may ooze, that is, there is always a discharge of clear or slightly yellowish liquid on its surface. This symptom may be the first sign of seroma. This is the name for the accumulation of fluid in the area of contact between the gland tissue and the implant. It consists of the plasma part of the blood; with a small size and good outflow, it resolves on its own.
If there is no drainage, the patient does not wear shapewear, and puts pressure on the shoulder girdle, then the seroma increases. This causes severe pain and fever. In this case, a visit to the surgeon is required. It will help remove accumulated fluid. The procedure takes place under local anesthesia and does not affect the result of mammoplasty.
Watch this video about complications after breast augmentation:
What are the dangers of pus on the suture after surgery?
Pus on the suture after surgery threatens the development of inflammation. Its signs:
- after a week the pain does not subside, but intensifies;
- the wound and the skin adjacent to it are swollen, red, hot;
- headache, fever, and weakness occurred.
Antibiotics are prescribed for treatment, but this should only be done by a surgeon after examining the wound. In some cases, it is necessary to allow the outflow of pus; installation of drainage (tube or elastic band) will be required.
There is also this option - the wound healed normally, but after a few weeks (sometimes months and even years) swelling and a red polka dot appeared on the seam. It matures and opens with the release of pus. This happens when the suture material remaining in the wound is rejected (ligature fistula). If it comes out with pus on its own, then complete healing occurs. But perhaps surgical help will be needed. When surgery is not required, the following is prescribed:
- lotions with saline solution (10 g per 100 ml of water, boil and filter through sterile gauze, bandage in 6 layers);
- applications of ointment with ichthyol;
- washing with antiseptics (for example, Dioxidin), enzymes (Chymotrypsin).
After the suture material appears, it is removed and the wound is treated with antimicrobial agents.
Expert opinion
Tatyana Somoilova
Cosmetology expert
In all cases of suppuration or fever, you should urgently consult a surgeon. Self-medication is strictly prohibited.
What does it mean if the seam turns red after breast removal?
If after removal of the mammary gland the seam turns red, this means:
- Option for normal healing in the first 2-3 weeks, the suture requires observation and treatment.
- Infection when there is swelling, pain and fever. It is caused by the penetration of bacteria into the wound or the introduction of blood from the site of a chronic process (for example, the nasopharynx). One of the common options is erysipelas. Examination by a surgeon and antibiotic therapy are recommended.
- Relapse of the tumor process, which occurs after 8-12 months, is accompanied by enlarged lymph nodes, lumps in the chest, severe weakness, fever, pain in the gland, bones, and joints.
Risk of breast cancer recurrence
Why does the seam on the mammary gland darken?
The seam on the mammary gland may darken for the following reasons:
- formation of normal scar tissue;
- vascular sprouting (hypertrophic scar);
- healing with the proliferation of connective tissue and the formation of a rough keloid.
In the latter case, this is accompanied by the risk of a significant cosmetic defect. The main symptom is the spread of scar tissue beyond the postoperative wound. At the same time, patients feel itching in the suture area, and there is pain when pressing. For treatment, creams with silicone (Dermatix, Kelocode), laser therapy, and liquid nitrogen treatment are used.
A hypertrophic scar resolves over time, but usually this happens within a year . You can speed up the process by using:
- laser resurfacing;
- local hormone injections;
- ultrasonic treatment with Contractubex, Hydrocortisone;
- Lidase electrophoresis.
Why do stitches take so long to get wet after a mastectomy?
The main reason for the long healing of the suture after a mastectomy and the weeping surface of the wound is low immunity. It accompanies tumor processes and weakens as a result of taking cytostatic drugs, hormones, and radiation therapy. Risk factors are also considered:
- diabetes;
- obesity;
- age after 40 years;
- smoking;
- food lacking protein and vitamins;
- hot and humid weather;
- circulatory disorders.
It is important to consider that weeping wounds are a gateway for infection. It is recommended to dry them; for this, the surgeon may recommend:
- lubricate with iodine, brilliant green;
- treat with a mixture of calendula tincture and chloramphenicol;
- sprinkle with Baneocin powder.
