During puberty, all young girls begin to develop mammary glands. All girls are individual and therefore their breast development is different. Some young girls are naturally gifted with curvaceous figures. However, if the bust becomes much larger, then we can talk about irregularities - the so-called gynecomastia in women, that is, an increase in fatty tissue in the breast.
Solve your life problems. Change your destiny!
Ask the Universe for whatever you want: ⭐ Love ⭐ Money ⭐ Career ⭐ and more
To learn more
What is gynecomastia in women? This is a deviation from the norm of the mammary glands, which is expressed in a unilateral or bilateral increase in volume due to the abundance of glandular or adipose tissue. It manifests itself as thickening and enlargement of the breasts, as well as a feeling of heaviness and pain on palpation of the mammary glands. In some cases, the disease goes away on its own. If drug treatment is ineffective, surgery is prescribed. ICD 10 code N62. If your child has symptoms of gynecomastia, do not delay visiting a doctor and getting treatment.
Types of gynecomastia
Depending on age, there are different types of gynecomastia in women:
- Infants and newborns. If a medical examination of the mother did not reveal diseases from mammology, then up to 12 months this is the norm and does not require treatment, and the physiological phenomenon disappears after the child turns one year old.
- Gynecomastia in girls. As a rule, the mammary gland in girls begins to develop at the age of 9, but it can develop at the age of 14-16. It depends on the girl's development and is passed on from mother to daughter (that is, if a mother's breasts begin to develop at age 10, the daughter will likely be 10 as well). If your daughter’s breasts begin to develop at the age of 5-6, this is not a reason to be happy, this is a reason to consult a mammologist.
- Gynecomastia in children. The disease begins to develop in adolescence (usually from 12-15 years). The reason for the occurrence of this pathology is that hormonal changes occur in the body of a teenager. In this case, it is worth consulting with a doctor to adjust the diet and observe on the spot (the so-called registration at the clinic).
- Female gynecomastia. If an adult woman has breast enlargement, an urgent consultation with a doctor is necessary.
University
→ Home → University → University in the media → If a girl matures ahead of time
Puberty is one of the most difficult periods in a girl’s development. Enlargement of the mammary glands (thelarche) is often the first and only sign of the manifestation of true precocious puberty in girls.
Puberty is one of the most difficult periods in a girl’s development. During the transition from childhood to puberty, a complex of physical, hormonal, and mental changes occur in the body, and secondary sexual characteristics appear and progress. The leading role in this case is played by the hypothalamic-pituitary-gonadal system, an increase in the activity of which leads to pubertal secretion of ovarian hormones.
Breast enlargement (thelarche) is often the first and only sign of the manifestation of true precocious puberty (iPPD) in girls. During the initial examination, it is difficult to clearly distinguish between the onset of the full form of premature puberty and isolated growth of the mammary glands. With the simultaneous detection of thelarche, genital (pubic and axillary) hair growth, and accelerated growth rates in the patient, the diagnosis of true precocious puberty is beyond doubt. More often, the pediatrician has to deal with only one or two symptoms (mainly thelarche), each of which may be a manifestation of the full form of PPR, incomplete sexual development, or other diseases requiring urgent hormonal therapy. Patients with premature thelarche after 2–3 years of life need a particularly thorough examination by a pediatric endocrinologist. This is due to the high probability of further progression of puberty due to the instability of gonadotropic regulation.
The incidence of true precocious puberty is 1 in 5,000–10,000 girls. In 2009, 114 such children were registered in Belarus (28 of them for the first time).
There are two types of iPPD: central and idiopathic. The first develops due to disorders in the hypothalamic or pituitary regions, including tumors, traumatic injuries (birth trauma), and radiation. In most cases, the cause of iPPR cannot be determined when using modern diagnostic methods, and then it is regarded as idiopathic. This form reaches 75% of cases of premature puberty.
The mechanism of occurrence of true precocious sexual development has not been disclosed. It is assumed that the main impulse that activates gonadotropic function in girls with physiological (normal) and true premature puberty is an increase in the pulse secretion of luteinizing hormone releasing hormone (LH-RH).
Until recently, age restrictions on the timing of normal puberty in girls were the subject of debate. Recent studies by American authors have led to a revision of the criteria proposed by the American Academy of Pediatricians. According to these recommendations in the United States, the onset of puberty is considered premature in girls younger than 6 (African-American) and 7 (white) years, and not 8, as was previously accepted. In the Netherlands, the average age of onset of thelarche decreased by only 3 months between 1965 and 1997. Such significant discrepancies in the results are explained by the peculiarities of the methodological approach and epidemiological characteristics (for example, a significant increase in the incidence of obesity in the United States compared to European countries). According to the classification of pediatric endocrinological diagnoses adopted by the European Association of Pediatric Endocrinologists in 2007, breast enlargement in girls under 8 years of age is regarded as a sign of precocious puberty.
