Types of cystic formations
Based on the time of appearance, all cysts are classified into 2 categories:
- Congenital, or dysontogenetic, arise due to disruptions in the process of intrauterine development.
- Acquired ones appear as life progresses.
According to the mechanism of development of cysts, there are:
- Retention - the most common. They are formed if the excretory duct of the gland is compressed or blocked from the inside. The secretion has no outlet, accumulates and stretches the surrounding tissue.
- Ramolitic - arise at the site of dead cells, for example, in the brain after a stroke.
- Parasitic is a capsule within which the parasite is located. In this way, the helminth protects itself from the body’s immune attacks.
- Traumatic ones form at the site of bruises due to the accumulation of tissue fluid.
- Tumor - lined with epithelium with signs of metaplasia; inside there are seals and places where fluid accumulates.
CLASSIFICATION OF ATHEROMAS
- Congenital epidermal cysts
(Atheromatosis) appear as small formations up to 5 mm. Their appearance is due to the genetically defective structure of the sebaceous glands, accompanied by a violation of the release of sebum to the outside. - Acquired atheromas
Secondary, or formations that appear during life, which are ducts of the sebaceous glands with clogged lumens, dilated and filled with viscous contents. These include common sebaceous gland cysts, dermoids, and steacytomas.
Is treatment necessary?
The doctor decides what to do with the identified cyst. It depends on its size, contents, patient complaints:
- Small formations, if they do not bother you, there is no rapid growth and no risk of degeneration into oncology, just observe.
- If the formation is large, causes pain, impairs the functioning of the organ in which it is located, grows quickly, festers or has signs of malignancy, it is removed. After surgery, the tissue is sent to a histology laboratory for examination.
Classic surgery is an open intervention with removal of the cyst using a scalpel. If possible, preference is given to gentle options - using endoscopic techniques, small incisions, and a short rehabilitation period.
The formation is removed using instruments inserted through incisions in the skin, or aspirated with a vacuum device. To avoid relapse, in the latter case it is necessary to cauterize the walls of the cyst. This can be done with a laser, injecting a sclerosant, treating the capsule with radio waves or cold (cryotherapy with liquid nitrogen).
Carrying out the operation
It is often performed under general anesthesia, but if it is small and located subcutaneously, local anesthesia may also be used.
As a rule, a skin incision is made and, if necessary, the cavity is opened, access is provided and complete excision is performed. If possible, laparoscopy is performed; if this is not possible, then open intervention is performed.
Surgical removal of the formation can be performed on part of an organ or the entire organ. We are, of course, talking about paired organs. Removal of the ovary is recommended for significant size pathological formations and for postmenopausal women. Removing one kidney with a cyst is only advisable if it is not possible to save the organ. The liver and pancreas can only be resected to the extent that the remaining part of the organ can cope with its function.
That is why, when pathology is localized in the liver, pancreas or other unpaired organs, it is recommended to eliminate them at the earliest stages, including in children, since an increase in the size of the formations can lead to damage to most of the organ and the impossibility of performing radical surgery.
What types of cysts are there in the human body?
Cystic formations can occur in any human organ. Most often, women develop cysts of the ovary, cervix, Bartholin's gland, and mammary gland. In men, a coccygeal cyst occurs, in patients of both sexes - a cyst of the thyroid gland, brain, paranasal sinuses, and larynx.
Ovarian cyst
The formation may be asymptomatic and is discovered accidentally during a pelvic ultrasound. If the size is large, it stretches the organ capsule and causes pain. A woman may also complain of non-cyclical spotting from the genital tract, disruptions in the menstrual cycle, and inability to become pregnant. In severe cases, torsion of the ovarian cyst pedicle occurs - an acute surgical pathology. It is accompanied by severe pain in the lower abdomen and requires urgent intervention. Otherwise, tissue necrosis may occur and peritonitis may develop.
