Serous fluid is clear moisture that is secreted by the membranes of the body cavity. Its secretion is a natural consequence of the functioning of the body. The occurrence of serous discharge is associated with the filtration of the contents of blood vessels, which is why it contains protein along with leukocytes, mesothelial cells and some other elements. Against the background of disruptions in blood and lymphatic circulation, excessive amounts of moisture may accumulate in the body, which is accompanied by copious discharge.
What are the signs of discharge after surgery?
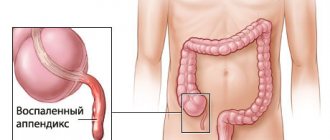
An enlarged area of surgical intervention is considered the main symptom of an emerging disorder. This symptom often occurs after liposuction, as well as against the background of plastic surgery to install implants. Following the removal of a large amount of fat from the internal cavity, serous moisture begins to accumulate in the resulting voids. The introduction of implants may additionally be accompanied by a rejection process, due to which fluid will accumulate between the soft tissues and the foreign element.
Serous discharge is determined by the swelling of the surgical area. Palpation of this area may cause an unpleasant sensation in the patient. Often mild pain accompanies the patient even without pressing on the area of swelling; it can intensify with slight physical activity. As seromas (the so-called accumulation of serous fluid) progress to severe stages, colic may become more intense.
One of the main signs of the appearance of seroma is considered to be hyperemia of the skin in the area of \u200b\u200bthe operation. With moderate serous discharge, this symptom often does not appear. It can occur when an excessive amount of excess moisture accumulates, which will indicate the need for its mandatory removal from the body.
Serous discharge from the suture is a fairly rare occurrence, indicating a severe form of the disorder. The initiation of the treatment process often leads to the formation of a fistula tract, through which excess moisture begins to ooze out.
Next, we will find out what are the causes of serous-purulent discharge from a wound during surgical intervention.
How does the process of wound suppuration develop?
Typically, suppuration begins when a clean wound becomes infected, swelling around the wound develops, tissue necrosis and purulent discharge appear. If redness begins around the wound, which is accompanied by a tugging pain that gets worse at night, then this means that you are dealing with the first symptom of wound suppuration, and urgent measures need to be taken.
When examining the wound, dead tissue and pus are visible. The situation is dangerous because the decay products are absorbed by the body, and this leads to increasing intoxication of the body. As a result, the following symptoms appear:
- significant increase in temperature;
- chills;
- headache;
- weakness;
- nausea.
Causes of discharge from a wound
So, basically, the accumulation of serous fluid is directly related to the extensive wound surface, which is accompanied by detachment of the subcutaneous tissue. Surgical intervention must be accompanied by delicate handling of the internal cavity. It is unacceptable to interact roughly with tissues and use low-quality tools. The cut must be made quickly and carefully in one motion. The use of blunt instruments along with the unsteady hand of the surgeon turns the surgical area into a kind of mess of damaged tissue that can bleed and be destroyed, which will lead to the formation of a large amount of serous discharge.
An extensive wound surface may simultaneously be accompanied by destruction of the lymph nodes. Numerous injuries to the lymph nodes lead to increased secretion of serous secretions. Unlike blood vessels, they do not have such a rapid healing ability and therefore become scarred within one day after surgery.
The reason for the formation of copious serous discharge may be excessive bleeding of the internal tissue. Through small capillaries, blood can enter the operated area, forming hemorrhages. After some time, they usually resolve and form serous fluid.
Another example of the occurrence of serous-purulent discharge is the development of a postoperative hematoma in a patient. Against this background, the source of filling the cavity with liquid is not capillaries, but large vessels, whose damage often leads to bruising. In this case, serous discharge appears only on the fifth to seventh day after surgery. Resorption of the hematoma may be accompanied by the formation of fluid. It is important to monitor the patient closely during the first few days after surgery to monitor for small bleeding that may be difficult to detect during surgery.
In what other cases does serous discharge from a wound occur after surgery?
After plastic surgery, implant rejection cannot be ruled out. Some patients are overly sensitive to foreign elements. Taking this into account, their manufacturers strive to use the highest quality biomaterials, which significantly reduce the risk of rejection. But, nevertheless, it is impossible to predict with complete certainty the body’s reaction to implants. Therefore, due to the rejection of a foreign element, serous discharge may also begin to accumulate.