The main goal of diagnosis is to determine the form of the disease, the causes of increased secretion of hormones of the hypothalamus-pituitary axis and target organs, the likelihood of progression of the pathology and the need for treatment. It is necessary to take into account the characteristics of the clinical status, anamnestic data, timing of onset, severity and nature of development of secondary sexual characteristics. Specific markers are considered data from visual research methods and the results of a test with an LH-RH analogue.
In most cases, clinical, instrumental criteria, and the basal hormonal profile of girls correspond to the results of a GnRH stimulation test, which remains the “gold” standard for diagnosing iPPD.
The need for it is due to the fact that a single determination of the basal values of luteinizing (LH) and follicle-stimulating (FSH) hormones in patients with iPPD is not very informative due to the wide range of individual fluctuations. A rise in LH levels of more than 10 IU/l indicates pubertal secretion and indicates a true variant of PPR. Some researchers also take into account the concordance of increases in LH and FSH in response to stimulation. The pubertal response is characterized by a predominance of the LH peak over FSH.
Topical diagnosis for premature puberty consists of a CT or MRI scan of the brain. The central cause (hypothalamic hamartoma, glioma, arachnoid cyst of the bottom of the 3rd ventricle and chiasmatic-sellar region, hydrocephalus, irradiation of the hypothalamus) is detected in girls in approximately 20% of cases.
The goal of drug treatment of true precocious puberty is to improve growth prognosis and reverse the development of secondary sexual characteristics.
Indications for treatment of girls with central premature puberty: complete iPP (including menarche); pubertal LH level and LH/FSH ratio are higher than the diagnostic value after LH-RH stimulation; rapidly progressing puberty; a pronounced decrease in the predicted growth of the child relative to the genetic one or below the 3rd percentile for population indicators.
GnRH agonists have been used to correct iPPD for more than 20 years. Deposited forms of drugs are most widespread in our country. The continuous action of GnRH leads to blocking of receptors on the gonadotropic cells of the pituitary gland and reduces the secretion of its hormones, thereby reducing the levels of sex steroids. The effect of paradoxical suppression of gonadotropic function by active LH-RH agonists underlies the clinical use of these drugs in the treatment of iPPD. Low hormone levels persist throughout the course of treatment, provided the frequency of administration is observed once every 28 days.+
An important aspect is the restoration of puberty. In girls, after the last injection of the drug, the levels of gonadotropic and sex hormones increased to the initial pubertal values after 3–12 months. Restoration of menstrual function was observed 0.5–2 years after cessation of therapy.
The criteria for completing treatment with GnRH agonists are reaching the age of physiological (normal) puberty and improving the prognosis for final growth. All published data indicate a positive effect of LH-RH agonists on the final growth of the child. Other factors influencing effectiveness are timely initiation and duration of correction. This highlights the importance of early diagnosis and drug therapy in children with early onset of secondary sexual characteristics.
Case from practice
Patient L., 1 year 8 months, was admitted to the Republican Children's Endocrinology Center at the 2nd City Children's Clinical Hospital in Minsk with complaints of enlarged mammary glands over the past 2 months, single bleeding from the vagina (at 1 year 6 months). From the anamnesis: a girl from her first pregnancy. Body weight at birth - 3,100 g, height - 50 cm. She was breastfed for up to a year; in the second year of life, the mother notes frequent colds. On examination, the mammary glands are enlarged in size (corresponding to Tanner stage 4); sparse, weakly pigmented pubic hair. Within six months, the child experiences accelerated growth - more than 10 cm in 6 months, growth exceeds the 97th percentile for a given age and gender. Ultrasound examination of the pelvic organs: the uterus is pear-shaped, enlarged in size (17x13x35 mm, M-echo 2.2 mm), right ovary 14x7 mm, left ovary 13x6.5 mm, fine-meshed echostructure, echogenicity is normal. Conclusion: echoscopically the uterus corresponds to 7–8 years. Ovaries without pathology.
X-ray of the left hand and wrist: bone age is ahead of the passport age and corresponds to 2 years 6 months.
