From the medical history
M.V., 29 years old, first pregnancy, had experience of unsuccessful lactogenesis with her first child.
Her obstetric, medical, family and social histories were ordinary. She did not take medications regularly and did not use tobacco, drugs or alcohol. She noted that her breasts were small and widely spaced, without much change during pregnancy. Her mother breastfed 4 children without any difficulty. In an uncomplicated labor, she gave birth to a boy and began nursing him within the first hour of birth, and nursed with a good latch every 2 to 4 hours during her hospital stay. M.V. and her newborn were discharged home on the second day. M.V. She sought help from a lactation consultant when her milk did not come in on the 5th day after giving birth. Her baby wet too few diapers and was excessively fussy. The pediatrician noted significant weight loss (13% less than birth weight). M.V. They prescribed supplementary feeding every 2-3 hours. At 4 weeks postpartum, all her tests, including complete blood count, prolactin, testosterone and thyroid-stimulating hormone levels were normal. The course of metoclopramide (an analogue of domperidone - approx.), which was prescribed by the doctor, did not lead to an increase in the amount of milk. On the recommendation of one of the lactation consultants, she started taking fenugreek regularly and her milk began to increase slightly. Although she felt very tired and regarded the situation as a failure of breastfeeding, M.V. steadfastly continued to breastfeed.
M.V. I fed with supplementary feeding for 7 months. During this time, she was unable to express more than a few milliliters.
2 years later she became pregnant again. There were no breast changes during pregnancy. At 38 weeks, she gave birth to a boy through natural spontaneous labor. Her breasts, colostrum, and newborn latch were normal. She managed to start breastfeeding, but had to use supplementary feeding again after being discharged from the hospital. At 3 weeks postpartum, she was able to express 5 ml from each breast in 15 minutes, and a lactation consultant was called and diagnosed breast hypoplasia.
Breast-feeding
WHO recommendations
All professional organizations now recommend that women breastfeed exclusively for 6 months. [7–13] The American College of Nurse-Midwives believes that breastfeeding is based on both instinctive and learned behavior patterns, and a woman's choice to breastfeed is influenced by health care providers [9]. The American Academy of Pediatrics recommends that women breastfeed for at least 12 months and notes that contraindications to breastfeeding are rare [7]. The World Health Organization opposes the routine use of infant formula, including because formula lacks the antibodies found in milk and because formula is diluted to increase the risk of malnutrition due to lack of maternal education and the high cost of the product. and due to the risks of using unsafe water. [10] WHO also talks about fluorosis and staining of permanent teeth due to excessive fluoride content in infant formula, which is diluted with fluoridated water [12]
While it is important to encourage breastfeeding and support mothers in their efforts to breastfeed, it is also important to correctly and promptly identify women who are unable to produce enough milk to exclusively breastfeed their newborns. (you can supplement feeding not only with formula, but also with donor milk - approx.)
Anatomy and physiology of lactogenesis
(lactogenesis - the development of the ability of the mammary glands to secrete and secrete milk - approx.)
For successful breastfeeding, the breasts must contain sufficient glandular tissue, as well as intact hormonal and neuroendocrine pathways. This does not mean that a woman must have large breasts, but a sufficient amount of glandular tissue is necessary. Research shows that there is a weak correlation between a woman's breast size and her ability to produce milk [6, 14, 15].
After intensive development during puberty, the mammary glands typically develop fully during pregnancy, including intensive penetration into the epithelium and further differentiation. [16, 17]
The increase in estrogen levels that occurs during puberty stimulates the proliferation of glandular tissue, lengthening, branching and increasing the number of ducts within the fatty tissue of the breast. Rising levels of progesterone and prolactin during pregnancy stimulate further growth of glandular tissue through cell proliferation by division, further development and branching of the network of ducts and the development of milk-filled alveoli. [18]
These changes observed during pregnancy, which ultimately lead to the ability of the breast to produce milk, are called lactogenesis I. [17]
In the first four days after birth, progesterone levels decrease significantly, which leads to a new transformation of mammary gland tissue and the beginning of abundant milk production. This stage is called lactogenesis II. [17, 18] Lactation also requires the hormone prolactin in sufficient quantities and a sharp drop in progesterone levels, which occurs after the placenta is delivered. [18] (More details about the mechanism and stages of lactogenesis can be read here - approx.)
