Consequences of vacuum abortion
The consequences of a vacuum abortion for the female body are minimal in comparison with other methods of terminating a pregnancy.
This method allows you to get rid of an unwanted pregnancy with minimal damage to the body. But still, like any intervention in the body, vacuum abortion does not always go smoothly. The most common consequences of a vacuum abortion are incomplete termination of pregnancy and the need to repeat the abortion using the classical method - the curettage method.
How to Prepare for Vacuum Aspiration
Removing a fetus using a vacuum syringe is as serious a procedure as any surgical intervention.
Therefore, preparation must be taken with full responsibility. The gynecologist will definitely refer the woman to studies such as:
- general blood test, general urinalysis;
- coagulogram;
- establishing accurate information about blood group and rhesus;
- blood for syphilis, HIV, gonorrhea, hepatitis, and other internal infections.
The gynecologist will also examine the patient in a gynecological chair, take smears from the vagina and cervix for microbiological examination and culture. An electrocardiogram may be required, as well as a thyroid hormone test.
This should be done for those who have problems with the heart or endocrine system.
The woman should also visit an ultrasound diagnostic room, where a specialist will verify the presence of pregnancy, set the exact timing, and make sure that there are no inflammatory processes in the pelvic organs or ectopic pregnancy. It is also important to determine the site of attachment of the fetus. All studies are aimed at excluding possible pathologies and contraindications.
On the day of surgery, you should take a light breakfast, do not pass it on. We need to take care of the way back home. If a woman is prone to fainting, she may need to arrange for someone to meet her and accompany her home.
It is also worth taking mental preparation seriously. Termination of pregnancy, as a rule. accompanied by the woman's mental suffering. Therefore, it is necessary to weigh everything and make a decision. And if this decision is final, tune in to a successful outcome.
Vacuum aspiration after medical abortion
Medical abortion and vacuum aspiration are minimally invasive methods of terminating pregnancy. However, the medicinal version is more effective for up to 4 weeks, and the vacuum version is more effective for up to 5 weeks.
In approximately 3% of cases, pharmaceutical abortion ends unsuccessfully - the fertilized egg remains inside. In this case, in order not to injure the uterus with surgical instruments, vacuum aspiration is used.
This must be done because the fetus exposed to abortifacient drugs is damaged. There is a high risk that the child will be born very sick and even non-viable.
If time permits, then vacuum cleaning is the best way out, especially for nulliparous women. Vacuum aspiration in this case also, as a rule, preserves the woman’s ability to become a mother in the future. Restoring health after it occurs faster than after a surgical abortion.
Diagnosis of diseases using vacuum aspiration
Some diseases require analysis of a fragment of the endometrium of the uterus. For example, if endometrial hyperplasia is suspected, it is necessary to obtain material for analysis. Since mechanical intervention in the uterus is very traumatic, in this case a vacuum is used. This procedure is called aspiration biopsy. Through vacuum aspiration, the doctor obtains a fragment of the endometrium, while the operation itself does not require anesthesia for the patient; local anesthesia with a lidocaine solution is often sufficient, as well as taking conventional antispasmodics.
In our clinic, patients can receive vacuum aspiration services using the latest modern devices. Competent doctors provide a full range of services, from vacuum abortion to aspiration biopsy. Only here women can be sure that the medical services provided are performed at the highest level.
What tests need to be taken before the procedure?
The vacuum termination procedure involves preparatory measures, which necessarily include a visit to the gynecologist and testing. Let's explain why.
When giving a referral for an abortion, the doctor must be sure that the pregnancy really exists and is not ectopic. Since during a vacuum abortion, the embryo is detached from the walls of the uterus and subsequently absorbed into the catheter tube, it is important to follow the recommended timing for such an operation.
The fact is that at a period of 4-6 weeks, the connections between the fetus and the walls of the uterus are not yet very strong, and the egg is easily separated from the walls of the uterus and absorbed into the catheter. In the 7th week and later, this will be much more difficult, so the risk that part of the egg will remain in the uterus increases. It is no coincidence that when the time is prolonged, the doctor resorts to using a curette.
