What is microsclerotherapy (removal) of telangiectasia (spider veins)?
Microsclerotherapy of telangiectasia (spider veins) is a modern cosmetic procedure aimed at removing small-diameter venous vessels by introducing substances (sclerosants) specially developed for this purpose into their lumen. The technique is based on the effect of a chemical burn of the inner wall of the asterisk with subsequent fibrosis of the vessel.
Microsclerotherapy procedure for telangiectasis
The microsclerotherapy procedure for telangiectasia is the “gold standard” for the removal of these vascular formations that arise from persistent dilatation of the smallest veins. This state of affairs is associated with a high aesthetic effect, safety and good tolerability of microsclerotherapy for telangiectasia.
Operating principle
A cosmetologist uses a laser to direct a broadband pulsed light stream to problem areas, which leads to the disappearance of all destructive manifestations on the skin of the face. As a result of the directed action of the beam, the upper layer of tissue is heated, which causes activation of coagulation processes. The walls of blood vessels narrow and “stick together” under thermal influence. Blood flow decreases, and visible manifestations on the skin disappear. Vascular networks and “stars” dissolve without leaving marks on the skin.
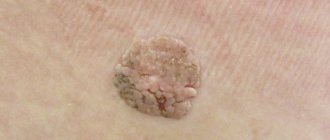
What is telangiectasia (spider veins)
Telangiectasia (spider veins) is a persistent dilation of the smallest vessels of the skin: venules, arterioles and capillaries. The dilations of the smallest arteries rarely exceed a diameter of 0.2 mm and are predominantly red in color. These are red telangiectasia. To remove them, methods based on physical influence are used: radiofrequency and laser percutaneous exposure.
Types of spider veins
The clinical significance of telangiectasia is still discussed by leading European phlebologists. However, the contribution of telangiectasia to the development of symptoms of chronic venous insufficiency is rather exaggerated. The leading clinical significance of telangiectasia is a pronounced cosmetic defect. The so-called “blue” telangiectasias are dilated venules. It is these formations that are the leading reason for turning to an aesthetic phlebologist.
Diagnostics
Nowadays, some experts consider this disease not serious, because it only carries the threat of a cosmetic defect. In addition, patients are highly prone to relapses (even after removal of the asterisk, it often appears again) and resistance to main treatment methods. But, if spider veins cause discomfort, even if only from an aesthetic point of view, this is already a good reason to seek qualified help. Also, you need to remember that in some cases the appearance of spider veins is a symptom of a more serious disease, for example, chronic vascular pathology, varicose veins, ataxia-telangiectasia, liver cirrhosis, Bloom's syndrome, which is why it is important to be properly examined and exclude the possibility of another diseases.
Diagnosing spider veins is not difficult - it is a matter of examining and interviewing the patient. But for a complete picture, it is important to find out the reason for their appearance, and whether there is a concomitant disease. A blood test, ultrasound, test for the patency of the main vessels, consultations with other specialists (cardiologist, endocrinologist, gastroenterologist) may be required.
Therefore, with the problem of spider veins, it is initially better to contact a specialist in a medical center with sufficient laboratory and diagnostic facilities.
What is the method of microsclerotherapy for telangiectasia (spider veins) based on?
The microsclerotherapy technique is based on the chemical effect of special substances (sclerosants) on the inner wall of the vessel, followed by its exclusion from the bloodstream and resorption.
Spider vein removal procedure
A very important point in this process is the absence of damaging effects on healthy venous vessels. This happens because in a normally functioning vein there is a fairly high blood flow rate and the sclerosant is quickly diluted to a concentration that does not have a damaging effect.
Why do spider veins appear?
The most common causes of spider veins are:
- kidney and liver diseases;
- arterial hypertension;
- lack of vitamin C, vitamin deficiency;
- endocrine disorders, hormonal disorders;
- metabolic disease;
- overweight;
- too frequent visits to baths, saunas and other rooms with high temperature and humidity;
- dermatological diseases;
- significant physical activity, mechanical pressure on specific areas of the body;
- pregnancy and childbirth;
Doctors believe that one of the main reasons for the appearance of spider veins is genetic predisposition. Some doctors believe that mesh occurs, among other things, due to the use of inappropriate medications and cosmetics. According to statistics, women are more likely to suffer from asterisks.