Ointment bases can enhance separation, so only gels are applied (for example, Solcoseryl). If there is redness, severe itching or burning, or fever, you should immediately consult a doctor.
Redness around the stitch
Redness of the skin surrounding the suture occurs during an inflammatory reaction. If this happens in the first week, and the pain and swelling do not become stronger, then this requires continuation of the prescribed treatment - treatment with antiseptics, antibacterial ointments, wearing compression garments.
If redness appears some time after initial healing, there is swelling and an increase in local, general temperature, then this means infection has entered the wound. It can come from the outside or from a source of chronic inflammation in the body. You should consult a surgeon to determine the condition of the wound and the advisability of using antibiotics.
Why is the suture hard after surgery?
The suture after surgery may become hard due to the accumulation of blood under the skin (hematoma) or compaction due to inflammation. In the first case, there is usually no pronounced temperature reaction, but pressure on the seam is painful. For resorption, ointments with heparin and Lidaza are used locally.
If there are signs of an inflammatory reaction (red and hot skin, swelling, elevated body temperature), local therapy with antibiotics, their administration by injection, or taking tablets is prescribed. In case of compaction of any origin, surgical treatment of the wound may be required - drainage to ensure the outflow of accumulated fluid (inflammatory exudate or blood).
Yellow fluid is oozing from the seam
If the yellow liquid released from the suture is transparent, then this is a sign of seroma. This is the name for the accumulation of the plasma part of the blood, lymph. It may also contain a small admixture of blood from injured vessels.
After mammoplasty, it is often a reaction to the installed implant, suture material, and during mastectomy it is associated with an abundance of lymphatic pathways, which are inevitably damaged during the operation. Treatment requires fluid drainage and drainage installation. Sometimes seroma resolves on its own.
If the liquid is yellow, thick with a greenish tint, then it is pus. Its separation from the seam is a sign of microbial penetration. In such cases, an urgent visit to the surgeon is needed to determine treatment tactics - antibiotics or wound treatment followed by anti-inflammatory therapy. The purulent process does not disappear without treatment, but only spreads.
Blood from the suture after surgery
The appearance of blood from the suture after surgery occurs when the vessel is damaged or the clotting ability is reduced. If the bleeding is slight and there is no pain, then local use of a hemostatic sponge is recommended. Severe bleeding will require surgery. An urgent examination by a doctor is needed if there are signs of inflammation during blood discharge - redness, swelling, twitching pain in the suture area, temperature.
Consultations: ask a question
ONLINE consultation with Vitaly Aleksandrovich Skvortsov >link>
Get a QUICK ANSWER to your question from Dr. Skvortsov >link>
The questions are answered by the winner of the nomination “BEST ONCOLOGIST” Vitaly Aleksandrovich Skvortsov , doctor of the highest category of the State Clinical Clinical Oncology Department, kmn, oncologist surgeon, mammologist, plastic surgeon
HOW TO ASK A QUESTION CORRECTLY >link>
Hemoglobin dropped sharply
QUESTION: Doctor, my mother’s hemoglobin dropped sharply after a mastectomy. What do you recommend? How to raise it? And what caused this? Thank you. ANSWER: Hello! How long ago was the operation? Your mother, most likely, if she recently had surgery, has a hematoma after lymph puncture! Contact the surgeon who performed the operation! Has hemoglobin dropped significantly? He shouldn't fall like that!
Hemoglobin
QUESTION: Vitaly Alexandrovich, I asked you a question about my mother, whose hemoglobin dropped after a mastectomy. 12 days have passed since the operation, hemoglobin is 80. Thank you. ANSWER: Hello! Most likely, your mother was bleeding! But 80 is not enough, we must definitely raise it!
Breast removal
QUESTION: Vitaly Alexandrovich, are the emotional needs of the patient taken into account when deciding to remove the mammary gland? ANSWER: Hello! Many factors are taken into account: from the type of tumor, from the person and his adequate response to the situation, from the future lifestyle! Everything is taken into account! How could we do without this?
Mammary cancer
QUESTION: Vitaly Alexandrovich, does preventive mastectomy—breast removal—increase survival? If it increases, then for what molecular subtypes of cancer? ANSWER: Hello! Of course, you can argue that no gland and no cancer, increasing survival rates! Typically, prophylactic mastectomy is done for Brca1,2,3,4 mutations! But in our country, prophylactic mastectomy is not yet widely used!