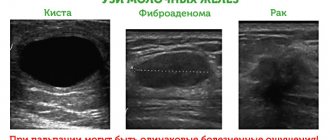
Women with breast hypoplasia have no or insufficient glandular tissue. Ultrasound can be used to study the anatomy of the nursing breast. [9, 19] In one study, researchers noted that 80% of lactating women who had a difference in the amount of milk expressed between the left and right breasts of more than 200 g had more glandular tissue in the more productive breast [19], which supports the thesis that the more glandular tissue there is in the breast, the more milk it produces, if all other factors are normal. [20] (Russian experts note that the use of ultrasound to diagnose hypoplasia is not always indicative, since this method shows only the presence or absence of glandular tissue, but not the degree of its development, and is only advisable during lactation - approx.)
However, several questions regarding breast glandular tissue remain unanswered. It is unknown whether there is a minimum required level of glandular tissue for successful exclusive breastfeeding. It is also unknown whether the location of the glandular tissue inside the breast affects the level of lactation. The anatomy of women with breast hypoplasia has not been studied immediately after childbirth or during breastfeeding.
Lactogenesis disorders II
There are many reasons why women do not have enough milk for their newborn babies. "Low milk" is a general term that describes a newborn's insufficient milk supply, regardless of the cause. Lactogenesis disorder II - This term describes a situation where a woman is unable to produce enough milk for her baby. The most common primary causes of insufficient breast milk production are breast surgery, placental fragments that have not left the uterus, hypothyroidism, breast hypoplasia, polycystic ovary syndrome, Sheehan syndrome. [17] When a woman experiences a lactogenesis disorder II [21], then most likely one of the above reasons is present: hormonal or neuroendocrine pathways are damaged, or there is an absence of an adequate amount of glandular tissue. Hypoplasia of the mammary glands or insufficiency of glandular breast tissue is a typical example of the root cause of lactogenesis II disorder. [21]
Secondary causes of impaired lactogenesis II are usually errors in the organization of breastfeeding and difficulties associated with it, such as pain when the baby sucks at the breast, ineffective sucking, poor latch, or early return to work. [17,22] These causes are much more common, but they can be corrected or prevented. It is important to distinguish between primary and secondary causes of impaired lactogenesis II if a woman has little milk. In addition, it is advisable to ensure that there are no secondary causes before looking for the primary cause of low milk supply due to the fact that primary causes are relatively rare.
How are female breasts formed normally?
But first, about the development of the female breast, so that later we can talk about its “under...”. At the beginning of puberty (that is, the age at which puberty begins), hormones called estrogens begin to be actively produced, which are responsible for:
- Breast cell growth
- Increase in the length of the ducts in it and their number
- Rapid growth of stromal tissue, that is, tissue (mainly connective) that forms the very “framework” of the female breast. The condition of the stromal tissue in the future determines its elasticity and ability to withstand sagging with age.
The hormone progesterone inhibits proliferation (that is, the rapid growth of connective and other tissue cells that form the female breast). So in the formation of breasts, in their growth to a size acceptable for a woman, it is not the amount of estrogen or progesterone that is important, but their ratio. By interacting, they start and then stop the growth of the mammary glands. The beginning of this process falls on the 9-10-11 year of life of girls. And it ends with 18-19 year old girls.
They say that a girl can have hypomastia only if her size is the so-called “zero”. And it is defined simply:
| The difference between measuring with a measuring tape under the chest and measuring with it at the protruding extreme points | Size |
| 10-11 | 0 |
| 12-13 | 1 |
| 14-15 | 2 |
| 16-17 | 3 |
| 18-19 | 4 |
| 20-22 | 5 |
| 23-25 | 6 |
| 26-28 | 6+ |
Subtract the first from the second measurement and you will get the bust size number.
It's about the norm. Now let’s explain why and how hypomastia occurs.
Breast hypoplasia
The literature on breast hypoplasia is still limited and known cases are not well documented, but underdevelopment of breast glandular tissue appears to be a rare occurrence. Neifert notes in his study that only 5% of women experience low milk supply due to anatomical changes in the breast or disease. [22]
Most of the known information about breast glandular deficiency comes from the plastic surgery literature, where it is often referred to as “bottle breasts.” [23] If a woman has a history of breast augmentation surgery, this may make the diagnosis of breast hypoplasia difficult. Breast surgery affects tissues anatomically necessary for lactation, and this in itself can lead to a situation where a woman is unable to successfully breastfeed her child. One way to determine whether breast hypoplasia is occurring is to visually examine photographs of the breasts before plastic surgery. [24]
The etiology of breast hypoplasia also remains unknown, although there are several theories regarding factors that may contribute to its occurrence. Juliette's study describes the development of altered breast tissue in women growing up in an agricultural region of Mexico who were prenatally exposed to relatively high levels of chlorine fertilizers that were used to treat crops and pollute the environment. [25]
Other theories, based on experiments with rodents, talk about embryonic pathology, exposure to high doses of estrogen, or chemical pollution in the environment. [20, 25, 26]
Hormones may also play a role. In women who have been treated for infertility, in particular for luteal phase failure, it is possible that due to low progesterone levels, the glandular tissue of the breast does not fully develop during phase II of lactogenesis. [2, 16] If a woman has a history of luteal phase disruptions and difficulties with breastfeeding, there is every reason to carefully examine the breasts for mammary gland hypoplasia as the main cause of impaired lactogenesis II.