A good modern sclerosant, as it should be
A good modern sclerosant should have the following properties:
- The substance must not be toxic to the human body
- The sclerosing effect should be caused only by a strictly defined concentration of the drug, subject to prolonged contact with the vein wall
- No allergic reactions to sclerosant
- The drug must have the necessary strength to obliterate sufficiently large vessels, and be safe in case of extravasation (going beyond the boundaries of the vessel)
- The drug should not cause scarring or skin pigmentation effects
- No pain effect on drug administration
- The sclerosant must have good solubility in physiological solution.
How to treat vascular network on the face?
To combat this aesthetic problem, you can use several methods at home, as well as special care products. They help reduce the spread of redness, prevent the appearance of mesh in new places, and also significantly reduce the degree of its manifestation.
- A simple but effective method is contrast washing. Alternating cold and hot water can further strengthen the walls of blood vessels and reduce the appearance of redness. This procedure is also good as a preventive measure.
- At home, you can use special serums with an anti-rosacea effect, take vitamins with ascorutin, and also use algae face masks for vascular network.
- An effective procedure is thermolifting, which can be done in any beauty salon. With its help, it is possible to activate the body’s production of its own collagen in tissues, which has a beneficial effect on strengthening the vascular network. The skin becomes denser, and visible manifestations of rosacea become invisible. You can also lighten lesions with vascular walls using mesotherapy injections.
- For mild, unexpressed forms of manifestation, it is recommended to use special massages and anti-rosacea programs. The complex of such cosmetology programs includes anti-rosacea cryomasks, ampoules and firming massages of the face and body. The result of this procedure is the activation of blood movement and the effect on the lymph, which leads to the strengthening of blood vessels.
Types of modern sclerosants
All modern sclerosants can belong to one of the following groups:
- Detergent preparations. The chemical structure of these substances is based on fatty acids or alcohols. The mechanism of their action is based on the extraction of protein molecules from the surface membrane of the endothelial cell of venous vessels, the cell is irreversibly damaged and dies. This effect works only in the range of a certain sclerosant concentration, below which there is no effect on vascular cells. This group is represented by the following drugs:
- Ethoxysclerol (Polidocanol).
- Sodium tetradecyl sulfate (fiberwein).
Everything is ready for microsclerotherapy
In addition to these drugs, the following detergents are also used in the world: sodium morruate, ethanolamine oleate, glycerin.
- Cell toxin preparations are used by some specialists for sclerosis of vascular formations.
- Hypertonic and ionic solutions. Modern European phlebologists also use the following sclerosants of this group:
- Hypertonic sodium chloride solution (20 and 23.4% solutions).
- Sclerodex (a combination of a solution of 25% glucose and 10% sodium chloride).
- Ionized iodine preparations (variglobin, sclerodin).
- 75% glucose solution.
In Russia today only drugs from the detergent group are approved for use: polidocanol (ethoxysclerol) and tetradecyl sulfate (fiberwein). The issue of admitting 75% glucose solution into medical phlebological practice is being actively resolved.
History of sclerotherapy (microsclerotherapy) technique
The first attempts to sclerose veins probably took place in antiquity. Data about this were preserved in the most ancient written works. These works are known today as the "Hippocratic Corpus". Here, an artificially created inflammatory process in a varicose vein followed by puncture with a thorn of the “Tree of Hippocrates” (eastern plane tree) was described in fairly detailed form. The first documented experiments of injecting solutions into a vein date back to 1656. Then an English scientist from Oxford, Christopher Wren and a group of like-minded people, united around the physicist Robert Boyle, tried to experimentally study the recently presented theory of blood circulation by W. Harvey. The first documented attempt to cause obliteration of a vein by introducing acid into its lumen belongs to the Swiss doctor D. Zollikofer in 1682. An important historical milestone in the development of injection techniques was the invention of the syringe by the French doctor from Lyon C. Pravaz, who used his own invention for sclerosis of arterial aneurysms.