Vacuum abortion is not very good for a fetus up to 3 weeks - a small embryo is difficult to absorb, and during this period the medical method of terminating pregnancy works well. Therefore, when writing a referral for vacuum aspiration, the doctor will definitely prescribe a number of procedures.
Before vacuum aspiration, to clarify the diagnosis, gestational age and position of the uterus in the pelvis, a gynecologist is examined and a vaginal ultrasound is prescribed. The woman gives:
- general analysis of urine and blood;
- blood for clotting, group, Rh factor;
- hCG tests to more accurately determine the duration of pregnancy;
- tests for HIV, hepatitis B and C.
Since a mini-abortion has a number of contraindications (any viral and infectious diseases, including those of the reproductive system), the woman will also have to undergo a smear test. This is done in the interests of the patient herself: any virus that enters the uterus during aspiration can provoke serious inflammatory processes and complications. If necessary, the gynecologist prescribes additional examinations or a consultation with another doctor (therapist, surgeon).
Preparing for a mini-abortion
When performing aspiration under general anesthesia, you should not eat food 8 hours before the intervention. Intimate relationships should be avoided 3 days before the procedure.
Otherwise, the preparation is the same as for an appointment with a gynecologist. Gynecologist appointment
Women often ask what can replace a vacuum abortion; an alternative to vacuum aspiration is medical abortion. Medical abortion - termination of pregnancy without serious consequences?
Why is vacuum aspiration dangerous?
The vacuum method of abortion is one of the most reliable and gentle. However, there is no safe abortion. And this method is fraught with a number of complications. The dangers are:
- disruption of hormonal levels, leading to serious consequences in the form of weight changes, tumor formation, metabolic disorders, and so on;
- psychological trauma that risks developing into depression;
- intrauterine bleeding;
- pain in the lower abdomen;
- inflammatory processes in the pelvic organs;
- incomplete abortion, when particles of the fertilized egg remain;
- menstrual disorder;
- infection;
- air embolism, when air enters the blood vessels and the woman dies (this is extremely rare);
- perforation of the uterine wall while measuring its depth with a probe;
- damage to the cervix with the need for suturing;
- Infertility is a rare complication, but can also occur due to improperly performed surgery.
Complications can occur early, that is, immediately after surgery. And also late - they are revealed months later in the form of hormonal problems, disruption of the menstrual cycle, and infertility.
Prevention of complications after vacuum aspiration
Even if the operation was successful, safety precautions should be followed to avoid complications. What is being done for this:
- after the procedure, the woman lies on her stomach for about 30 minutes in the presence and under the supervision of medical workers;
- if everything is in order, the woman can go home, but remember the restrictions;
- in the first 4 weeks you should not have sex, as this can lead to infection and bleeding;
- You should not take baths, saunas, or get too cold;
- visiting open and closed bodies of water is prohibited for a month;
- you cannot lift weights;
- It is contraindicated to use tampons in the first month after surgery;
- You should be careful and serious about genital hygiene, wash them with warm water, possibly with baby soap.
To prevent infectious inflammation. The doctor may prescribe antibiotics and antifungal medications. Taking special herbal teas will be useful. Their choice should be discussed with a gynecologist.
As a rule, oral contraceptives are prescribed in the first months, which will protect against re-conception, which is dangerous in the first 6 months after an abortion. These contraceptives will also help restore hormonal levels.
After 2 weeks, you should visit the gynecologist again to do a control ultrasound and make sure. that everything went well, there was no inflammation or bleeding. Fusion of the walls of the uterus.
What you should be wary of in the first days after an abortion:
- absence of discharge or very scanty bleeding (this may indicate cervical spasm);
- discharge in the form of blood clots for more than 3-4 days (possible intrauterine bleeding);
- excessive bleeding for several days after the abortion;
- purulent vaginal discharge;
- increased body temperature;
- nagging, aching pain in the lower abdomen.
After termination of pregnancy, a woman is required to be more attentive to her health and promptly seek medical help for any suspicious manifestations.