Huggins notes that it is possible to identify women with hypoplastic breasts early and determine the likelihood of insufficient breast milk production. [27] Visually, the breasts of a woman with a lack of glandular tissue may appear widely spaced, “bottle” and/or asymmetrical in shape. [27] Visual assessment of the breasts can be supplemented by asking the woman how her breasts have changed during pregnancy and in the early postpartum period, whether stretch marks have appeared, how wide the distance is between the mammary glands, as well as how much milk the baby can suck from the breast and how much the volume of milk is expressed immediately after feeding - all this helps to successfully identify women with breast hypoplasia. The authors successfully identified women at risk for lactogenesis disorder II associated with underdevelopment of glandular breast tissue, but the sample in this study was small and there was no control group. [27] Further research in this area is needed. However, this study is the only published study attempting to identify women at risk for breast hypoplasia, and it provides important information. Depending on which part of the glandular tissue has not developed, several types of underdevelopment of glandular tissue have been identified. [20, 23, 27] Figure 1 shows some of these types.
Figure I. Types of breast hypoplasia (c); Taina Litwak 2009. from West D.Marasco The Breastfeeding Mother's Guide to Making More Milk. New York: McGraw-Hill: 2009.
A – incomplete development before puberty. B – poorly developed upper part, little breast tissue below. C – bottle-shaped with a convex areola. D – elongated, deviating towards the outer edge of the chest, with a very large areola. E – widely spaced with noticeable asymmetry. F – wide apart with little breast tissue.
Conservative treatment
Some methods that at first glance seem unrelated to the disease can help not so much to enlarge the mammary glands, but to change the perception of them by others. The following methods of conservative treatment of hypoplasia are used:
- If other women in the family suffered from a similar illness, then already during puberty the girl can be treated safely with medication. It includes vitamins, especially A, E, as well as oral contraceptives as indicated. Various folk methods with herbs (hops, etc.) can also be used.
- Exercises to strengthen the pectoralis major and minor muscles can slightly enlarge the breasts and lift them up. However, in most cases this is not enough.
- Exercises to strengthen your back muscles and straighten your posture can also significantly change the visual appearance of your breasts.
- Using underwear that will correct all imperfections.
- Sometimes it is recommended to slightly increase body weight, especially if it is deficient. But adipose tissue has fundamentally different properties, so you shouldn’t expect too much.
- The use of creams, especially those based on hormones, is unacceptable, despite their popularity. Indeed, during the period of their use, it is possible to achieve some enlargement of the mammary glands, but this is temporary and is formed due to tissue swelling. As a result, after the course the woman will return to her previous state, but often with obvious signs of mastopathy.
Practical significance
Ideally, breast assessment should be performed during pregnancy and the early postpartum period. During pregnancy, it is necessary to pay attention to how breastfeeding of previous children developed in order to find out whether there was a lack of milk and try to determine its possible causes. For all women who say that they had little breast milk, it is necessary to establish whether these were primary or secondary causes of lactogenesis disorder II. [27] The woman should also be asked about breast changes during pregnancy. If she says that the breast has changed minimally or has not changed at all, this should be a marker for paying close attention and checking its condition in the postpartum period. [20,21]
During the examination, pay attention to the symmetry of the breasts and whether the intramammary space—the distance between the breasts—is greater than or equal to 1.5 inches (3.81 cm). [20,27] Slight asymmetry is normal, but noticeable asymmetry may indicate an inadequate amount of glandular breast tissue. [28] Assessment in the early postpartum period typically includes checking for the presence or absence of postpartum breast engorgement. In addition to the anatomical features of the breasts described above, women with breast hypoplasia may notice only minimal breast swelling on the 3rd or 4th day after delivery. [28]
In terms of psychological assistance to women with a lack of milk, who want to breastfeed despite the difficulties associated with this, a key role belongs to midwives (in Russia, also doulas and lactation consultants - approx.).