During a hormonal examination, the basal levels of the gonadotropic hormones LH and FSH are increased compared to the age norm, the estradiol level is normal. For differential diagnosis between iPPR and isolated mammary gland enlargement, a test with a gonadoliberin analogue (LH-RH) was performed, while the maximum stimulated LH surge exceeded the initial level by 8 times and amounted to 16 IU/l.
MRI of the pituitary gland revealed no pathological changes.
Based on the results of the examination, a diagnosis was made: true idiopathic premature sexual development. Treatment with gonadotropin-releasing hormone analogues at a dose of 1.8 mg per month was prescribed. During therapy, a regression of secondary sexual characteristics was noted: the mammary glands shrank, menstruation stopped, the growth rate corresponded to pre-pubertal (5–6 cm/year), and the progression of bone age stopped.
Main criteria for progressive central premature puberty
| Sign | Slowly progressing puberty | iPPR |
| Puberty stage | stabilization/regression of secondary sexual characteristics+ | progression to stage 1 in less than 6 months+ |
| Growth rate | meets age standards | acceleration (more than 6 cm/year)+ |
| Breast enlargement | Yes | Yes |
| Growth forecast | within target growth limits+ | below target growth/population norm+ |
| CV>CV for more than 1 year | No | Yes |
| Uterus dimensions | not enlarged | length more than 35 mm; bulb-shaped;+ endometrial thickening |
| Ovarian sizes | diagnostically insignificant; polycystic disease | |
| Estradiol level | diagnostically insignificant | |
| Basal LH level | diagnostically insignificant | |
| LH/FSH after stimulation with LH-RH analogue | <1 | >1 |
| Increase in LH after stimulation with LH-RH analogue | 2–4 times | 8–10 times |
The material is intended for doctors: pediatricians, endocrinologists, gynecologists.
Angelika Solntseva , Associate Professor of the 1st Department of Childhood Diseases of the Belarusian State Medical University, chief freelance pediatric endocrinologist of the Ministry of Health Medical Bulletin , December 9, 2010
Share
Causes
The development of disorders is influenced by the following factors:
- irrational diet
- inactive lifestyle
- Fertility and lactation period
- certain medications
- hormonal disorders
For hormonal disorders, complex pharmacological treatment will be required. However, in the case of childbirth and poor nutrition, long-term medication is not required.
Symptoms
The main symptom of gynecomastia in women that should be considered is the unnatural growth of the mammary glands. Both girls and women should pay attention to breast asymmetry.
This pathology does not create problems after breast surgery. In this case, the disease will proceed quickly and painlessly. The main danger is the diffuse or nodular form of gynecomastia. It is characterized by the following symptoms:
- pain and discomfort in the chest area
- tissue thickening
- Any discharge from the nipple, including blood.
If these symptoms are detected, treatment should not be delayed.
Diagnostics
To make a diagnosis, the doctor must carry out a number of manipulations:
- Exploratory survey. After talking with the patient, the doctor begins to examine the woman’s mammary glands. The doctor also pays attention to such indicators as: symmetry, size, color, distortion, discharge from the nipple.
- Palpation. Palpation is carried out in 3 positions: standing, lying on your back and on your side, from the center of the gland to its edges. Please note that this procedure can be performed at home.
- X-ray fluoromammography (mammography). This examination is carried out without special contrast agents. It allows you to diagnose the initial stages of dangerous diseases. However, a mammogram alone is not enough to make a reliable diagnosis, as it can sometimes be difficult to distinguish healthy tissue from malignant lesions.
- Dictography. This is a conventional mammogram, but with the use of special contrast agents. This examination may be slightly painful due to the insertion of a needle containing a substance into the tissue.
- ULTRA-HEARING. The procedure is safe and is one of the main diagnostic methods in modern medicine. The sensitivity of this method is high.
- MRI. This examination allows for an accurate diagnosis, but due to the cost of the device, the use of this method must be justified by medical indications.
- The cytological (morphological) method is often used when a malignant neoplasm is suspected. education. This examination is virtually painless and can be performed under local anesthesia.
Treatment of mastitis in teenage girls
In the structure of purulent-inflammatory diseases of the mammary glands (MG), the proportion of non-lactation mastitis (NM) ranges from 5–45% and does not tend to decrease. NM is usually called inflammation in the breast outside the period of childbirth and lactation. The clinical picture, diagnosis and treatment of lactation mastitis in adult patients is well covered in the literature, while the tactics for managing pubertal patients with mastitis are practically not defined. Non-lactation mastitis is a complex diagnostic problem due to a blurred clinical picture and a polymorphic course that requires the use of additional diagnostic methods. In most patients with urinary tract, only a palpable formation in the breast is clinically detected, often without signs of inflammation, which requires differential diagnosis with other diseases of the breast [1–7].