French doctor C. Pravaz invented the syringe
For the first time, data on the successful removal of varicose veins using sclerotherapy using iron perchlorate were presented by Debout and Cassignac in 1853. Desgrange in 1860 reported success in the treatment of varicose veins by injecting iodine and tannin into a vein. In subsequent years, scleroobliteration was used to remove varicose veins with varying degrees of success by leading doctors of the era. The development of sclerotherapy was influenced by the fundamental advances of that time in the field of surgery. The discovery of the great saphenous vein by Madelung (1844), asepsis by J. Simmelweis (1848), antiseptics by J. Lister (1867), and the development of anesthesia techniques determined the shift in the vector in the treatment of varicose veins towards open surgery. At the same time, the imperfection of sclerotherapy drugs and techniques led to a significant number of complications, sometimes fatal. These factors led to the fact that the World Congress of Surgeons, held in Lyon in 1894, gave a clearly negative assessment of the sclerotherapy method, and open vein surgery took a dominant position for many years. Work on alternative sclerosants continued in the early 20th century. A new page in the development of the technique was opened in 1911, when the French doctor Jean Sicard spoke about the successful experience of using a relatively safe solution of sodium salicylate. Later (1919, 1920) the salicylate solution was replaced by a sodium carbonate solution and founded the “French” technique of sclerotherapy. In the 1930s, a new type of sclerosing preparations, detergents, appeared. Their action is based on the denaturation of endothelial proteins of the venous wall. Further work with drugs of this type led to the appearance of sodium tetradecyl sulfate and polidocanol in the 1940-1950s. Their appearance led to the fact that the technique of sclerotherapy of veins reached a new level. These sclerosants remain relevant in the world of modern phlebology to this day. The combination of sclerosant and air was first proposed back in the 40s of the 20th century, but widespread introduction into practice took place only in the 1990s. This was facilitated by both the strengthening of the role of ultrasound scanning in phlebological practice and the introduction of the L. Tessari three-way valve technique.
L. Tessari three-way valve in a modern modification
The creation of high-quality fine foam and the use of ultrasound navigation made it possible to successfully obliterate large-diameter veins and use sclerotherapy to treat stem venous reflux. A Cochrane review published in July 2014 based on 13 randomized clinical trials showed that microfoam echo-guided sclerotherapy does not produce more recurrences than combined phlebectomy in the treatment of varicose veins. And although currently the method of microfoam echo-controlled sclerotherapy is significantly inferior in effectiveness to thermoobliteration, it is quite successfully used by leading phlebologists around the world.
Stages of microsclerotherapy
Microsclerotherapy in its modern form has become possible thanks to the advent of the finest laser-sharpened needles. These needles allow you to inject the drug into even the smallest vessels with pinpoint precision, practically without damaging the surrounding tissue.
Microsclerotherapy techniques used in the Moscow City
At the Moscow City Phlebology Center we use only the most modern types of microsclerotherapy (scleroobliteration of veins).
Sclerosants for microsclerotherapy
- Telangiectasia (spider veins), diameter up to 1 mm, are removed using a liquid form of the drug: polidocanol (0.25 - 0.75%), tetradecyl sulfate (0.1 - 0.2%).
- To remove venulectasias (diameter 1-2 mm) and reticular veins (2-4 mm), both microsclerotherapy solution and microfoam sclerotherapy (foam-form) are used. Concentration of active substance: polidocanol - 0.5-1%, sodium tetradecyl sulfate - 0.25-0.4%.
Cuperosis and enlarged veins on the face: what can and cannot be done?
First, let's look at the types of veins that can appear on the face. The most common ones include:
- Dilated veins of the paraorbital region: veins around the eyes (usually located at the lower and outer edge of the eye), temporal veins (formed in the temple area, sometimes involving the frontal part of the face, and then the scalp). Most often, the diameter of such veins is from 0.5 mm to 4 mm.
- Separate single vessels, telangiectasia - small veins with a diameter of less than 1 mm of blue, purple and pink color, localized in the face, wings of the nose, above the upper lip, and chin.
- Cuperosis is an accumulation of dilated vascular networks in the cheeks, cheekbones, and less commonly in other areas - neck, décolleté, etc.