Next, we’ll talk about how serous fluid accumulates in the uterus and find out what the main causes of this pathological process are.
Excess exudate
If there are no crusts or necrosis in the wound, then the technique of local negative pressure can be used for active outflow of exudate. For these purposes, the PICO wound treatment device is used, which creates a constant outflow of purulent exudate from the wound, which is accompanied by a decrease in tissue swelling, a decrease in the number of bacteria in the wound, as a result, the inflammatory reaction subsides, and the growth of new tissues begins, the vessels that fill the wound begin the epithelium grows, the edges of the wound gradually come closer together and the wound heals. When using this device, there is no need to carry out dressings daily. It is enough to change the dressings on average once every three days.
For passive drainage of exudate from the wound, absorbent dressings of your choice are used:
- Carbonet. This multi-layer dressing perfectly absorbs viscous purulent exudate, and, thanks to a layer of activated carbon, absorbs the odor that often accompanies purulent wounds. Since Carbonet does not contain antimicrobial components, dressings on purulent wounds must be changed daily.
- NEOFIX polyurethane sponge dressings with silver - NEOFIX FibroSorb AG and NEOFIX FibroSorb AG Sacrum. Silver in dressings provides antimicrobial effect.
Sponge dressings absorb liquid exudate and retain it in their structure even under pressure, for example, under compression bandages or underwear (stockings, stockings, tights), which are one of the main attributes of the treatment of trophic venous ulcers. NEOFIX FibroSorb AG sponge dressing
without adhesive edge is indicated for wounds where the skin around which is damaged.
Such a bandage requires additional fixation with a bandage or adhesive roll bandages NEOFIX ROLL, or OpSite Flexifix, always only around the perimeter, without covering its central part with adhesive patches. This is necessary to prevent maceration of the skin and wound. NEOFIX FibroSorb AG Sacrum bandage
with a sticky edge, specially shaped for fixation in the sacrum area, while the skin around the wound should be dry and healthy, without any disturbances. The bandage protects the wound from the ingress of urine, feces, as well as from the penetration of external liquids during hygiene procedures.
When using NEOFIX FibroSorb AG and NEOFIX FibroSorb AG Sacrum dressings for wound treatment, there is no need to change dressings daily. It is recommended to change the dressing once every 2-3 days, depending on the degree of filling of the dressing with exudate.
How does serous-mucous discharge occur in the uterus?
A serosometer is a collection of serous fluid in the uterus.
Many people wonder what color is serous discharge from the uterus? This substance is transparent and has a special composition similar to blood serum.
Between the muscular uterine tissue and the endometrium there is a serous membrane (it is a film of connective tissue), which is penetrated by many capillaries. Transparent yellow blood plasma can leak through the walls of these tiny vessels. This, in fact, is that same serous fluid. If a woman has scars on the cervix or any other defects that prevent fluid from being removed from the cavity, it accumulates and stagnates.
Obstacles to the release of accumulated serous discharge from the uterus may appear due to previously suffered gynecological diseases, various operations on the uterus, malignant tumors, and so on. The consequences of such processes may be atrophy of the mucosa along with narrowing or fusion of the tissues of the cervical canal. In more complex cases, fluid also accumulates in the cervical canal, and then the so-called serozocervix develops.
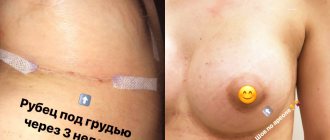
Seroma after cesarean section
Mothers in labor encounter this pathology quite often. This is explained by the depletion of the body’s internal resources during pregnancy. It becomes incapable of rapid tissue regeneration. Seroma in women in labor often leads to the development of complications such as ligature fistula and suppuration of the suture. In some cases, the inflammatory process goes inward and affects the pelvic organs.
Initially, seroma in women who have undergone a cesarean section appears in the form of a small ball with exudate in the suture area. It does not cause concern and can resolve without any treatment. But if the compaction area increases in size, then immediate treatment is required.
Why does serous fluid accumulate in the uterus?
Many women encounter diseases of the genital organs during childbirth and during cleansing, but not everyone experiences serous fluid in the uterus. This is not a disease characteristic only of the postmenopausal period, and can also appear in young women.
For example, exposure to nicotine or alcohol on the female body, along with hormonal disorders as a result of long-term use of contraceptive drugs during premenopause, can contribute to the occurrence of serous stagnation.