How many lymph nodes are removed during a mastectomy?
QUESTION: Vitaly Alexandrovich, how many lymph nodes are removed during a mastectomy? ANSWER: Hello! During a standard operation according to Madden and Patty, 3 levels of lymph nodes in the axillary region are removed - for some it may be 10 lymph nodes, and for others 20 or more.
First shower after mastectomy
QUESTION: Vitaly Alexandrovich, when can you take your first shower after a mastectomy? ANSWER: Hello! The answer is when the doctor allows it, usually after the drainage is removed!
Exercise after breast cancer
QUESTION: Vitaly Alexandrovich, what physical activity is acceptable after a mastectomy? Thank you. ANSWER: Hello! There are loads, but they are dosed. You can read more details in my article on the website. Rehabilitation after breast removal
Dressings after mastectomy
QUESTION: Vitaly Alexandrovich, how long should dressings be done after a mastectomy? ANSWER: Hello! This period is different for everyone, while lymphorrhea lasts, this is normal during a mastectomy. On average 1.5-2 months.
seam seal
QUESTION: Hello, Vitaly Alexandrovich! My question is, 2 months after the mastectomy, my suture became thicker and reddened. Very dense in some areas. Previously there was a thin seam. What could this be and what should I do? ANSWER: Hello! Most often this is a healing process! Up to 6 months it becomes denser, and then vice versa. Red because now it is sprouting vessels and it’s like a reaction! Sometimes inflammation occurs after 2 months, but usually it goes away after local dressings!
Reconstruction of the arm after mastectomy.
QUESTION: Vitaly Alexandrovich, almost 6 months have passed since the mastectomy and my arm is still limited in mobility. What will you advice me? ANSWER: There can be many reasons for this. Do you do exercises and a set of exercises for recovery? We need to look at you, come for a consultation and we will solve this issue! I think it will be useful for you to read my article about how to live after a mastectomy. https://www.skvorsov.ru/blog-breast-cancer/reabilitatsiya-posle-udaleniya-grudi
Pain after mastectomy
QUESTION: Doctor, my mother has had 4 months since her mastectomy, but she still feels pain in the operated area. How normal is this? And how long does the recovery process take? Thank you. ANSWER: Hello! This is normal and natural, you can read in detail on my website information about recovery and pain! We are all different and everyone’s pain lasts differently! I hope everything gets better for your mom soon. On average, pain can last 6 months! https://www.skvorsov.ru/blog-breast-cancer/reabilitatsiya-posle-udaleniya-grudi
Ring after mastectomy
QUESTION: Vitaly Alexandrovich, is it possible to wear jewelry on the operated side after a mastectomy. I mean bracelets on the hand or rings on the fingers. Or it's better not to do this. Thank you. ANSWER: Hello! Of course you can wear jewelry. If you have symptoms of lymphadenitis, then you will not be able to put on the ring, but if you do not have signs of hand swelling, then wear it without problems!
Lymphorrhea after mastectomy
QUESTION: Vitaly Alexandrovich, is there always lymphorrhea after a mastectomy? Is this considered normal? And how long can it last? Thank you. ANSWER: Hello, this is the norm and natural! It lasts differently for everyone - from a month to 3-4 months!
Suture hurts after mastectomy
QUESTION: Vitaly Alexandrovich, 3 months have passed since the mastectomy and the stitch still hurts. Is this a normal option? And this place is still numb. ANSWER: Hello! This is the norm in your case! This is all related to the operation and soon all symptoms should disappear!
Swelling after mastectomy
QUESTION: Vitaly Alexandrovich, I am worried about swelling after a mastectomy. The operation took place 2 months ago. Do I have cause for concern? Thanks a lot. ANSWER: Hello, you have no reason to worry, this is a natural normal process after a mastectomy.
Lymphorrhea after mastectomy
QUESTION: Vitaly Alexandrovich, are there any ways to reduce lymphorrhea after a mastectomy? Thank you. ANSWER: Hello! Surgeons have been trying to combat this problem for many years and, unfortunately, nothing has been invented, only punctures! This process usually goes away later!