The first two variants of veins (paraorbital, temporal, individual telangiectasia) in most cases are only an aesthetic feature not associated with any significant pathology. The patient is allowed to play sports, fly on an airplane, sunbathe and swim. Even if a trip to the south provokes a couple of new blood vessels, the situation will still not be critical. With such veins, you can live an ordinary life without committing yourself to any noticeable restrictions.
The paraorbital and temporal veins may increase in size during intense exercise. This phenomenon is a consequence of increased blood flow. After training, it completely disappears, the veins return to their previous size.
As for rosacea, it is important to understand the reason for the appearance of pronounced blood vessels on the face. For example, exposure to temperature factors (cold or heat) can aggravate the situation. Therefore, long periods of snowboarding and skiing, frequent trips to the sauna, solarium and prolonged sun exposure should be limited. The same goes for alcohol and nicotine - they affect vascular tone, which also manifests itself on the face.
The answer to the question “is it possible to play sports with rosacea” will also be positive. In moderate volumes (not in hot or frosty weather), physical activity gives only a short-term rush of blood and a temporary increase in the vascular pattern on the face. Accordingly, after playing sports everything becomes the same as before.
The choice of cosmetic procedures for this pathology also has its own characteristics. For example, peeling for rosacea is allowed, mainly superficial (enzymatic). It is recommended to select a cream for rosacea together with a cosmetologist. It is also important to remember that any active massage for rosacea is not indicated, as it can cause deterioration.
If the appearance of blood vessels on the face is caused by any serious disease (for example, systemic lupus erythematosus, SLE), then the restrictions become stricter. Patients should avoid prolonged exposure to the sun (photosensitization is possible). The sports program must be coordinated with the attending physician - rheumatologist, cardiologist or other specialized specialist.
SLE can affect various organs and systems, therefore, the limiting factors for playing sports are no longer the vessels on the face, but pathologies of the joints, heart, etc. More detailed information about all restrictions can be obtained after a thorough history taking at a face-to-face consultation with a doctor.
Indications for spider vein removal in Moscow
The microsclerotherapy procedure in the presence of telangiectatic disease and reticular varicose veins in leading European clinics is carried out for cosmetic reasons. Often, when a large number of small vessels are removed, patients note an improvement not only in self-esteem, but also in sensations in the leg area. This is due to the elimination of the pathological venous bed and the elimination of symptoms of venous stagnation. Good phlebological practice involves diagnosing the venous system before starting microsclerotherapy procedures. Often, dilation of the smallest vessels is associated with disruption of the valve apparatus of the main saphenous veins, even without the formation of visible varicose veins. According to the standards of European phlebology clinics, such diagnostics are carried out for all patients, even if the complaints consist only of the presence of telangiectasis.
Symptoms
It is unnecessary to write about the symptoms of the disease, because its manifestation usually does not raise questions - small vessels become visible to the naked eye. They may be red or blue, or change color from red to blue due to the appearance of venous blood in the vessel; may bulge on the surface or not be palpable. They are most often localized on the lower extremities, sometimes occupying a significant area, differing in the shape of the pattern (tree-like, spot-like, stellate, linear). There are stars not only on the legs, but also on the face (especially on the wings of the nose and cheeks), and on the hands.
Sometimes the stars go away on their own without any treatment. For example, if they appeared during pregnancy, then after the birth of the child they will most likely go away on their own. A similar effect can occur when hormonal treatment is stopped, which caused the asterisks to form.
Some people prefer not to pay attention to the appearance of telangiectasias, leveling out their cosmetic defect with clothing or cosmetics. Indeed, in themselves they do not pose a threat to the body. The attitude towards these formations from an aesthetic point of view is completely at the discretion of the person, but we must not forget that telangiectasia can be either a symptom or a harbinger of a more serious disease. Therefore, it is better to consult a doctor and get examined.
Contraindications to microsclerotherapy
The microsclerotherapy procedure for telangiectasia is an innovative, fairly safe, planned procedure. But, as with absolutely any invasive technique, it has contraindications:
- Skin diseases in the area of intervention of an inflammatory and infectious nature.
