Complications in the form of local infectious and suppurative processes after back surgery account for from 1% to 8% in the overall structure of all interventions. Among surgical manipulations on the spine associated with the installation of implants and metal structures, the frequency of this kind of inflammatory reactions is significantly higher (6%-20%). Infectious-purulent post-surgical pathogenesis can negatively affect the final outcome of the applied tactics for surgical correction of the spine, even if it was performed flawlessly.
A good calm stitch after surgery.
Despite the enormous achievements of spinal neurosurgery in the field of intra- and postoperative infection control, infections and purulent inflammations still remain the leaders among all possible complications. Various factors can push the development of unfavorable pathogenesis: from the specifics of the patient’s body to preoperative, operational and postoperative disorders.
Infections and purulent inflammations in the projection of the surgical field can be superficial and deep, early and late. Moreover, each type requires emergency medical care aimed at intensified eradication of the pathogenic environment. Intensive therapeutic measures are necessary not only to increase the likelihood of a positive functional outcome in relation to the operated part of the back. Their value also lies in preventing the development and spread of sepsis throughout the body, which poses a great threat to human life.
The more extensive the intervention, the higher the likelihood of complications.
An infectious complication (IO) is a rather serious problem, not always easily solved, so every patient should be aware of it, regardless of whether he has it or not. As they say: forewarned is forearmed. Next, we will inform you in detail about complications of an infectious, purulent nature after back surgery: after removal of a hernia, disc replacement, resection of tumors, interventions using metal structures, etc. We will also be sure to familiarize you with how specialists treat patients in such a situation.
Symptoms and signs of complications
Infectious and purulent reactions in the area of surgical intervention are usually classified into 2 main types:
- superficial (suprafascial) – infection affects exclusively the skin surfaces and subcutaneous fat layer at the incision site;
- deep - the infection penetrates deeper, affecting fascial and muscle structures (advanced cases lead to infection of bone tissue).
Superficial infection of the wound area occurs no later than the first month after the operation; the causative agent is usually staphylococcus. The deep development of harmful microflora is more associated with long-term periods, and, as a rule, appears within 3 or more months after the surgical session.
One example of an open seam.
The first specific manifestations of the dissemination of pathogenic microorganisms within the surgical field are:
- redness of the tissue around the seam;
- compaction;
- painful sensations.
Regardless of the type of pathogenic agent, the activated inflammatory process in the area involved in the surgical intervention can also be judged by the presence of one or more symptoms:
- discharge of serous, serous-purulent fluid from the superficial tissues of the incision;
- limited tissue swelling;
- localized soreness that tends to increase;
- local hyperemia of the skin with an increase in local temperature;
- purulent discharge from the depths of the surgical wound, the presence of fistulas;
- spontaneous dehiscence of the suture with separation of the edges of the wound, if in addition there is pain and/or hyperthermia of the body (total body temperature up to 38 degrees or more).
Inflammation on the back in and around the surgical access site does not always indicate an infectious complication. Swelling, pain, and redness almost always appear immediately after surgery as a natural reaction of the body to surgical aggression. And such symptoms may be a variant of the norm, but with the condition that after 3-5 days these three signs are eliminated after minimally invasive surgery (without the use of implants). When it comes to extensive open surgery with fixation of metal structures or prostheses, a dynamic reduction in the severity of inflammation of injured tissues in the early period is considered normal, with final relief from it within a maximum of 7-10 days.
Types of fistulas
The classification of fistulas is diverse; each organ has its own gradation of fistulas by location, sometimes the degree of involvement of surrounding tissues, and even by the volume of secretion released through the fistula.
Complete fistulas have an external and internal opening, incomplete fistulas have only an internal opening.
Those opening in the skin are called external fistulas, while fistulas connecting organs are called internal .
Depending on the number of organs involved in the process, internal fistulas can be combined or isolated . Isolated fistulas are named after the organ that gave rise to them: pancreatic, biliary, intestinal, vaginal, ureteric, and so on.
When there is an anastomosis of two or more organs - a combined type of fistula - a “combined” name is used, so with a fistula between the rectum and the vagina - rectovaginal fistula, with a fistula from the gallbladder to the stomach - cholecystogastric fistula, between the pancreas and the stomach wall - pancreatogastric or pancreas-gastric fistula.