Bloody discharge after cleaning the uterus
If a woman has undergone a surgical abortion, almost in the very first days of the rehabilitation period she may experience bleeding. In their type, they will in many ways resemble menstruation, but in fact they are not menstruation. Thus, when terminating a pregnancy using instrumental methods, in absolutely all cases, damage to the uterine mucosa occurs, which leads to bleeding of the tissue.
Bloody discharge is a standard and predictable reaction of the body to such surgical interventions. The discharge usually lasts for about seven to ten days. Their amount can vary from slight dark brown spotting to intense discharge with clots. If they are released too actively, and four large pads are filled in 2 hours, urgently contact a doctor, who, after examination, will prescribe the optimal treatment.
To ensure that the discharge complies with established standards, it is recommended to protect yourself from too much physical activity. Doctors also advise not to start having sex too early after an abortion.
Pregnancy after vacuum aspiration
Many women are concerned about the issue of future pregnancy: when it is possible to afford to become pregnant again and how quickly conception can occur.
It all depends on the individual characteristics of the woman’s body and on the correct operation to terminate the pregnancy.
Reconception may not occur for some time due to:
- hormonal disorders;
- pathologies in the endocrine system;
- due to inflammation in the pelvic organs, the formation of adhesions that impede the advancement of the egg, disruption of the patency of the fallopian tubes;
- due to trauma to the cervix and its inability to hold the fetus (risk of miscarriage).
After any type of abortion, even such a gentle one as vacuum aspiration, you should plan for a future pregnancy. A consultation with a gynecologist will be required. If you become pregnant without a preliminary examination, there is a high probability of miscarriage, missed abortion, or the birth of a child with health pathologies.
In the first six months, at least 3 months, repeated pregnancy is not recommended.
| Termination of pregnancy in early and late stages | Reception is strictly by appointment, make an appointment by phone: +7 | Prices for services | Reviews about the clinic |
Why are periods late?
Even after a properly performed abortion, the menstrual cycle may be delayed and begin at a relatively late time. In particular, this may be caused by the slow rate of healing of the lining of the uterus. In order for its recovery to occur as quickly as possible, it is recommended to strictly follow all the instructions of your treating gynecologist.
If you have problems restoring your menstrual cycle after an abortion, this is a reason to seek qualified help from a doctor. Remember that the body is under stress and only an experienced and highly qualified doctor can rehabilitate it.
Click here to add your review
Ultrasound after vacuum aspiration
After any method of abortion, it is recommended to undergo an ultrasound to ensure a successful result.
A vacuum mini-abortion is performed under the control of an ultrasound machine. But even in this case, after two weeks you need to do a repeat ultrasound examination.
This is done to ensure that:
- the entire fertilized egg has been removed;
- there is no internal bleeding and no delay in the removal of blood to the outside;
- no inflammatory processes, formation of polyps;
- the epidermis at the site of fetal separation heals well.
If the operation was performed without the control of an ultrasound machine, then an ultrasound examination is prescribed 2-3 days after the vacuum abortion.
A pelvic ultrasound after an abortion also gives an idea of the health of the organs in this area.
What anesthesia is used for vacuum aspiration?
Vacuum cleaning, although a minimally invasive procedure, still requires anesthesia, as it involves pain. The anesthetic agents in our clinic are modern, more gentle and do not cause allergic reactions.
What types of anesthesia are there:
- Local anesthesia is most often used. It completely removes pain, but the woman is conscious, understands what is happening, and answers questions.
- The half-sleep method is also used, when an anesthetic drug is injected intravenously, reducing the ability to perceive reality. In this case, the woman is almost in a sleeping position, does not understand what is happening to her, does not feel pain, but can hear distant sounds. She breathes on her own and quickly recovers from anesthesia.
- At the woman's request, general anesthesia can be used. It requires an equipped operating room and the presence of an anesthesiologist. The woman is completely asleep, the artificial respiration machine supports vital systems. The woman doesn’t remember anything, but wakes up in the ward.
There are many drugs for anesthesia. The doctor chooses the one that is safest for a particular woman, taking into account her physiology and health status.
Which doctor performs vacuum aspiration?