Lymphorrhea
QUESTION: Vitaly Alexandrovich, what will happen if the fluid that forms during lymphorrhea is not pumped out? Thank you. ANSWER: Hello, liquid will accumulate under the skin and this will cause discomfort, and the worst thing is that the wound may become inflamed and suppurate!
Arm pain after mastectomy
QUESTION: Vitaly Alexandrovich, more than two months have passed since the mastectomy, but I am still bothered by pain in my arm. How to relieve this arm pain after mastectomy? Thank you. ANSWER: Hello! Pain is a natural state in this case, it can be reduced by taking painkillers! This pain will soon be less!
Sick leave after mastectomy
QUESTION: Vitaly Alexandrovich, for how long is sick leave given after a mastectomy? Thank you. ANSWER: Hello! Usually, a sick leave certificate is given by the attending physician in a hospital and in a clinic at the place of residence, and it is given for the period that is necessary, this period is unlimited!
Mastectomy
QUESTION: Vitaly Alexandrovich, what is a Madden mastectomy? ANSWER: Hello, this is removal of the breast with lymph nodes of all levels in the axillary region for breast cancer!
Compression sleeve after mastectomy
QUESTION: Vitaly Alexandrovich, how long after a mastectomy should I start wearing a compression sleeve? Thank you. ANSWER: Hello! It is not necessary to wear a sleeve after a mastectomy; it is necessary to wear it only if any complications arise, for example, lymphedema!
Chemotherapy
QUESTION: Is it necessary to prepare the body for chemotherapy, when to start and how? ANSWER: Hello, there is no such need, since our body is ready for anything!
Mastectomy
QUESTION: Vitaly Alexandrovich, are there any ways to somehow reduce the secretion of serous and lymphatic fluid after a mastectomy? And what is this process called? The drainage has been in place for the seventh day and a lot of fluid is still accumulating - sometimes less, sometimes more! ANSWER: Hello! I’ll honestly tell you that this problem is hanging in the air and no one knows how to solve it!!! There are many methods for stopping lymphorrhea, as this process is called, but they are all ineffective and lymph still continues to accumulate in the armpit area, but only time stops this process, which on average lasts about 1-2 months! Some surgeons sew flaps of skin to the chest in the axillary region, some inject solutions into this area, but I repeat that this is all pointless! Don't trust anyone who promises otherwise! Everything will pass for you soon, be patient!
Blood in fluid after surgery
QUESTION: Good afternoon! For the second week after a mastectomy, my mother’s drainage has accumulated fluid and blood, the blood is dark, is this normal? Is it possible to remove the drainage if there is little fluid, but there is blood in it. If so, where will this blood go after the drainage is removed? ANSWER: Hello, the question of removing the drainage is decided by her surgeon, it can be from 5 days to 15 days! This is not blood, but ichor, and if it is old blood, then it was a small hematoma under the skin, this happens often and is, in principle, normal! When the drainage is removed, the blood is lysed (the clot will dissolve) and punctures through a needle will remove it all over time!
Histology and immunohistochemistry after mastectomy
QUESTION: Vitaly Alexandrovich, how does histology differ from immunohistochemistry after mastectomy? ANSWER: Hello! Fundamentally different!! Histology is the structure of the tumor, what type of cancer and the damage to the lymph nodes is assessed. Immunohistochemistry is an analysis of the same tumor, which tells how to treat this tumor! Is this studying tumor cell receptors? This is in short words for the average non-medical person!
Suture after mastectomy
QUESTION: Vitaly Alexandrovich, what can you recommend to make the suture after a mastectomy less noticeable. Or is there any special care for the suture immediately after a mastectomy? Thank you. ANSWER: Hello! No special care! The healing process of wounds and sutures depends on you, everyone has different regenerative capabilities, you cannot improve this situation with any ointments! The healing process takes up to 6 months! There are special silicone-based bandages, this is the only way to somehow make the seam less noticeable!
