- home
- Breast surgery
- Breast reconstruction after mastectomy using lipofilling
Breast cancer ranks first among all malignant diseases in women. According to statistics, the incidence of malignant neoplasms of the mammary gland in the Russian population has more than doubled over the past 15 years. Unfortunately, these patients require complete or partial resection (removal) of the gland. And, of course, after such an operation, in addition to the absence of the gland, numerous rough scars remain, which significantly complicate its aesthetic restoration in the future. This becomes a great psychological trauma for a woman and affects her quality of life. However, this does not mean that the breast is lost forever.
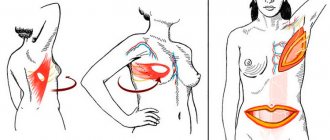
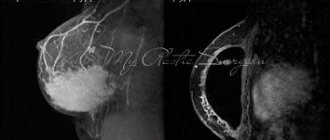
In the photo: the patient underwent lipofilling and breast prosthetics. The next stage of reconstruction is planned to form the areola (followed by tattooing, imitating the natural color of the nipple). According to David Grishkyan, breast tissue after resection often behaves unpredictably, so consistent step-by-step restoration allows for more precise manipulation with a predictable result.
Indications for breast reconstruction with lipofilling
- The patient requires breast reconstruction after a mastectomy, when there is a problem of lack of tissue for prosthetics.
- Failure or inability of the patient to undergo complex traumatic operations associated with the formation of new scars in the donor area.
- The patient’s desire to avoid the use of implants and other foreign objects during breast reconstruction.
- The desire to heal and rejuvenate the skin, create a reservoir and stretch internal tissues for subsequent prosthetics.
- Carry out reconstruction using the most gentle method possible, with comfortable rehabilitation and minimal risk of complications.
Preparing for breast reconstruction surgery
Before undergoing breast reconstruction surgery, an examination and consultation with an oncologist or mammologist is mandatory. Blood and urine tests are required, as well as an assessment of the patient’s general health by specialized specialists.
As with any surgical procedure, it is necessary to avoid smoking and drinking alcohol. Taking any medications must be agreed with your doctor. It is advisable to monitor your weight - obese patients usually tolerate anesthesia less well. You should discuss physical activity with your doctor. Exercise will increase the elasticity of the tissues that will be needed for transplantation.
The essence of the method of breast reconstruction using lipofilling
Our clinic has developed a technique that allows women to recreate lost breasts. The difficulty of reconstructive surgery often lies in the fact that the tissues lose their elasticity, and rough scars exist not only on the outside, but also on the inside. Therefore, the first stage of the operation is tissue preparation, which we carry out using the American BRAVA system. Thanks to the BRAVA system, we are able to stretch and prepare the skin, as well as gain space for the subsequent introduction of a fat graft into the breast (lipofilling) and improve the survival of fat cells in the postoperative period.
The next step is to restore the breasts with our own fat cells, which we take from the patient’s donor areas, thereby creating a fat layer that will later allow us to get natural breasts. In addition, adipose tissue has other advantages: it secretes growth factor, which has a beneficial therapeutic effect on scars in the transplantation area.
The last stage is the formation of the nipple and areola. In many cases, it is necessary to perform surgery on both mammary glands at once in order to achieve symmetry. To do this, if necessary, a second breast lift, reduction or prosthetics is performed. Our method allows you to carefully and correctly restore the mammary glands, without leaving additional scars or scars on the body. Usually, operated patients (even those who had some doubts before the operation) would never take a step back - their moral and aesthetic satisfaction is truly great.
- In preparation for surgery, the patient wears special vacuum external expanders, often at night.
- To stretch the skin and create a reservoir, as well as improve tissue health, the first stage of lipofilling is performed. The fat tissue obtained during liposuction is prepared and injected into the breast area.
- To form the required shape and volume, an additional fat autograft is introduced into the already prepared tissues. At the patient's request, breast prosthetics are performed. Often a simultaneous operation is required on a healthy breast to create symmetry.