The suture gets wet after surgery, how to treat it?
Doctors recommend proper care of the postoperative suture. Many people ignore advice on purchasing compression garments, bras and panties. This should not be done, because underwear allows you not only to reduce the belly after a caesarean section, but also prevents the development of seroma. Pressure is necessary on the suture area to prevent fluid accumulation.
The suture gets wet after surgery, how to treat it?
- It is often recommended to ventilate the seam after a caesarean section. You should not cover it with a large number of bandages, much less seal it with adhesive tape. Such manipulations provoke a sauna effect, as a result of which the seam sweats, possibly causing a secondary infection.
- Therefore, in between wearing compression garments, it is recommended to walk without clothes, or at least with a T-shirt raised, so that the seam dries out and is ventilated. In addition, it is recommended to wash the wound with laundry soap twice a day. This product dries the skin well and disinfects it. It is recommended to carry out antiseptic treatment using hydrogen peroxide or regular alcohol.
- Some experts recommend Solcoseryl or Bepanten ointment. But Bepanten is oil-based, so it can also provoke an infection, this is important if it is already very hot outside. You should definitely follow the doctor’s recommendations and not lift anything heavy.
- After all, this can also contribute to the seam coming apart and getting wet. Usually after 2-3 weeks the suture is completely tightened and heals without traces. The wound stops getting wet. Often one or two holes may be found on the surface of the seam. These are peculiar fistulas through which excess fluid comes out. There is nothing wrong with their formation, however, keloid scars and the proliferation of fibrous tissue may appear. This may subsequently cause seals to form.
Abdominoplasty
Serous discharge from the uterus in postmenopause
At the beginning of postmenopause, hormonal changes in the female body are already completely completed. A decrease in the level of sex hormones affects the condition of the uterine mucosa. Regular renewal of the endometrium is completed. The cleansing of the uterine cavity from physiological fluids also stops. Stagnant processes cause unpleasant symptoms, for example, serous discharge from the uterus may be observed. In each case where there are deviations, the choice of treatment method is approached individually.
Factors that increase the risk of discharge
These factors include the following:
- Decreased physical activity, which causes disruption of the blood supply to organs. Age-related changes lead to thinning of blood vessels, and in addition to the appearance of areas of expansion and contraction. Blood flow can slow down, and pressure on the vascular walls increases, and thus their permeability increases.
- Poor metabolism along with poor nutrition. Abuse of fatty foods may cause cholesterol deposits in blood vessels. The human body spends a lot of energy processing fatty foods, so the load on blood vessels increases significantly.
- Presence of vaginal dryness. This is the most characteristic sign of menopause. Thinning of the vaginal mucosa leads to the appearance of microcracks, which is why certain inflammatory diseases easily arise. In addition, the composition of the microflora is disrupted. Against the background of all this, the infection is able to easily penetrate the uterus, which will lead to changes in the tissue structure of the cervix and uterine cavity. The douching procedure only worsens the situation and increases dryness.
- Treatment with hormonal medications to relieve the symptoms of menopause.
- The appearance of polyps, fibroids, cysts and endometriosis, which disrupt the structure of the surface of the uterus.
Indirect reasons
In addition to these, there are other factors that can indirectly affect the appearance of serous discharge during menopause:
- The presence of benign or malignant neoplasms in the uterus, ovaries or fallopian tubes.
- The presence of a viral or bacterial infection of the genital tract.
- Untreated endometriosis.
- Carrying out unsuccessful abortions or operations that left large scars on the uterine mucosa.
- Passion for bad habits. The fact is that smoking and alcohol can cause swelling, and in addition, reduce the tone of blood vessels.
- Deficiency of vitamins and minerals. It is worth noting that against the background of impaired salt metabolism, the risk of edema increases.
So, what is serous discharge?
Symptoms
At the initial stage of the appearance of discharge, when not much fluid has accumulated in the uterus, a woman may not even notice this disorder, since the body itself will not clearly signal this. Women's genital tracts can normally contain up to one and a half liters of fluid. But when serous discharge begins to accumulate, viruses and bacteria develop in it. The fluid presses on the abdominal wall, as well as on the urinary canals, and against the background of all this, the following unpleasant symptoms appear:
- There is a frequent urge to urinate.