Suture after mastectomy
QUESTION: Vitaly Alexandrovich, good evening! Thank you for your answers to the questions. I have a question for you about the suture after a mastectomy. Maybe you can advise how to make it invisible? Thank you. ANSWER: Hello! You need to watch! Everything is individual! It won’t be possible to make a seam at all! And you can make it minimally visible, observing all plastic principles, remove it and recreate it in a new way! get rid of the so-called “fishbone”!
breast bruise after mastectomy
QUESTION: Good day! My mother had breast cancer in her left breast and had a mastectomy. On the first day, or rather the evening after the anesthesia, she lost consciousness, fell on her chest, there was a bruise all over her chest, she complained that it felt like her chest was pinching; now they clean/wash the wound twice a day. what could be the consequences? ANSWER: Hello! None. Most likely, there was a collapsed state after the operation, this often happens, so we usually tell patients to lie down for the first 24 hours. Blood has accumulated in the area of the postoperative wound and is now a bruise. It's okay and will pass soon.
Mastectomy and fibroadenoma
QUESTION: Vitaly Aleksandrovich, in what cases with fibroadenoma do you recommend mastectomy. Thank you. ANSWER: Hello! Fibroadenoma is a benign disease and a mastectomy is never performed for fibroadenoma, so I do not recommend doing a mastectomy for fibroadenoma, only removing the tumor itself through a minimal incision and an invisible area, so that there is no visible scar in the future.
Mastectomy
QUESTION; Vitaly Alexandrovich, what kind of mastectomy should be performed for breast cancer? Thank you. You can read the ANSWER to your question at the link mastectomy
Mastectomy
QUESTION: Vitaly Alexandrovich, good evening! What is a Madden mastectomy? Thank you. ANSWER: Madden mastectomy is a gentle radical method that involves removing the mammary gland, but preserving the pectoralis minor and major muscles, which allows you to shorten the rehabilitation period and obtain the maximum possible cosmetic effect.
Reconstruction quota
QUESTION: Hello! In July 2022, we had a mastectomy of the right breast (stage 2A cancer). I live in a rural area and there is no oncologist. The attending physician is a surgeon. I wanted to sign up with my attending physician for a quota for breast reconstruction, but the doctor had not heard anything about it. He told me to find out everything about the quota myself and tell him what was needed for this. And he, in turn, will give all the directions that will be needed for the quota. Please explain what is needed to obtain a quota. Where to sign up, who to call? Thank you. ANSWER: Hello! You need to take a referral from an oncologist at your place of residence and go to your regional oncology clinic and get a quota there. Free assistance is provided as part of the compulsory medical insurance at the oncology center at the place of residence.
treatment after mastectomy according to Madenne
QUESTION: Hello Vitaly Alexandrovich! After a mastectomy according to Madenna for TNBC, what kind of chemotherapy is usually given, how much, h/w what is the time from course to course? They also prescribe rays after x/t. ANSWER: Hello! After a mastectomy for triple-negative cancer, any chemotherapy can be used, but in the regimen, taxanes are preferable, the chemotherapist knows this for sure! Taxanes can be prescribed once every 21 days or weekly! For this type of cancer, radiation therapy is also prescribed!
Collecting fluid after a mastectomy
QUESTION: Good afternoon! Today is 10 days after my mastectomy. I was discharged. I'm home. But it seems to me that fluid is collecting in me, a sort of sac appears. Go to the appointment only on the 9th. Is there any reason to panic? We live 250 km from the hospital. ANSWER: Hello! Normally, it should accumulate, if there are no signs of inflammation, and you feel good, then everything is fine and calm on the 9th, go for a dressing!
Mammography
QUESTION: Hello Vitaly Alexandrovich! Please tell me, is it necessary to do mammography (ultrasound) after a mastectomy on the axillary lymph nodes and is it possible to do mammography with an implant? ANSWER: Hello! Mammography for axillary nodes is not performed; only ultrasound of this area is performed. For implants, it is necessary to perform an MRI of the mammary glands, since this method is informative in this case, but mammography is not.
Airplane and mastectomy
QUESTION: Good evening! Is it possible to take a long flight on an airplane? ANSWER: Hello! Of course, you can take long flights after a mastectomy. This will not affect your illness in any way.