According to the number of tracts, fistulas are divided into single-channel or simple and multi-channel or complex , as well as branched or indirect and unbranched or direct .
According to the condition of the tissues and course - infected or complicated fistulas, as a rule, purulent and “clean” uninfected or uncomplicated fistulas with the release, for example, of bile or pancreatic juice.
| Depending on the number of holes | Complete fistulas | They have two openings - they connect two organs to each other or one organ to the surface of the skin. |
| Incomplete fistulas | They only have one hole. | |
| Depending on the location of the second hole (for complete fistulas) | Internal fistulas | Connects internal organs. |
| External fistulas | Connect internal organs to the surface of the skin. | |
| Depending on the number of organs involved | Isolated fistulas | They are named after only one organ that gave rise to the fistula. |
| Combined fistulas | Two or more organs are involved. | |
| Depending on the course of the fistula | Single channel (simple) | One fistula tract. |
| Multichannel (complex) | Several fistula tracts. | |
| Branched (indirect) | There is a branching of the fistula. | |
| Unbranched (straight) | No ramifications. | |
| Depending on the presence of complications | Uncomplicated (uninfected) | There are no signs of infection. |
| Complicated (infected) | There are signs of an infectious process in the fistula. | |
| Depending on the current | Primary | The fistula was discovered for the first time. |
| Recurrent | The process either subsides or reactivates: inflammation develops, new fistula tracts appear or old ones open. |
Fistulas are divided into primary and chronically occurring - recurrent , when the process either subsides or becomes inflamed again with the formation of new passages and, sometimes, the closure of old ones.
A rectal fistula is classified in relation to the anal sphincter, and fistulas that are localized above the anus and go around it like a horseshoe, with an opening into the rectum, are also graded according to 4 degrees of complexity.
Complete pancreatic fistulas can be small with the release of up to half a glass of juice, medium - up to 700 milliliters and large.
There are as many classification options as there are types of fistulas in human nature.
Consequences due to the patient's condition
Initially, the main diagnosis was the severe clinical condition of the patient admitted to the hospital.
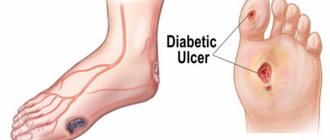
Concomitant diseases and conditions that reduce the body's resistance to pathogens or interfere with normal wound regeneration:
- diabetes;
- immunosuppression;
- obesity;
- dermatoses;
- oncology;
- elderly age;
- infancy.
- The presence of an active infectious bacterial, pyogenic focus in absolutely any part of the body (dental caries, infections of the genitourinary system, throat/nose, etc.).
Intraoperative reasons
- Low degree of “cleanliness” of the surgical wound. In practice, “clean” operations are much less likely to provoke complications than conventionally “clean” or “dirty” ones. The riskiest spinal procedures are those that were initially performed for abscesses, such as spondylitis.
- Violation of the implementation of technical techniques of the selected surgical intervention.
- Failure to comply with aseptic and antiseptic standards in the operating room.
- Extensive soft tissue trauma (forced or accidental), a technically complex and lengthy operation.
- Severe injuries to blood vessels, muscle fibers with a surgical instrument, resulting in the need for a blood transfusion.
- Surgical drainage, it can promote the migration of pathogenic bacteria from the skin into the wound. In many cases it is impossible to do without it. Therefore, drainage should be carried out strictly limited in time, and drainage systems (preferably a closed suction type) require very careful handling.
Drainage of the wound.
- Failure to comply with the conditions to ensure normal hemostasis, which affected the volume of intraoperative blood loss, wound bleeding after surgery, the formation of hematomas, etc.
- Poorly performed wound suturing - non-compliance with the technology of applying a suture thread, incorrectly chosen technique and/or materials.
Brief anatomical summary
The upper jaw contains the maxillary sinus (maxillary sinus), the alveolar process located under the sinus and a number of other anatomical formations. In the absence of pathology, the roots of the teeth of the upper jaw are tightly fixed in the alveolar process. Normally, between the tips of the roots of the teeth and the sinus cavity there is from 3 to 15 mm of bone tissue.