Until now, there are no common views on the etiology and pathogenesis of the disease, therefore there is no single classification of NM. Existing classifications are based either on clinical data or on histological findings. There are no diagnostic criteria for various forms of UI and, as a result, unified approaches to treatment.
Treatment of mastitis in teenage girls is often carried out without taking into account the dynamics of hormonal status; as a rule, the leading methods are aggressive surgical methods of opening formations in the breast [8–13].
The question also remains relevant whether mastitis in teenage girls is only a consequence of exposure to an infectious factor on the breast, or whether mastitis is combined with manifestations of any changes in other organs of the reproductive system.
We examined 106 girls with breast diseases who were treated in the gynecological department of the Morozov Children's City Clinical Hospital over the past 5 years. Of these, 100 were diagnosed with UI.
All girls with mastitis were admitted on an emergency basis, 7 of them were admitted again, after previous treatment in the surgical departments of children's hospitals in Moscow, three of them were transferred from the surgical department to the gynecology department of the Morozov Children's City Clinical Hospital.
Upon admission, all girls complained of pain in one breast, the appearance of redness of the skin over the breast, in many cases the presence of a lump in the breast and an increase in the size of the diseased breast. Five girls were diagnosed with galactorrhea. All patients were diagnosed with NM.
According to the nature of mastitis, we divided the patients into two groups: with serous (diffuse) mastitis - 16 girls (16%) and with purulent mastitis (abscessing) - 84 girls (84%).
When analyzing the pace and nature of sexual development, girls with mastitis were divided into two subgroups: the youngest - up to 13 years old and the older - 14-17 years old. The average age of girls with serous mastitis was 13.4 ± 0.5 years. The average age of girls with purulent mastitis was 13.2 ± 0.2 years.
When studying family history, it was revealed that 12.3% of mothers, grandmothers and other relatives had breast pathology, most often it was fibrocystic mastopathy. 16% of mothers were diagnosed with various menstrual cycle disorders, in most cases such as irregular menstruation.
Chickenpox affected 42% of patients, and 6% of patients suffered from this disease approximately 1 month before the onset of mastitis. Measles, rubella, and scarlet fever were noted by us as extremely rare diseases.
Condition of the reproductive system of girls with mastitis
The growth and development of breast tissue in these patients began at 8–9 years of age, menstrual function began on average at 12–13 years of age. The average age of menarche in girls was 12.2 ± 0.3 years.
When analyzing menstrual function, we found that 27 patients did not yet have menstrual function, which is 27% of the total number of patients.
The menstrual cycle was established in only half of the patients. In most girls it lasted 24–28 days, in some up to 38–40 days, bleeding lasted from 3 to 7 days, in most it was moderate or scanty, in 8% of patients there was a history of uterine bleeding during puberty (UMB), in one girls were diagnosed with manual transmission at the time of admission for urinary incontinence. In 23 patients, menstruation was irregular.
Upon admission of patients to the department, it was revealed that sexual development corresponded to age in 91 patients. In all girls, the development of secondary sexual characteristics was assessed using the Tanner scale (table) [3, 5].
A study of the sexual development of girls showed that breast cancer began to develop in a timely manner in 93% of girls. In most patients, the degree of breast development was 2 or 3. The 1st degree of development was observed in 7 girls aged 8 to 11 years; 2nd degree of development was observed in 24 girls from 11 to 14 years old; developmental stage 2–3 was determined in four 14-year-old girls; The 3rd degree of development was observed in 29 patients, on the basis of which we can conclude that urinary incontinence develops in the developing breast, during the period of its rapid growth and development.
In 23 menstruating girls, mastitis appeared in the expected first phase of the cycle, in 30 1–12 days before menstruation, in 23 girls menstruation was irregular, so it was impossible to determine the phase of the cycle.