Mastectomy and sports
QUESTION: Doctor, hello! Can you please tell me when can I do TRX after a mastectomy? There was slight swelling of the arm on the side of the operation. Thank you. ANSWER: Hello! TRX training is not contraindicated for you in principle. It all depends on when the mastectomy was! How long ago and how much did your hand swell? If more than 3 months have passed, then you can gradually dosage it; if it starts to swell again, then you need to stop and take measures to prevent lymphedema!
RMJ
QUESTION: Good afternoon! On January 16, 2019, a sectoral resection was performed for a suspected fibroadenoma. A routine histological examination revealed infiltrative lobular breast cancer, grade 2 malignancy. In an immunohistochemical study, the reaction with antibodies to estrogen receptors is positive in 65% of tumor cell nuclei (intense staining) (7 points (TS) Allred score), the reaction with antibodies to progesterone receptors is positive in 80% of tumor cell nuclei (intense staining) (8 points (TS) Allred score), reaction with antibodies to the oncoprotein cerb - B2 0. Reaction with antibodies to Ki-67 is positive in 23% of tumor cell nuclei. On February 20, 2019, a Madden radical mastectomy was performed with plastic surgery of the axillary-subclavian region using a composite graft. Histological examination: At the site of the removed sector of the mammary gland there is lipogranuloma. Fmbrocystic disease of the breast: periductal fibrosis, ductal ectasia. No tumor cells were found. The nipple is of normal structure. No tumor cells were found in 17 axillary lymph nodes. No tumor cells were detected in 1 subclavian lymph node. The chemotherapy doctor prescribed treatment with Tamoxifen 20 mg per day for 7 years. Please decipher the histology after a mastectomy in simple language. Is it always the case that during a Madden mastectomy, so many lymph nodes are removed, because no cancer cells were found in them? And another question: Tamoxifen was prescribed, but I am allergic. The allergy manifests itself in the form of a skin rash. At the moment, it is most severe at the site of the postoperative suture. Everything is red and very itchy. Is it possible to replace the drug with something? 51 years old, menopause (about half a year ago I had spotting menstruation, the Chemotherapist claims that menopause is not yet stable). ANSWER: Hello! During mastectomy, all axillary lymph nodes are removed: they can be from 4-6 to 23 nodes, their number is different for everyone, red manifestations and itching in the area of the postoperative scar are not associated with allergic manifestations of tamoxifen, but with early changes in wound healing. You have early stage cancer and only Tamoxifen is indicated for you. Take this drug, and if after long-term use of 3-4 months this continues, then it must be changed to another drug.
Silicone patches
QUESTION: Good afternoon Vitaly Aleksandrovich, can you recommend which company is better to buy silicone plasters? Thank you in advance. ANSWER: Hello! Today there are already many manufacturers on the market, previously there were several, I recommend not getting hung up on any manufacturer, the main thing is that the bandage has a silicone base, and it doesn’t matter the brand! Find headbands that suit your price on the Internet!
Lump after mastectomy
QUESTION: Hello! A year ago I had breast removal surgery. I get examined once every three months. Now I found a very hard, uneven lump on my chest next to the seam. I often experience spasmodic pain in this area. The pressure has decreased, the pulse is 90-130 at rest. Could it just be a chest spasm? ANSWER: Hello! It could be anything, it is better to contact an oncologist at your place of residence and carry out a series of diagnostic procedures to exclude relapse of the disease. You are examined very often - once every three months!
One and a half years after mastectomy, pain on the operated side
QUESTION: Vitaly Alexandrovich, almost a year and a half has passed since the mastectomy (stage 2). Recovery was normal, without swelling. Exercises, massage, gentle regimen - everything is still being done. And recently, without any clear reasons, without increased stress or a cold, pain appeared again in the entire affected area. For two weeks now my arm and shoulder have been aching, even a small load is unpleasant, but there is no swelling. Can this phenomenon occur periodically? And is it worth increasing exercises and massage? ANSWER: Hello! This may happen, perhaps you have somehow stressed this area, but in this case I would contact an oncologist at your place of residence in order to carry out a set of minimal procedures to prevent tumor progression, since pain may be a manifestation of bone metastasis.