Vacuum cleaning is performed by a gynecologist. It is within his competence to establish pregnancy, determine indications and contraindications for any type of abortion, and help to rehabilitate after an artificial termination of pregnancy. He also performs abortions provided he has completed additional training.
Our clinic employs a gynecologist who has certificates for all types of services. He has gained extensive experience and an impeccable reputation.
Rehabilitation of women after late induced abortion with congenital malformations of the fetus
Abortions lead to both early complications and long-term consequences - numerous complications of pregnancy, childbirth, and the formation of a number of gynecological diseases. Minimizing the risk of possible complications from medical abortions is extremely important. Such circumstances force scientists to look for ways to alternatively improve abortion technologies and ways to prevent possible complications [1, 2]. At the same time, regulatory documents do not sufficiently cover the issues of rehabilitation of women after a medical abortion, especially after termination of pregnancy in the second trimester.
Complications after an abortion are divided into: early (immediately during surgery - bleeding and perforation of the uterus); delayed (within one month after surgery - hematoma, endometritis, remnants of the fertilized egg, progression of pregnancy, inflammatory diseases of the uterus and appendages or exacerbation of a chronic inflammatory process, menstrual irregularities); remote (damage and scar changes in the internal pharynx and cervical canal, damage and degeneration of the endometrium, formation of synechiae in the uterus, disruption of the patency of the fallopian tubes, dysfunction of the hypothalamic-pituitary-ovarian system (HPO), psychogenic disorders) [2].
In recent years, numerous studies have been conducted to develop various safe abortion technologies aimed at reducing the risk of these complications. Vacuum aspiration of the fetal egg is widely used in the early stages of pregnancy (mini-abortion), which is considered less traumatic compared to instrumental curettage of the walls of the uterine cavity, but is still a surgical intervention. One of the modern methods is medical termination of pregnancy in early and late stages by using prostaglandins in combination with antiprogestins [3–5]. Mifepristone is a synthetic steroid drug that is a competitive inhibitor of progesterone. By binding to progesterone receptors, mifepristone blocks the action of progesterone. In this case, the sensitivity of the myometrium to oxytocin is restored, the action of prostaglandins is potentiated, which enhances the contractile activity of the myometrium [6].
Undoubtedly, surgical abortion is more traumatic, as evidenced by the presence in histological preparations of fragments of the transition zone of the endometrium into the myometrium and the myometrial tissue itself. In addition to the functional layer of the endometrial glands, the cambial glands are also removed, and the adjacent layers of the myometrium or uteroplacental region are injured [7]. The relative risk of complications is certainly higher in the second trimester, but the absolute risk is small when termination of pregnancy is performed (in the case of surgical abortion) or observed (in the case of medical abortion) by qualified health professionals [8]. From year to year, the quality of medical care for abortion of different stages is improving. Thus, in accordance with Order of the Ministry of Health of the Russian Federation 572-n [9], pregnant women undergo artificial termination of pregnancy, depending on the duration of pregnancy, indications and contraindications, using medication based on the informed voluntary consent of the woman. A clinical protocol “Medical termination of pregnancy in the first trimester” has also been developed [10].
In general, medical abortion is considered by international experts as a significant reserve in reducing maternal mortality due to termination of pregnancy at all stages. The World Health Organization (WHO) recommends that every effort be made to replace curettage with vacuum aspiration and medication to make abortion safer. Monitoring the emptying of the uterine cavity is carried out by visualizing the removed tissues [9].
However, no matter how gentle the method of termination of pregnancy, it is still a serious psychological and physical trauma, hormonal stress and always poses a risk of serious complications, including menstrual and reproductive dysfunction [7]. Studies of sufficient statistical power are still needed to compare currently used medical and surgical methods of abortion for second-trimester pregnancy termination. However, preliminary clinical experience of late pregnancy termination using modern methods in Russian research institutions within the framework of scientific programs, as well as the practical experience of a number of medical institutions in the regions according to protocols approved by local governments, demonstrates the promise of these methods for reducing complications and maternal mortality among women forced to terminate a pregnancy beyond 12 weeks [8, 11].