Mastitis clinic
All girls with mastitis, both serous and purulent, complained of pain in one breast, two - in both, which arose from 1 to 5 days before admission to the clinic. The intensity of pain is described as ranging from moderate to very severe. When examining the breast, swelling of the patient's breast, local hyperemia of the skin in the periareolar region, most often on the lateral side of the gland, measuring from 4 to 12 cm, hyperthermia of the skin and tenderness of the breast on palpation were noted. The affected breast is larger in size than the healthy one and has an unusual shape due to the pathological infiltrate, the size of which ranged from 3 to 10 cm in diameter. In the center of the infiltrate, an area of softening (abscess) was identified in 84% of patients. In 11%, enlargement and pain on palpation of the axillary lymph nodes were noted, less often (in 3%) - cervical lymph nodes. On the breast skin of 9% of girls, marks were noted from compression by the metal inserts of the bra. Discharge from the nipple (purulent or sanguineous) was observed in 5% of patients. Low-grade fever was observed in 34% of patients, body temperature ranged from 37.2 to 38.0 °C.
Purulent (abscessing) forms of mastitis predominated. Of 100 patients from 8 to 17 years 11 months 28 days, 16 patients had serous mastitis, and 84 had purulent mastitis.
Ultrasound data of the breast in girls with mastitis
Repeated ultrasounds were performed: the first - upon admission, the second - at the time of puncture, the third - before discharge. The method is free of radiation hazard and allows for multiple studies.
When performing an ultrasound of the breast in girls with mastitis, as a rule, dilatation of the ducts in the diseased breast is detected, often in the healthy one, larger or smaller in size, one or more anechoic formations, usually located in the para-areolar region. The presence of an anechoic formation is characteristic of dilatation of the breast ducts [2, 14–16].
When a suppurative process occurs against the background of diffusely changed tissues, a hypoechoic zone and hyperechoic areas of the abscess capsule (zones of purulent melting) and hyperechoic zones (areas of detritus) are determined [2, 14, 15]. The contents of the inflammatory formation may be homogeneous or contain various echo-heterogeneous inclusions. By the time abscess formation is complete, a hyperechoic capsule is clearly visible.
When performing an ultrasound of girls with purulent mastitis, a hyperechoic formation with anechoic areas in the right breast was detected in 50% of girls, in the left - in 48%, and in 2% - bilateral mastitis. In 83% of girls, one formation was found, in 17% from one to three, which was classified as multi-cavitary mastitis. In 94% of patients, the pathological focus was found in the upper or lower lateral segment, in 6% of girls - in the medial segment; as a rule, the entire pathological lesion was located para- and subareolar (Fig.).
The external genitalia of all girls were developed correctly, according to the female type. Pubic hair growth (according to the Tanner scale) corresponded to grade 1. in 27% of girls, 2nd stage. - 32%, 3rd grade. - 23%, absent in 18% of patients. During a two-manual rectoabdominal examination, the uterus was palpated in size corresponding to puberty, dense in 84%, soft in consistency in 16% of girls menstruating during the examination, mobile, painless. The areas of the ovaries upon palpation were painless in all; in three, slightly enlarged ovaries were noted.
Results of a study of sex hormones in girls with mastitis
A study of hormone secretion was carried out in 37 girls, of which 28 patients had purulent mastitis and 9 had serous mastitis. In patients with purulent mastitis, hormone secretion was examined in two age groups: MVG and SVG.
In girls with mastitis, the secretion of luteinizing hormone and follicle-stimulating hormone in both groups was slightly higher than for age. Prolactin secretion was high (above 20 ng/l) in almost half of the patients (48.6%). The secretion of estradiol in both groups was slightly lower than the age norm in most girls and only in two girls in the group of serous mastitis reached 220.0 and 417.46 pmol/ml, which indicated the presence of an ovulatory peak of estrogen in them during the examination cycle. The secretion of progesterone was especially low, averaging 0.7 ± 0.1 ng/ml and 1.7 ± 0.5, respectively, in the MVH and SVG. Only four (10.8%) girls showed an increase in progesterone to 4.48, 5.29, 10.63 and 12.67 ng/ml, which indicated the presence of an inferior corpus luteum in two patients and a normally functioning one in two patients. corpus luteum.
Thus, the content of hormones in the blood plasma, taking into account the age of the patients, the timely appearance of secondary sexual characteristics in them and the sufficient development of the breast, despite the fact that menstrual function has not yet appeared in everyone, allows us to assert that the girls with mastitis were in the period of formation of menstrual function. functions.
We believe that dilatation of the breast ducts may be associated with the influence of excess prolactin, which was noted in 48.6% of patients. Apparently, prolactin promotes the expansion of the ducts and the appearance of secretions in them even at puberty. It can be assumed that the combination of reduced levels of estrogen and progesterone and increased secretion of prolactin stimulates the secretory function of the breast, that is, lactation [4, 8, 17–22]. A similar hormonal situation, according to M.A. Tarasova and K.A. Shapovalova (2011), is observed in the early postpartum period at the beginning of lactation [19]. In girls, in the absence of outflow, the ducts expand and stagnation of discharge occurs, which can become infected with microorganisms inhabiting the skin or coming from foci of chronic infection, causing mastitis. Consequently, such mastitis, in essence, is also lactational, and it should be more logical to call it pubertal (adolescent) mastitis, rather than non-lactational.