Once it is determined that breast milk is low and it is suspected that breast hypoplasia may be the cause, treatment can be started that can help increase milk supply. Medicines and herbal preparations that are used to increase breast milk supply are called lactogenic drugs or lactogonics. [28, 29] (Table 1)
Many of the drugs, such as metoclopramide (Reglan) and domperidone (Motilium), work as dopamine receptor antagonists, resulting in increased prolactin release. [29,30] Domperidone is not available in the United States but is available through some compounding pharmacies. [33] (In Russia, domperidone can be bought in pharmacies under the trademarks Motilium, Motilak, Motonium, Domperidon-Teva, Domstal, Passazhiks, Motinorm, Motizhekt, Domet ", "Domelium" - before using any drug, you need to consult a doctor - approx.) However, domperidone, compared to metoclopramide, penetrates the blood-brain barrier less and passes less into breast milk. [29] Additionally, although it has not received FDA approval, domperidone is the only lactation enhancement drug that has been evaluated in a randomized, double-blind, controlled trial. [31]
Some herbal preparations have also been shown to be effective in increasing milk production in women with breast hypoplasia, although they remain poorly studied and there is a lack of rigorous scientific research on this issue [20, 29]. Fenugreek (finugrek, shamballa, helba) is a spice that is used in India and the Middle East, has the ability to increase the amount of milk by stimulating the work of the sweat glands. Mammary glands in mammals are modified sweat glands, therefore, by stimulating the sweat glands, milk supply can be increased. [20, 29, 32] An increase in milk supply is often noted 24 to 72 hours after starting fenugreek. [29] There are no standards for dosage and frequency of taking it, since the content of fenugreek in each capsule is not clearly defined. (Fenugreek capsules do not exist in Russia, but you can buy its seeds in spice stores - approx.) Taking fenugreek or any other lactogen should be done under the supervision of a doctor.
Another relatively well-known herb that has earned a reputation as a milk extractor is goat's rue (galega). [20, 30]
Usually, in combination with fenugreek, to increase the amount of milk, blessed thistle (Knikus pharmacius, curly thistle) is taken in order to activate blood supply to the breast [20, 32]. Effective lactogens must be selected individually for each nursing mother, and this should be done by a doctor. (In Russia, very few doctors have the necessary qualifications for this; a breastfeeding consultant would be more likely to be knowledgeable - approx.) The lack of evidence base is a strong obstacle to the spread of herbal milk extracts. Further research in this area is needed.
Table 1: Lactogens used for women with hypoplasia, their usual doses and side effects
| Lactogen | Mechanism of action | Dosage | Side effects |
| Domperidone | Dopamine antagonist. Increases prolactin levels. As prolactin levels increase, milk supply also increases. | 10-20 mg orally 3-4 times daily. Total: 30-80 mg per day [20, 31] | Not approved by the FDA, but is the most preferred lactogen internationally. In very rare cases, it can cause minor arrhythmias. Other rare side effects are dry mouth, skin rash, headache, stomach pain, and drowsiness. [20] |
| Metoclopramide | Stimulates prolactin production | 10-15 mg orally 3 times daily. Total: 30-43 mg per day [33] | Penetrates the blood-brain barrier and may cause drug-induced depression if taken for more than 3 weeks. In case of long-term use, dystonia (involuntary muscle spasms) may also occur [39]. |
| Fenugreek | According to the plan, it should help increase milk production by stimulating the sweat glands. The breast is a modified sweat gland. | 2 drops of tincture sublingually (under the tongue) 2-3 times a day or 2-4 capsules of 5 mg 3 times a day with meals. A tincture may be more effective than capsules. [19, 38] | When taking large doses, hypoglycemia, diarrhea, and shortness of breath may develop (worsening of asthma symptoms, if any). The maple smell of urine and sweat. This usually occurs when the body is oversaturated with fenugreek. |
| goat's rue | Belongs to the same family as fenugreek. Contains galegin, an alkaloid structurally related to metformin (more details here - approx.). Marked growth of breast tissue [20] | Tincture 1-2 ml 4 times a day or 1 capsule 1 time a day. If weight is more than 175 pounds (79.38 kg - approx.), then 2 capsules 3 times a day. | Hypoglycemia. May thin the blood. [20] |
| Blessed thistle | The mechanism of action on milk production is unknown. Often taken along with fenugreek. Antibacterial and anti-inflammatory agent [20] | Tincture 1-3 ml 2-4 times a day or 1-3 250-300 mg capsules 3 times a day. Use with fenugreek if possible. [20] | Virtually non-toxic. Very large doses may cause gastrointestinal distress. (This is one of the most bitter herbs to taste, so in folk medicine its tincture with honey is often used - approx.) |