The treatment is carried out by a gynecologist. He examines the woman, decides whether surgical intervention is necessary and what kind. If the formation has a low oncogenic risk, it is usually removed endoscopically. Sometimes diagnostic laparoscopy with puncture and biopsy of the formation is performed before surgery. If atypical cells are found in it, you may have to perform an oophorectomy (removal of the cyst along with the organ) or adnexectomy (removal of the fallopian tube from the affected side).
Physiological cysts also form in the ovaries, so before removal the patient is observed and ultrasound scans are performed several times, including transvaginally.
Pilonidal cyst
It occurs in men at a young age - up to 30 years. More often this is a congenital formation. A hole is visible in the skin in the area of the sacrum or coccyx. This is an epithelial passage that goes deep into the tissues. Another option is that a cyst forms around the hair, especially during puberty. As long as there is no inflammation in the tissues, there are no symptoms. If microbes get inside, the patient complains of pain, redness, swelling of the skin, and pus is released from the hole.
Conservative treatment can relieve the symptoms of inflammation. Outside of exacerbation, the formation is excised with a scalpel.
Bartholin's gland cyst
It is localized in the thickness of the labia majora. If it is large in size, it can cause pain to a woman while walking, sitting, or intimate relationships. If its contents fester, the pain intensifies, the surrounding skin becomes hot and red.
Sexual infections, poor hygiene in this area, wearing tight underwear, and weakened immunity contribute to the formation of Bartholin gland cysts.
Removal of the cystic formation is carried out using a laser or traditional surgery. After the operation, you may feel dry in the vagina, as the secretion of the Bartholin gland serves as a lubricant for the external female genitalia. If possible, during the intervention, a new excretory duct is formed to allow secretions to come out.
Cysts in the cervix
Nabothian retention cysts are most often diagnosed in the cervical area. They are formed when the mucous secretion has no outlet. This happens due to chronic inflammation, after abortions and other interventions. Sometimes the appearance of a formation is provoked by childbirth, hormonal changes during menopause, or wearing an intrauterine device. Less commonly, endometrioid cysts are detected in the uterus; they fill with blood during menstruation and can be localized in any organ. They are manifested by pain, bloody discharge, which coincides with menstruation.
A Nabothian cyst often occurs without symptoms; a woman may feel pain, discomfort during intimacy, and contact bleeding. Sometimes education is an obstacle to conceiving a child.
A cyst is diagnosed during a gynecological examination and a test is performed with iodine preparations or acetic acid to identify the risk of malignant degeneration. Cervicoscopy, cytology, and biopsy if indicated are performed. Only after all these studies the doctor will determine further treatment tactics.
A surgical removal method or more gentle methods are used: cryodestruction, laser, radio wave exposure, chemical cauterization. If a woman has not given birth and no signs of metaplasia have been detected, doctors try to preserve the cervix as much as possible.
Breast cyst
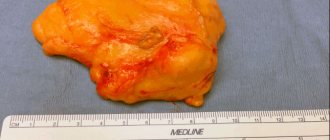
Cysts form from the ducts of the gland. They are single (solitary) and multiple. The capsule is formed by connective tissue or overgrown epithelium. Fatty cysts are formed from the sebaceous gland if its outlet is clogged with epithelial cells and fat.
The stimulus for the appearance of cavity formations can be injuries, hormonal changes, and stress.
Small cysts do not manifest themselves in any way. With an increase in size, a woman can notice the formation and palpate it. It is necessary to contact a mammologist for further examination. Examination by a specialist, palpation, ultrasound, mammography will help make an accurate diagnosis and select treatment.
Modern methods of treatment are sclerotherapy and laser exposure. A puncture is performed through the skin under ultrasound guidance, the contents are aspirated and sent for cytology. A substance is injected inside to scleros and glue the walls of the cyst, or the capsule is treated with a laser. This method will not be suitable if there are signs of malignant growth, the formation is large (more than 1.5 cm), it is in the stage of purulent inflammation, and has a multi-chamber structure. Then a surgical operation is performed - sectoral resection, that is, they are removed along with part of the mammary gland.