- A vacuum system of external expanders is used to ensure engraftment of the injected fat cells.
Organ-preserving interventions
During organ-conserving surgery, the tumor and a portion of surrounding healthy tissue are removed. This operation is called a lumpectomy . Sometimes you can hear other names: quadrantectomy, partial mastectomy, sectoral resection - depending on the volume and characteristics of the intervention.
The removed tissue is sent to a laboratory to be examined under a microscope. It is important to study the resection margin - the border of the removed tissue. There should be no tumor cells in it: in such cases they speak of a negative resection margin , which means that the tumor has been completely removed. If the resection margin is positive, this indicates that there are cancer cells in it, perhaps they remain in the woman’s body. The doctor may prescribe repeated surgical treatment.
How is breast reconstruction performed using lipofilling?
The plastic surgeon determines the areas suitable for fat tissue harvesting and the approximate number of operations that will be needed to achieve the most aesthetic result. The external vacuum expander system consists of special bra cups in which a vacuum pump creates negative pressure. For three to four weeks before surgery, the patient uses the system daily for 10-12 hours. The operation is performed under general anesthesia; preoperative preparation, which includes all the necessary tests, is mandatory. The collection of adipose tissue for lipofilling is carried out using special thin cannulas through small punctures; traces of this procedure are leveled over time and will not be noticeable. By forming microtunnels, the surgeon injects fat cells in small doses for their best engraftment. Using back-and-forth movements, the surgeon fills the deep layers of tissue with the patient’s own fat, then the superficial ones. After the operation, the patient is put on a system of vacuum expanders - it mobilizes the transplanted fat cells, resulting in the formation of new blood vessels and protects the breasts from external factors and injuries. The reconstruction takes place in several stages with the necessary time intervals for restoration. The transplanted fat cells make the tissue healthier and more elastic; if the patient wishes, the final stage of breast reconstruction can be the installation of an implant to give the breast volume and a more curvaceous shape.
One on one with the diagnosis
Irina (name changed) has a different cancer. Stage 2 thyroid cancer. The nodes, which she had been monitoring for half her life, turned out to be malignant after removal. In general, this type of cancer is not very aggressive and rarely metastasizes. But Irina found out about this from the Internet. The surgeon, handing her the histology results, muttered something about cancer and left.
“Then, at the clinic at my place of residence, where I was supposed to undergo regular examinations, the oncologist, from whom I expected at least some kind of explanation, did not explain anything to me. He didn't talk to me at all. It seems he didn't even look. I took a piece of paper and entered something into the computer. I wrote out directions for an ultrasound. I went to many doctors, I visited regional oncologists, I visited the oncology clinic, and I visited private clinics. Doctors don't explain anything at all. At best, they answer questions, but I didn’t always know what exactly I should have asked,” says Irina .
Reference: Clinical depression accompanies 8 out of 10 cancer patients. It often develops against a backdrop of uncertainty. A person hears his diagnosis and is left alone with it.
The doctor does not explain what is happening in the body, what you can expect, how to live with it. For some reason, doctors act as if they are embarrassed to tell a patient a diagnosis, but at the same time for them it is a common thing and, of course, they do not care. It looks like this: “Here you can wash your hands, there’s delicious borscht in the cafeteria today, and you also have cancer.”
Then there will be tears, trips to doctors, complex and difficult treatment. When the fear of the pain of death recedes a little, the moment of getting to know your new body comes. This is especially true for female cancers: breast, body and cervix.
Exposition of the exhibition “SPORKING”. Photo by Andrey Titov
Nipple tattoo
To restore the shape and volume of the breast, there are many methods of reconstructive surgery, and to restore the aesthetic side - tattooing, as a way to restore the nipple-areolar complex. A specialist uses pigments to graphically recreate their relief and structural features. Tattooing is performed on both breasts to achieve a uniform color. As a rule, at least three colors of implanted pigments are used simultaneously to work on the nipple-areolar complex. The pigments for dermatopigmentation used in the clinic are a certified, modern complex product, do not cause irritant reactions, do not come into contact with organic tissue and are not excreted through the lymphatic system. New generation pigments are resistant to various factors (such as ultraviolet radiation). Stable fixation in the skin is guaranteed by the optimal molecular size (about 6 microns). Modern anesthetics make the procedure painless.