Breast prosthesis
QUESTION: Vitaly Alexandrovich, what is a breast prosthesis? ANSWER: Hello! A breast prosthesis is an artificial device that is inserted into underwear to replace a missing body part, in this case the breast.
Is mastectomy necessary and what is the prognosis?
QUESTION: Good afternoon. I am 43 years old and have been diagnosed with G3 invasive nonspecific carcinoma. IHC - expression of estrogen receptors is weak in 90% of nuclei, expression of progesterone receptors is pronounced and moderate in 80% of nuclei, ki 67 -30%. FISH - Her 2 negative 1+. CT scan showed no metastases. What will be the treatment and prognosis? Is a mastectomy necessary? ANSWER: Hello! The scope of the operation depends on the stage of the disease and the location of the tumor, usually your surgeon looks at it and determines the volume of the operation, this is very individual and breast preservation depends on many factors, it is often possible to perform organ-preserving surgery!
Lymphostasis
QUESTION: Good afternoon, doctor. In March 2022 I had a mastectomy with the removal of 7 lymph nodes. Recently, swelling of the arm and axillary area and severe pain, with anemia, appeared. What could it be? How to relieve unbearable pain. I wanted to make an appointment with you for a consultation in the near future, but I only have an appointment for May 15th. ANSWER: Hello! You need to be looked at to find out the possible cause. It is possible to consult with me by prior arrangement, by calling the phone number indicated on the website, or in any way convenient for you, and also sign up on the oncology center website.
complete breast removal, please tell me this is correct
QUESTION: Hello, Vitaly Alexandrovich! I am 49 years old, I was diagnosed with cancer of the right breast, here are the results of an immunohistochemical study: Strong estrogen expression>10% of tumor cells, strong progesterone expression, 10% of tumor cells, C-erb2 negative, ki67 - 10%. The doctor said complete breast removal, please tell me this is correct. ANSWER: Hello! Breast removal or preservation depends on many factors; in your case, you need to know the size of the tumor, its location and distance from the areola, breast size, one or more tumor nodes, and the type of cancer - lobular or ductal. Knowing these indicators, you can determine the indications for breast removal or conservation. If your surgeon says that only removal, then everything is not so simple for you. Simply being diagnosed with breast cancer is not an indication for breast removal.
Drainage after mastectomy
QUESTION: Hello! After a Madden mastectomy, my mother has a drainage installed, there is already 30 ml, it needs to be removed, and the doctors are on the weekend, since it’s the holidays, what do you recommend to do? Thank you. ANSWER: Hello! This is an important decision that your surgeon makes and it is better to discuss this with your attending physician; it is correct to leave the drain on the weekend, regardless of the volume in ml of the contents.
Severe redness after breast removal
QUESTION: A month has passed since the removal of the left breast, the first chemotherapy, there is severe redness throughout the entire area, it feels hot to the touch, but there is no temperature, what should I do? ANSWER: Hello! It is possible that lymph has accumulated there and needs to be evacuated from under the suture! Contact your treating surgeon!
drainage and blood with odor
QUESTION: Hello. I wanted to ask you, my mother was diagnosed with breast cancer, had surgery, there was a drainage, everything was fine and the fluid came out well, but a week later there was blood with a smell, what could it be. Thank you. ANSWER: Hello! Most likely, ichor with lymph accumulated there and became slightly inflamed and is now beginning to go away. In this case, it is better to contact the attending surgeon.
drainage after mastectomy is leaking
QUESTION: Hello! An operation was performed: radical resection of the mammary gland with regional lymphadenectomy. 6 days have passed, the stitch does not bother me, I am worried that I am leaking lymph from the hole where the drainage tube is sewn. Until yesterday everything was fine, 50 ml in the morning and 50 ml in the evening. Now little flows into the accordion storage tank, 20 ml in the morning, 30 ml in the evening. And it oozes out of the hole, I put a napkin under it, it’s damp. What to do in this situation? ANSWER: Hello! If the drainage does not work and leaks past, then you just need to remove it and that’s it! Contact your surgeon and he will remove your drainage!
the hand is limited in movement
QUESTION: Hello, a month has passed since my mastectomy. I'm doing exercises. But the arm is still limited in movement and hurts from the inside to the elbow. ANSWER: Hello! In general, this is normal, such phenomena can occur for up to 6 months. You need to go to a rehabilitation center and they will prescribe you adequate recovery.