Brain cyst
The formation can be congenital or acquired, located inside the brain or between the meninges. As it increases, it compresses the surrounding tissues, causes headaches, signs of intracranial hypertension appear, and sometimes focal symptoms (impaired vision, sensitivity, motor sphere). Possible dizziness, sensation of pulsation, noise in the head.
Intracerebral cysts form at the site of necrosis during a stroke. Sometimes parasites enter the brain through the blood and become encapsulated. The appearance of cystic formations is facilitated by injuries, inflammation, surgical interventions, and intrauterine development disorders.
Diagnosis is carried out by a neurologist; additionally, CT and MRI of the brain are prescribed. Depending on the diagnosis, treatment is chosen.
Thyroid cyst
An organ in which cysts are often found. They are visible on ultrasound. In suspicious cases (the formation has several chambers, inclusions, epithelial growths), additional tests and a biopsy are performed to exclude oncology. Small asymptomatic cysts are not removed. For large sizes and confirmed malignant growth, surgery is performed.
A cyst in the thyroid gland can manifest itself as pain, difficulty swallowing, and changes in voice. If the walls are formed by glandular tissue, the level of thyroid hormones changes.
Treatment is conservative, gentle surgical (puncture and sclerotherapy or diode laser exposure). If this does not help, the formation reappears, is actively growing, there are atypical cells in the punctate, an operation is performed - half or the entire organ is removed.
Cysts of ENT organs
Laryngeal cysts at the level of the vocal folds are most often caused by large vocal loads. In other sections, they are formed when the excretory ducts of the glands are blocked. The patient may experience changes in voice, sore throat, difficulty breathing, cough, or the presence of a foreign body.
An otolaryngologist examines the larynx and performs a puncture if necessary. They may prescribe an ultrasound, CT scan, or endoscopic examination.
The formation is observed for some time; it may resolve on its own. If it begins to grow, becomes inflamed, or bothers the patient, remove it. Treatment is surgical, often using endoscopic techniques. After the operation, histology is performed.
The cyst is also found in the paranasal sinuses, most often in the maxillary sinus. It may appear due to problems with teeth or developmental features of the nose and sinuses. It manifests itself as pain under the eye, a feeling of fullness, frequent exacerbations of sinusitis with nasal congestion, and discharge along the back wall of the throat. The diagnosis is confirmed by x-ray. The punctate has a yellow color and a thick consistency. After the puncture, anti-inflammatory treatment is carried out. In difficult cases, endoscopic or open surgery is performed.
LASER REMOVAL OF atheromas in “EL. EN."
Do you want to get great results?
Choose laser removal of atheromas with short rehabilitation and no scars. Our surgeon will recommend the optimal laser treatment method and perform the procedure. 1 Photocoagulation
The method is suitable for eliminating atheromas with a diameter of up to 5 mm. High-intensity laser radiation is directed (non-contact) to the neoplasm; as a result of the impact, the capsule and its contents are completely evaporated. After the procedure, a crust remains at the site of the atheroma; no stitches are required. After a certain time, the crust disappears, the resulting wound gradually heals, and the skin becomes even.
2
Excision
The method is most often practiced in situations where the diameter of epidermal cysts is up to 20 mm (but there are exceptions). The surgeon cuts the skin (with a laser knife or scalpel), stretches the cyst shell and evaporates the tissue around it with a laser - this is how the atheroma is separated from healthy structures. Then drainage is placed for several days.
3
Evaporation
It is practiced when the diameter of atheromas exceeds 20 mm. The surgeon opens the capsule, removes its contents, and then acts on the capsule with laser radiation - it evaporates. The operation is completed by installing drainage and suturing.
Our clinic also performs laser removal of ingrown toenails - the cost starts from 6,000 rubles. Sign up online or by phone.