- Bladder capacity decreases.
- Painful urination occurs.
- There is pain in the lower abdomen and lumbar region.
- Abdominal girth increases.
- There is copious liquid discharge.
With a serozometer, the uterus in women begins to expand and, as it were, pushes the abdominal wall forward, in fact, this is what causes the increase in the volume of the abdomen. Liquid discharge against this background may have a yellowish or gray color. As a rule, they have no odor, but in the event of a bacterial infection, it can become unpleasant.
If an infection is added to the serous discharge, the woman may develop a high temperature due to the toxic waste of microorganisms absorbed into the blood with fluid from the uterus. Advanced cases lead to pathologies of the uterus and fallopian tubes.
It is important to remember these symptoms and consult a doctor in time, because serous discharge during menopause in advanced cases can end very badly, namely uterine rupture. This usually does not happen very often, since the organ has very strong muscles, but, nevertheless, its volume is also limited.
We looked at what serous discharge looks like.
The infection must be suppressed
To combat infection in a wound, it is best to use ACTICOAT and ACTICOAT7 dressings. These are mesh absorbent dressings that allow unimpeded drainage of exudate from the wound and fight infection. These dressings contain silver. The antibacterial activity of silver has been known for many years and its effectiveness is beyond doubt. The activity of silver is not affected by the presence of blood and pus in the wound. All causative agents of wound infections, including antibiotic-resistant bacteria, are not resistant to silver. Silver has a universal, wide spectrum of action, including against mixed microflora containing various bacteria, fungi, and yeast. The use of dressings with silver leads to rapid suppression of the inflammatory reaction in the wound, and at the same time the amount of discharged exudate decreases.
It is important that the silver in ACTICOAT and ACTICOAT7 dressings begins to be released immediately as soon as the dressing is applied to the wound, and quickly, within the first 30 minutes, the necessary concentration of silver is achieved in the wound to fight infection, and this concentration of silver is maintained at a constant level throughout long-term - up to 3 days when using ACTICOAT dressings and up to 7 days when using ACTICOAT7 dressings, thereby ensuring long-term antibacterial activity of the dressings, so the ACTICOAT dressing can be on the wound for up to 3 days, and the ACTICOAT7 dressing up to 7 days, with external absorbent dressings (gauze or Allevyn sponge) must be changed daily.
Use an acticoate dressing to effectively fight infection.
Carrying out treatment
It is worth immediately warning all women against such useless methods of therapy as the use of diuretics or herbs and any traditional treatment recipes, since none of this will definitely help remove fluid from the uterus.
Serous discharge should be treated by a surgeon. As part of the treatment, the cervical canal is expanded, and then the contents of the uterus are drained, but the therapy process does not end there. After removing the fluid, samples of the mucous membrane must be taken for histological examination. This will make it possible to accurately determine the reasons for the deviation. Such diagnostics help to detect inflammatory processes and neoplasms caused by infection.
Once the cause of fluid accumulation in the uterus is identified through histological analysis, the woman will need to undergo postoperative treatment. If the factor causing the serous fluid is malignant or benign tumors, they must be removed, and if the problem is an infection, then it must be treated with antibiotics or antiviral drugs.
What serous discharge from the uterus looks like is now known. During menopause, they often appear in women. This pathological condition can signal serious health problems, so you should go to the doctor with such symptoms. Conventional drainage of the uterus will only temporarily remove the accumulation of serous fluid, and in order to prevent the next occurrence of the pathology, the cause will need to be eliminated.
Suture after cesarean section, fluid oozing: reasons
But not everything depends on the surgeons; the patient’s health status matters. That is why, before surgery, a series of studies and tests are prescribed. The likelihood of seroma occurring increases in such cases.
Suture after cesarean section, fluid oozing, reasons:
- Diabetes
- High pressure
- Excess weight
- Poor blood clotting
- The presence of a large amount of fat and subcutaneous tissue
In approximately 70% of cases, complications occur in overweight people. If the amount and thickness of adipose tissue is more than 5 cm, most likely, seroma formation will occur in the incision area and a large amount of fluid will be released. That is why, in some cases, patients are advised to lose weight before undergoing surgery, prescribed a diet, or undergo liposuction in emergency cases. If a person has high blood pressure, taking blood pressure-lowering medications is also recommended.