Before mastectomy
Before the operation, the woman receives specific instructions that describe restrictions and other things she needs to know. The patient should tell her doctor about any medications, vitamins, or supplements she is taking. Taking certain substances may negatively affect the course of surgery. For a week or more before surgery, you should avoid taking medications that may increase the risk of excessive bleeding. These include aspirin, ibuprofen and other pain relievers and blood thinners (anticoagulants).
Immediately before the operation, 8-10 hours, you should stop eating and drinking. It is also worth preparing in advance for your stay in the hospital. Find out how long you plan to stay there. Pack a bag with a toothbrush, robe, and slippers to make your hospital stay more comfortable. Also, prepare something that will help you pass the time, such as a book.
A mastectomy without reconstruction usually takes one to three hours. This usually requires one extra day in the hospital, although more and more women are choosing to go home on the day of surgery.
If you have surgery to remove both breasts (double mastectomy) or breast reconstruction after a mastectomy, the surgery may take longer and your hospital stay after surgery may increase to several days.
To perform a sentinel node biopsy, a radioactive substance or blue dye is injected near the tumor before surgery and deposited in the sentinel lymph node. This will allow the surgeon to identify and remove the affected lymph nodes during surgery.
Postoperative period
Breast amputation, regardless of typology, is a complex invasive intervention. You will have to spend about a week in the hospital, then the patient will have a recovery period lasting up to 3 months. After a mastectomy without plastic surgery, the operated patient will stay in the clinic for 4 days. In the first month, visits to the inpatient department are required for regular dressing changes and examinations.
When the anesthesia wears off, severe pain begins, lasting about 4-6 days. During this period, painkillers are usually prescribed. The patient must wear a drainage system for a week. Since you are sometimes discharged home with tubes attached to your body, the nurse will tell you in detail how to avoid damaging the device and dressing. You can get up and move around a little the day after surgery. In the future, wearing a corset and compression garments is recommended. Under no circumstances should you lift heavy objects or make sudden movements.
Disability after invasion is due if the diagnosis that led to the mastectomy is breast cancer. The intervention is followed by mandatory chemotherapy and radiation therapy, the consequences of which deprive the woman of her ability to work. Usually the patient is assigned a second disability group with re-examination after a year.
Consequences
The postoperative period does not always go smoothly. Complications may appear immediately or later, and there is also a risk of relapse. Life after a mastectomy is often overshadowed by psychological worries, doubts about one’s own attractiveness, and the expectation of potential disability. If depression occurs, you will need the help of a psychotherapist.
Complications of mastectomy more often occur in elderly, chemotherapy-weakened, and obese patients. Within 3–4 days, bleeding and lymphorrhea are observed, sutures come apart, necrotic tissue damage, and purulent inflammation are observed. Later, phantom pain appears, disruption of venous and lymph flow, swelling, loss of sensitivity, keloid scars form, and limb movements are distorted.
Relapses of cancer occur six months to a year after mastectomy. Most often they occur if the operation was performed in the late stages of cancer due to incorrect diagnosis, refusal of radiation therapy, or the presence of active metastasis. After 5 years, cancer can be considered defeated.
It is important to follow the doctor’s recommendations even after the postoperative period. Contraindications after invasive mastectomy:
- No sex for three months.
- Do not take hot baths.
- Avoid saunas and steam baths.
- You can't get pregnant for three years.
- Holidays at sea for 3 years are not advisable.
- Do not lift weights exceeding 1–3 kg.
- Smoking and drinking alcohol are contraindicated.
- Sharp bends and raising of arms are excluded.
A salt-free diet is recommended, excluding fatty and smoked foods. The support of relatives is crucial in the rapid recovery of the operated patient.