A fistula is a pathological course formed as a result of an infectious-inflammatory process. Due to the fact that during sinus lifting the amount of bone tissue is reduced, when an infection enters the surgical wound, the soft and hard tissues of the alveolar process and the bottom of the maxillary sinus melt. An oroantral fistula is formed, a fistula connecting the sinus cavity with the oral cavity.
Postoperative reasons
Inadequate postoperative wound care
- insufficient or, conversely, too frequent bactericidal treatment of the wound and dressing procedures;
- low-quality provision of cleaning wound areas, replacing tampons and drainages;
- non-compliance with aseptic standards during dressing procedures (poor disinfection of equipment, use of non-sterile napkins/bandages, failure to wash hands and use disposable gloves on the part of the health worker, the health worker is a carrier of the MRSA strain of infection, etc.);
- non-compliance with the rules for keeping the wound dry and covered with a bandage (the patient wets the wound with water ahead of time and/or exposes it, contrary to the prohibition voiced by doctors);
- incorrect dressing technique at home, performed by the patient independently.
Errors or neglect of the principles of the rehabilitation regime and treatment measures:
- incorrect course of antibiotic treatment recommended for the patient (type, frequency, dose, period of use of the drug), omissions or complete absence of mandatory antibiotic therapy after any spinal surgery;
- the patient’s failure to comply with the postoperative physical activity regimen, which can also increase the risks of IO (early refusal of physical rest, unacceptably high load on the operated area, unauthorized self-prescription of exercises, ignoring the wearing of orthopedic corsets, etc.).
Treatment of an infectious (purulent) focus
The basic principle of treatment, which applies equally to all patients with a similar complication, is based on fundamental wound debridement and intensive antibiotic therapy. However, there cannot be any templates in the way medical care is provided; the treatment program is developed individually and only on the basis of the nature and severity of the postoperative consequences. After a diagnostic assessment of the affected area, different strategic approaches can be applied with possible layouts:
- surgical opening of a purulent focus with evacuation of the pathological contents of the wound and removal of foci of necrosis;
- cleaning of the pyogenic component, washing the wound with a stream of antibacterial solution, intrawound administration of an antibiotic;
- use of ultrasonic/laser cavitation of the purulent cavity;
- application of VAC therapy methods based on vacuum systems;
- loose gauze-antiseptic packing and flow-wash drainage of the wound;
- installation of special suction and/or irrigation type systems;
- in case of deep infection, it is more often recommended to remove implanted disc implants, metal structures, and endofixators in order to perform the most complete sanitation and eradication of foci of infection. In isolated cases, it is possible to immediately replace the removed instruments/implants with new products.
Local treatment using the above methods, as a rule, includes immobilization of the patient. Local events usually last from 5 days to 14 days. However, with a generalized pathogenic process and little progress in treatment, they can be extended for a month or longer.
Bacterial culture to detect colony growth.
The next mandatory treatment measure is general antibacterial medication. It is selected taking into account the results of bacteriological culture and the sensitivity of a particular pathogen to antibiotics. General antibacterial therapy (mainly injection) is prescribed on average for 6-8 weeks. Doctors are skeptical about taking antibiotics orally for this consequence, not considering this method reliable.
In combination with antibiotic therapy, detoxification, immunocorrective, and symptomatic treatment methods must be present. A well-developed algorithm for combating the developed infectious-inflammatory, pyogenic environment allows in the overwhelming majority of cases to arrive at a positive prognosis.
Diagnostics
Determining the presence of the fistula itself is not difficult. To assess its depth and diameter, it is possible to use a special probe inserted into the resulting oroantral tract. To assess the extent of inflammation and the presence of additional passages, it is possible to use radiography of the upper jaw with the introduction of a contrast agent.
Evaluation of the presence of a foreign body or apex of the tooth root is carried out during radiography or directly during the operation to close the fistula. If there is no effect from antibacterial therapy, it is possible to culture the microflora to determine its resistance to antibiotics of various types of action.
Prevention, minimizing the risk of developing wound infection on the back
Preventive measures are aimed at identifying and taking into account all possible provoking factors that can cause complications. Based on this, adequate actions on the part of the medical staff and the patient must be fully ensured throughout the entire perioperative period. This is the only way to really eliminate or maximally protect a person from a local infectious attack. Let us list the leading principles of prevention of IO in spinal column surgery.