Treatment of serous mastitis
Analyzing various methods of treating girls with mastitis and taking into account our own experience, we have developed an algorithm for the treatment of mastitis in girls. In the treatment of patients with the serous form of mastitis, we preferred the conservative method [2, 4, 23–25].
Treatment of serous forms of mastitis began with the use of mast-lifting ointment or semi-alcohol dressings, immediate administration of antibacterial agents, mainly cephalosporins and penicillin drugs of the 2nd-3rd generation and non-steroidal anti-inflammatory drugs.
The use of immunomodulators in complex therapy makes it possible to increase the effectiveness of antibacterial agents, reduce the duration of treatment (hospital stay), help restore immunity, and stop the clinical manifestations of the disease 2 times faster.
This therapy made it possible to avoid the progression of inflammation and the transition from serous to purulent form.
Patients were recommended to be monitored by an obstetrician-gynecologist and a pediatric endocrinologist.
Treatment of purulent mastitis
Analysis of treatment data showed that previously girls with purulent mastitis were treated in pediatric surgical departments [1–5, 11, 24], where the treatment method was often surgical dissection of the breast and its sectoral resection. In the gynecological department of the Morozov Children's City Clinical Hospital, the main method of treating purulent mastitis was puncture of the abscess with a thick needle, through which the contents of the abscess were evacuated for subsequent bacteriological examination. The puncture was performed under aseptic conditions in a small operating room, usually under local anesthesia (lidocaine), with a needle with a diameter of 18–22 mm and a cannula under the control of ultrasound navigation. After evacuating the contents of the abscess, its cavity was washed with an antibacterial drug, antibiotics in a volume of up to 2–3 ml were injected through a needle, and a vascular catheter was left in place. An aseptic, semi-alcoholic or ointment breast lifting bandage was applied and subsequently daily visual monitoring of the condition of the breast was carried out, and if necessary, a repeat ultrasound of the mammary glands was performed. If the abscess persisted, it was punctured again. The issue of discharge of the patient was decided only after the disappearance of the abscess, according to palpation and confirmed resorption of the abscess according to ultrasound of the mammary glands.
96% of purulent formations were punctured under the control of ultrasound navigation. Four patients were admitted on duty as an emergency, and they underwent puncture without ultrasound guidance. In three of these four girls, within 3–5 days after puncture treatment, there was no positive dynamics in reducing the heterogeneous formation, and therefore it was necessary to resort to repeated puncture, which indicates the advisability of ultrasound navigation in all cases of puncture treatment of purulent formations of the mammary gland.
During a five-year observation, we had to resort to the surgical method of opening a purulent formation only twice, which also led to a complete recovery of the patients. In all girls, the therapy led to recovery, confirmed by dynamic ultrasound of the mammary glands.
As observations have shown, the thick-needle puncture-aspiration method turned out to be the most optimal for the treatment of purulent mastitis in girls, since it meets the main requirements for the treatment of patients in pediatric gynecology - the effectiveness of the method used, safety in use, minimal trauma to the still growing breast, as well as the above method allow you to preserve the anatomy and function of the breast and achieve complete recovery, which we observed in 98% of girls.
Literature
- Abaev Yu. K., Naychuk I. I. Mastitis in childhood // Pediatrics. 2006. No. 1. P. 53–57.
- Adamyan L.V., Bogdanova E.A., Sibirskaya E.V., Sorokina I.N. Mastitis in girls (literature review) // Problems of reproduction. 2012. T. 18, no. 5. pp. 27–32.
- Bogdanova E. A. Practical gynecology of young people. M., 2011. pp. 202–211.
- Kokolina V.F., Rasskazova-Galyatkina M.V. Non-lactation mastitis in teenage girls // Reproductive health of children and adolescents. 2007. No. 3. P. 67–73.
- Okulov A. B., Adamyan L. V., Brovin D. N., Bogdanova E. A. Mammary glands and their diseases in children. M.: MIA, 2010. pp. 65–70.
- Proklova L.V. Puncture treatment of abscessing non-lactational mastitis in girls of puberty. Author's abstract. dis. ...cand. honey. Sci. St. Petersburg, 2009.