- Acute period of deep or superficial vein thrombosis.
- Pregnancy and lactation period.
- Allergic reaction to sclerosant.
- Presence of thrombophilia (hypercoagulable state).
- Impaired motor activity of the patient.
- The presence of an open oval window of the heart (for the use of a foam form of the drug).
- Lymphostasis.
Adequate compression after the procedure significantly improves the aesthetic result. Therefore, aesthetic microsclerotherapy in patients for whom compression therapy is contraindicated is not contraindicated, but has its own nuances.
In the presence of morbid obesity, as a rule, a larger number of microsclerotherapy sessions are required and difficulties in selecting compression stockings are required. During long flights and hormonal therapy, it is better to refrain from aesthetic procedures and perform it later.
Technical aspects of microsclerotherapy for spider veins
The principles of microsclerotherapy for stars in the innovation center of Moscow fully comply with the best European standards. Here are some of them:
- First, blood reflux is eliminated in the proximal parts of the venous bed.
- Larger veins undergo scleroobliteration first.
- It is necessary to minimize the number of injections, preferably removing interconnected veins from one puncture.
- It is very important to ensure adequate compression. Therefore, immediately after the procedure, the patient is dressed in modern high-quality compression stockings and a half-hour walk is recommended.
How is the microsclerotherapy procedure performed in a modern phlebological center in Moscow?
In our phlebological center, we use some of the best thinnest needles with laser sharpening of 27-30 G. Using these tools, skin punctures are made that are practically not felt by patients. The procedure is performed by an experienced phlebologist, who has not only thousands of procedures under his belt, but also a significant number of master classes on this technology.
Master class performed by phlebologist Semenov A.Yu. on microsclerotherapy
Sessions are carried out with the patient in a horizontal position. After puncturing the skin, the tip of the needle enters the vessel, the specialist slowly and carefully injects the drug, making sure that the vein does not overstretch and rupture.
After the session, sterile bandages are applied and compression stockings are put on. The patient is recommended to take a half-hour walk.
Cryosclerotherapy using VeinViewer
This technology is currently used only in our clinics. The peculiarity of this microsclerotherapy technique is to identify the supplying veins using a special thermal imager. For an experienced phlebologist, this picture allows one to accurately differentiate intradermal vessels. Before injection of sclerosant, the skin is cooled with cold air with a temperature of 30ºC. This ensures complete painlessness of the injection and reduces the skin reaction - there is no redness, inflammation or large bruises.
Complications and side effects after a microsclerotherapy session
Minor ecchymosis (bruising) at the injection sites after the procedure is almost all that worries patients. These phenomena disappear within 1-2 weeks. Complications and side effects of sclerotherapy are quite rare, but you still need to know about them:
- Skin hyperpigmentation is a fairly rare phenomenon and goes away on its own within 6-12 months.
- Local tissue swelling. It resolves on its own and does not require separate treatment.
- Neurological complications: migraine-like headache, temporary impairment of visual fields, extremely rare complications that arise when working with the foam form of sclerosant in patients with congenital heart disease (patent foramen ovale). These phenomena disappear on their own within 10-15 minutes.
- Metting is the appearance of the finest red telangiectasia in the injection area. These manifestations disappear within a few months.
- Skin necrosis occurs when sclerosant enters the perivascular tissue in high concentrations. This is a very rare occurrence and is most often associated with improper manipulation technique.
- Allergic reactions to the drug. Modern sclerosants rarely cause sensitization of the body, but you should always remember this phenomenon.
Microsclerotherapy Foam-Form (micropoam)
This procedure is used to eliminate blue telangiectasias. The foam is obtained by mixing the sclerosing agent and air in one syringe using a three-way stopcock. Initially, injections of the foam form of sclerosant are carried out into the “feeding” reticular veins, after which most of the small veins and meshes on the lower limb disappear. After some time, the remaining intradermal vessels are sclerosed with additional foam or liquid. Elimination of telangiectasis must be carried out after elimination of varicose veins in the basin of the great and small saphenous veins, since otherwise the effect of microsclerotherapy will not be achieved.