- Preoperative comprehensive (extended) diagnostics of the body, including bacteriological examinations of urine and blood. It is also important to undergo a dental examination, examinations by an ENT specialist, and a BAC culture of the oral cavity. If high diagnostic titers of infections are detected in the body before surgery, it is necessary to undergo specific targeted treatment.
- At the preoperative stage, ensuring proper treatment of all decompensated chronic diseases, which are potential “amplifiers” of non-healing and infection of surgical wounds. Diabetics and patients with autoimmune disorders require special attention throughout the perioperative period! Surgery is allowed only when stable compensation for the chronic disease is achieved.
- The intervention is carried out exclusively in high-level clinics, where all neurosurgical canons are strictly followed - from patient preparation, strict adherence to surgical technology and antiseptic standards to impeccable provision of rehabilitation care.
- Prophylactic use of intravenous antibiotics for all types of surgery, be it resection of intervertebral hernia, neoplasms or elimination of instability, curvature of the spine through implants or grafts (the day before, intraoperatively, in the postoperative period).
- Upon returning home, impeccably follow the recommendations provided by the doctor for the care and treatment of the postoperative incision area.
- Strictly adhere to all medical and physical regimens after surgery.
- At the first symptoms of painful discomfort in the area of surgical access (pain, burning, swelling, redness, hyperthermia, etc.), immediately see your doctor.
Remember that infectious complications at the initial stage are easier to stop and eliminate than its advanced forms, and in some cases without surgery. And, of course, to prevent implant rejection, loosening, displacement, breakage, and migration across the anatomical expanses of a foreign body. Early diagnosis and timely treatment of IO are fundamental criteria for a successful outcome, less severe and long-term recovery after spinal surgery.
Why does the suture fester after surgery?
When dissecting the abdominal wall, be it a straight, transverse or oblique incision, it passes through the skin, subcutaneous fat, muscles, fascia or aponeurosis, preperitoneal tissue, and peritoneum. In some cases, the muscles are not cut, but moved apart, which subsequently speeds up healing. After abdominal surgery is performed, all layers of the abdomen are sutured. The technique of this manipulation will depend on where and how the access was performed. To make healing more likely to occur by primary intention, they try to sew each layer to a homogeneous tissue. Layer-by-layer suturing of a wound usually involves about 3-4 rows of sutures.
- After mid-upper laparatomy (access to the organs of the upper abdominal cavity), the parietal peritoneal layer, preperitoneal tissue and transverse fascia are picked up first. Catgut is used, which then dissolves on its own and does not require removal of suture material. Second row - separate interrupted sutures with silk, lavsan, nylon on the white line of the abdomen. This material does not dissolve and must be removed after the wound has healed. The third row of interrupted sutures is placed on the skin.
- Lower median laparatomy involves the first row to continuously suture the peritoneum and fascia with catgut, the second - separate sutures from catgut to the rectus abdominis muscles, the third - using synthetics with separate sutures to close the sheath of the rectus muscle, the fourth - to restore the skin and subcutaneous tissue with a discontinuous suture.
- Caesarean section usually involves a transverse approach along the suprapubic skin fold. The wound is sutured, starting from the parietal peritoneum in the longitudinal direction, with catgut continuously. The muscles are sewn continuously or with separate sutures using absorbable material. Aponeurosis - synthetics. Subcutaneous tissue - with catgut. The skin is sewn either with separate synthetic sutures, or with a continuous percutaneous self-absorbing suture, or fastened with metal staples.
To reduce the risks of postoperative inflammation even before surgery, in some cases, the patient is preventively prescribed cephalosporin antibiotics. The surgical field is treated with antiseptics before incision and after suturing. An aseptic bandage is applied to the area of the sutured wound. The sutures undergo specialized care until removal or complete healing - treatment with alcohol dyes and antiseptics (iodonate, chlorhexidine, ethyl alcohol, hydrogen peroxide) and change of dressings on the first, third, sixth and tenth days after surgery. The suture is carried out using the open method without signs of suppuration and treated with brilliant green.
note
The more carefully the sutures are cleaned, the lower the risk of suppuration and healing with the formation of a rough scar.