- Di Vasta AD, Weldon C., Labow BI The breast: Examination and lesions. In: Emans, Laufer, Goldstein's Pediatric & Adolescent Gynecology, 6th, Emans SJ, Laufer MR. (Eds), Lippincott Williams & Wilkins, Philadelphia, 2012. P. 405.
- Adamyan L.V., Bogdanova E.A., Sibirskaya E.V., Sorokina I.N. Development of the mammary glands in girls (literature review) // Problems of reproduction. 2012. T. 18, no. 6. pp. 20–23.
- Gurkin Yu. A. Children's and adolescent gynecology. M.: MIA, 2009. pp. 489–499.
- Pirveliev V.V. Long-term results of treatment of non-lactation mastitis in adolescence and youth. Author's abstract. dis. ...cand. honey. Sci. St. Petersburg, 2007. 18 p.
- Sokolov V.N. Non-lactation mastitis in teenage girls // Doctor's Notes. 2008, no. 9.
- Berna-Serna JD, Madriqual M., Bema-Serna JD Percutaneus management of breast abscesses. An experience of 39 cases // Ultrasound. Med. Biol. 2004. Vol. 30, No. 1. P. 1–6.
- Stricker T., Navratil F., Forster L. et al. Nonpuerperal mastitis in adolescents // J. Pediatr. 2006. Vol. 148(2). P. 278–281.
- Zabolotskaya N.V., Zabolotsky V.S. Ultrasound mammography (educational atlas). M.: 2005.
- Pykov M.I., Vatolina K.V. Pediatric ultrasound diagnostics. M.: Vidar-M, 2001. pp. 549–553.
- Gioffrè Florio MA, Famà F., Buccheri G. et al. Non-lactational mastitis: our experience // Ann. Ital. Chir. 2006. Vol. 77, No. 2. P. 127–130.
- Andreeva E. N. et al. Prolactin and mammary glands: norm and pathology // Gynecological endocrinology. 2012, vol. 14, no. 1.
- Koreyba K. A., Izmailov A. G. On the issue of the etiology of non-lactation purulent mastitis // Med. magazine 2003. No. 4. pp. 229–230.
- Tarasova M. A., Shapovalova K. A. Physiology of lactation, fertility and contraception after childbirth // Gynecology. 2011, vol. 13, no. 4. pp. 66–69.
- Elagili F. et al. Aspiration of breast abscess under ultrasound guidance: outcome obtained and factors affecting success // Asian. J. Surg. 2007. Vol. 30, no. l. P. 40–44.
- Fenton Suzanne E., Beck Lydia M., Borde Aditi R., Rayner Jennifer L. Developmental Exposure to Environmental Endocrine Disruptors and Adverse Effects on Mammary Gland Development. Endocrine Disruptors and Puberty, 2012, pp. 201–225.
- Russo J., Russo IH Development of the human breast // Maturitas. 2004. 49, 2, 15.
- Bashmakova N.V. Evaluation of the clinical effectiveness of the drug “Mastodinon” in the complex treatment of menstrual disorders in adolescents // Scientific and practical journal “Medical Department”. 2003. T. 3, no. 7. pp. 90–97.
- Lyubimov M.V. Non-lactation mastitis in adolescence and youth (clinical features, diagnosis and treatment). dis. ...cand. honey. Sci. 2002. 84 p.
- Pearlman MD, Griffin JL Benign breast disease // Obstet Gynecol. 2010 Sep; 116(3):747–758.
E. V. Sibirskaya*, 1, Doctor of Medical Sciences L. V. Adamyan*, Doctor of Medical Sciences, Professor, Academician of the Russian Academy of Sciences I. E. Koltunov**, Doctor of Medical Sciences, Professor E. A. Bogdanova*, Doctor of Medical Sciences , Professor I. N. Sorokina*, Candidate of Medical Sciences
* Federal State Budgetary Educational Institution of Higher Education MGMSU named after. A. I. Evdokimova, Ministry of Health of the Russian Federation, Moscow ** Morozovskaya State Budgetary Institution, Children's City Clinical Hospital, Moscow
1 Contact information
Treatment of mastitis in teenage girls/ E. V. Sibirskaya, L. V. Adamyan, I. E. Koltunov, E. A. Bogdanova, I. N. Sorokina
For citation: Attending physician No. 1/2018; Page numbers in the issue: 12-15
Tags: girls, mammary glands, inflammation, puncture
Treatment
Treatment depends on what caused the abnormality. If you are taking drugs, you just need to stop taking them. If this pathology is caused by obesity, then it is necessary to fight excess weight, and this means normalizing nutrition and exercise. If the pathology is caused by hormonal imbalance, surgery will be required.