Cosmetic microsclerotherapy (microscleroobliteration) at the Moscow Phlebology Center
The microsclerotherapy method is deservedly called the “gold standard” for the removal of telangiectasia. Due to its minimal invasiveness, good patient tolerance and good clinical effect, the microsclerotherapy technique has taken its rightful place in modern phlebological practice. Cosmetic microsclerotherapy at the Moscow City Phlebological Center is performed by some of the best phlebologists in Moscow and Russia according to the most modern European standards.
Microsclerotherapy performed by phlebologist of the MIFC Raskin V.V.
We use the most advanced technologies to achieve not only a good clinical effect, but also the best aesthetic result.
Microclerotherapy (removal) of stars in Moscow - price for procedures
At our center in Moscow, the price for the microsclerotherapy procedure is strictly fixed, and therefore, when contacting our clinic, patients can count on high-quality service, treatment and an affordable cost. And remember that timely consultation with a doctor will completely cure the disease and avoid its recurrence.
| Service | Treatment category | Price |
| Sclerotherapy (microsclerotherapy) on one lower limb (one session) | Reticular varicose veins and spider veins | 8000₽ |
| Postoperative sclerotherapy (microsclerotherapy) on one lower limb (one session) | Reticular varicose veins and spider veins | 4000₽ 8000₽ |
| Sclerotherapy (microsclerotherapy) on one lower limb (course of treatment) | Does not depend on the number of sessions | 35000₽ |
| Removal of unaesthetic veins on one arm (one session) | 10000₽ | |
| Laser removal of spider veins on one lower limb (one session) | 10000₽ |
For the convenience of our patients, we work with banks that offer credit lines. Also in our center there is a flexible system of discounts and installments. Payment by Visa and Mastercard is possible. At the end of the course of treatment, the patient is given a package of documents to submit to the tax office for tax deduction.
How is the laser removal procedure for spider veins and spider veins performed?
The procedure for laser removal of telangiectasia occurs according to the traditional algorithm:
- Skin cleansing and makeup removal;
- Application anesthesia (optional), achieved by uniformly distributing lidocaine spray or Emla cream over the skin surface and then covering it with a film for 15-20 minutes;
- Setting up equipment to suit individual needs and tasks;
- Application of a conductor gel to the skin, optimizing the penetration of light energy into the tissue;
- Laser treatment with selected attachment.
The key condition for fixing and prolonging the result is the advisory support of a doctor. Remember that if you are prone to telangiectasias, they may appear again (in the same or a different place) if you ignore the recommendations for skin care and lifestyle, or the doctor does not instruct you on this topic.
The main advantage of laser removal of blood vessels is the guaranteed onset of effect even with extensive lesions. Trust your doctor in choosing the tactics and sequence to combat the defect, and your expectations will be met.
Results of microsclerotherapy for telangiectasis. Photos before and after spider vein removal
The result of treating a patient at the MIFC phlebology clinic using microsclerotherapy (removal) of spider veins
Photos before and after removal of spider veins on the left thigh
Result of spider vein removal on the right lower limb
Result of spider vein removal 1 month after microsclerotherapy
Video result of spider vein removal in our patient on both lower extremities
Questions from patients about the procedure of microsclerotherapy (removal) of spider veins
How much does modern microsclerotherapy for spider veins cost in Moscow?
A session of modern microsclerotherapy for spider veins in our Moscow city center costs 8 thousand rubles. You can find out more detailed information about the cost of treatment by phone or on our website page:.
Where is the best place to do microsclerotherapy for spider veins in Moscow?
Microsclerotherapy of spider veins in Moscow is best performed in a good city phlebology center, where they work according to modern European standards.
Is microsclerotherapy for telangiectasia and reticular veins performed simultaneously in Moscow?
Simultaneous microsclerotherapy sessions for telangiectasia and reticular veins are performed in the best Moscow clinics. This is a good procedure for quickly eliminating unsightly venous vessels.
Where can I read reviews about microsclerotherapy for spider veins and reticular veins?
Reviews from patients about microsclerotherapy for spider veins and reticular veins at the city phlebological center can be read on our website page: .