1-50
51-78
Ask a Question
CATEGORIES
| Make an appointment [14] |
| Sign up for a consultation online [14] |
| Questions from the live broadcast on Instagram “Medical Reporter” [5] |
| Quota for breast reconstruction [25] Reconstruction of the mammary gland (breast) after mastectomy according to quota |
| Reviews about the work [8] |
| Breast cancer [1731] All about breast cancer: diagnosis, treatment, breast restoration and reconstruction. |
| Diagnosis of breast cancer [140] |
| Breast diseases [184] |
| Mammography [56] |
| Ultrasound of the mammary glands (breasts) [185] |
| Computed tomography and MRI [51] |
| Scintigraphy (osteoscintigraphy) [40] |
| Examination in remission [11] |
| Cytological examination of breast cancer [33] |
| Biopsy and histological examination of breast cancer [60] |
| Immunohistochemical study of breast cancer [250] Immunohistochemical study |
| Her2neu [60] |
| her 2 [16] |
| ER and PR [15] |
| ki67 [71] |
| Surgical treatment of breast cancer [60] |
| Mastectomy [78] |
| Organ-preserving operations [35] |
| Preventive mastectomy [10] Preventive mastectomy |
| Breast reconstruction according to quota [46] What is included in breast reconstruction according to quota, breast correction after reconstruction, lipofilling |
| Breast reconstruction consultation [32] |
| Breast reconstruction (breast surgery) [181] Breast reconstruction |
| Breast reconstruction [112] |
| Reconstruction of the nipple and areola [10] |
| Breast lipofilling [25] |
| Internship of Skvortsova V.A. in the USA, MD Anderson Cancer Center [2] |
| Mammoplasty (breast augmentation) [1] |
| Breast removal [4] |
| Chemotherapy for breast cancer [213] |
| Side effects of chemotherapy [29] |
| Taxanes (paclitaxel, docetaxel) [21] Taxanes (paclitaxel, docetaxel) |
| Paclitaxel [7] |
| Zoledronic acid [7] |
| Targeted therapy [58] |
| Trastuzumab (Herceptin, Herticad) [16] |
| Antihormonal endocrine therapy [240] Treatment of hormone-dependent breast cancer |
| Tamoxifen [198] Tamoxifen |
| Radiation therapy [121] Radiation therapy |
| IORT [11] Intraoperative radiotherapy |
| Cancer in situ [27] |
| Treatment of breast cancer [183] |
| Luminal A breast cancer [69] |
| Luminal In breast cancer [56] |
| Luminal In her positive breast cancer [37] |
| Her2neu positive breast cancer [20] |
| Triple negative breast cancer [98] |
| Breast cancer prognosis [24] |
| Treatment of breast cancer [45] |
| Treatment of stage 1 breast cancer [38] |
| Treatment of stage 2 breast cancer [37] |
| Treatment of stage 3 breast cancer [45] |
| Treatment of stage 4 breast cancer [53] |
| Breast cancer recurrence [25] |
| Monitoring the effectiveness of breast cancer treatment [13] |
| Medicines [42] |
| Vitamins [8] |
| Lymphorrhea, lymphostasis, lymphedema [77] Lymphostasis and lymphorrhea |
| Immunomodulators for cancer [4] |
| Keloid scar [1] Keloid scar |
| Ovariectomy for breast cancer [20] Ovariectomy |
| BRCA1, BRCA2 [7] |
| Tumor markers [42] |
| Mastopathy [5] |
| Fibroadenoma [46] Fibroadenoma |
| Breast cyst [21] |
| Injuries to the mammary gland (chest) [6] |
| Follow-up after breast cancer treatment [24] |
| Life after breast cancer treatment [143] |
| Myths and truths about breast cancer [32] |
| After breast cancer surgery [32] |
| Rehabilitation after breast cancer [14] |
| Miscellaneous [107] |
| Pregnancy and childbirth after breast cancer [2] |