Operation
Indications for surgical intervention:
- Severe chest pain and discomfort
- diffuse type of disease
- The bust is enlarged to such a size that it affects the heart muscle and other organs.
The operation is performed under general anesthesia. The operation lasts about an hour, depending on the complexity of the disease.
For symptoms of a false form of the disease during surgery to remove excess fat. From the true forms of the disease through surgery to remove excess glands. After surgery, swelling and bruising are normal and gradually disappear.
Traditional treatment does not bring results, so it is best to undergo surgery so that this pathology does not develop into oncology.
The term “gynecomastia” refers to enlargement of the mammary glands in men.
This is a fairly common condition that has no age restrictions. The presence of large breasts can cause a lot of complexes in a man, preventing an active social life.
Let's look at the reasons for the development of gynecomastia and how to treat it. This condition is not always a pathology and can develop at a certain age as a variant of the norm, when the hormonal balance is disturbed in the direction of increasing female sex hormones - estrogens.
Physiological gynecomastia in men can occur in three cases:
1. Gynecomastia of a newborn occurs in the first 2 weeks after birth, as a result of the entry of estrogens from the placenta into the boy’s body while still in the womb. After a few weeks, the mammary glands return to normal.
2. Adolescent (juvenile, pubertal) gynecomastia. This type of physiological gynecomastia develops in young men during puberty and usually goes away on its own within 2 years. Treatment is necessary when the mammary glands have not completely returned to normal. In these cases, surgeons come to the rescue.
3.Gynecomastia of old age. The cause is a decrease in the synthesis of male sex hormones (testosterone), as a result of which estrogens predominate. During this period of a man’s life, there are enough reasons for the development of pathological gynecomastia and special treatment may be required.
In all other situations, enlargement and pain in the mammary glands in men are the result of deviations from the norm, a consequence of hormonal changes. And in this case, treatment should begin with a trip to the endocrinologist.
The causes of gynecomastia may include problems such as:
— Endocrine diseases (obesity, thyrotoxicosis, pituitary adenoma, etc.).
- Liver disease.
- Kidney disease.
— Rehabilitation period after fasting.
- Use of a number of medications (estrogens, methyldopa, antidepressants, etc.).
- Tumors.
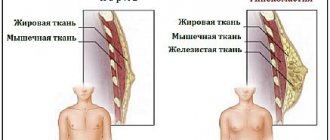
Depending on the development mechanism and the type of growing tissue, two types of this pathology are distinguished:
False gynecomastia , where the cause is general body obesity. Moreover, the gland is small in size.
True gynecomastia . It occurs as a result of the growth of the glandular tissue of the male breast against the background of the production of estrogens or various pathologies to voluminous sizes. Only hardware testing can determine it. The most accurate data on the condition of tissues is provided by the ultrasound diagnostic method .
The second type of disease is characterized by severe symptoms and requires mandatory treatment, since its prolonged manifestation will lead to irreversible complications.
Treatment of gynecomastia directly depends on its type.
If physiological gynecomastia occurs, it goes away on its own. The only recommendation for pubertal gynecomastia is to increase physical activity.
True pathological gynecomastia is treated differently depending on the cause and stage of its development; both conservative and surgical methods of therapy are used, but the issue of types and methods of treatment is decided by an endocrinologist .
If we are dealing with false gynecomastia, it does not pose a health hazard, but the psychological state of the patient suffers; in this case, a diet is prescribed, general weight loss measures are prescribed, and a minimally invasive method of surgical correction is used to eliminate the cosmetic defect, which does not require a hospital stay. – liposuction and cosmetic procedures to strengthen breast skin.
You can make an appointment with our specialists by calling and 260-27-90
DOCTORS
| Vasilyuk Anatoly Alexandrovich Urologist-andrologist, highest category Ultrasound-guided prostate biopsy treatment of erectile dysfunction - PRP therapy! | Makhno Evgenia Andreevna Endocrinologist, category 2 | ||
| Pedan Oleg Ivanovich Surgeon, plastic surgeon, certified Aptos trainer | Kondratyeva Marina Nikolaevna Doctor - endocrinologist of the highest category | ||
| Borushnova Oksana Vladimirovna Doctor – endocrinologist of the highest category, Ph.D. | Tikhonova Natalya Vladimirovna Doctor – therapist, endocrinologist. First qualification category |