Recently, the role of rehabilitation in practical medicine has become increasingly important. Rehabilitation is a complex of medical, psychological, social and professional measures aimed at the most complete restoration of health, impaired functions, psychological status and performance of people who have lost these abilities as a result of injury, illness, abortion, etc. The basic principles of rehabilitation include: early implementation, complexity, stages, continuity and consistency, individual program, emphasis on the social orientation of events, monitoring of effectiveness [12]. Post-abortion rehabilitation involves a set of measures aimed primarily at restoring reproductive health.
Antibacterial drugs (ABDs) are an important and often the main component of complex prevention and therapy in obstetric practice; their rational and justified use in most cases determines the effectiveness of the treatment and favorable obstetric outcomes [13]. Microbial contamination of the surgical wound is inevitable even if all the rules of asepsis and antisepsis are perfectly observed. During the completion of the operation, the wound surface is 80–90% contaminated with a variety of microflora (usually staphylococcal). Almost all microorganisms that are present in the vagina (with the exception of lactobacilli and bifidobacteria) can cause an inflammatory process [12]. Routine administration of antibiotics during abortion reduces the risk of infectious complications after termination of pregnancy [14, 15].
Antibiotic prophylaxis is the use of antimicrobial agents in patients without clinical and laboratory signs of infection to prevent its development, as well as in the presence of signs of microbial contamination, when the primary treatment method is either to prevent an infection caused by exogenous microorganisms, or to prevent exacerbation, relapse or generalization of a latent infection [12, 16]. The purpose of modern antibiotic prophylaxis is to create the required concentration of the drug in tissues from the moment of possible microbial contamination and maintain this level throughout the entire operation and for more than 3-4 hours after. Some researchers believe that the introduction of ABP after abortion does not prevent the development of infection and is irrational; in addition, resistance, adverse drug reactions and additional costs may occur [16].
The use of antibacterial drugs for preventive purposes must be justified, and the indications for their use must be differentiated and balanced. A drug for the prevention of inflammatory complications must have: a wide spectrum of action against pathogens, in particular aerobic bacteria (mainly gram-negative), anaerobic; have good pharmacokinetic parameters, high bioavailability, a fairly long half-life, since the essence is to achieve the required concentration of the drug in the tissues before their possible microbial contamination and maintain the level throughout the entire operation and several hours after it; have proven safety and a low likelihood of side effects; minimally interact with other drugs, in particular with anesthetics and analgesics [12, 16].
The advantages of local ABP for sanitation include: absence or minimal systemic effect on the body (minimal risk of side effects); direct contact of the active substance with the pathogen; high concentration at the site of inflammation, which reduces the risk of developing resistance; rapid elimination of symptoms of the disease, including due to the foundation. Some authors [17] recommend the use of antiseptic vaginal suppositories for 5–10 days and intrauterine administration of instillagel during post-abortion rehabilitation. Other researchers propose a two-stage treatment regimen for bacterial vaginal infections in the pre- and postoperative management of patients undergoing artificial termination of pregnancy, while establishing the effectiveness of a broad-spectrum drug (dequalinium chloride) in the first stage of therapy and the need to use a drug containing lactobacilli and estriol to restore the vaginal biocenosis in post-abortion period [18].
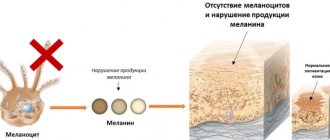
The occurrence of HPA axis dysfunction due to abortion can be explained by comparing pregnancy termination to a “hormonal shock”, which sometimes leads to catastrophic destruction of the endocrine system. It has been established that changes in the endocrine system resulting from termination of pregnancy lead to menstrual dysfunction, which contribute to the development of gynecological diseases and create conditions for the formation of metabolic syndrome. Complications associated with menstrual dysfunction develop gradually, and are often not associated with previous abortions due to their late clinical signs [16]. In addition, after repeated abortions, 3–4% of women experience inflammatory complications, 25–30% have menstrual dysfunction, more often with insufficiency of the 2nd phase of the cycle, relative hyperestrogenia, and in some women, with anovulation. Following progesterone deficiency, proliferative processes develop in the reproductive system - endometriosis, uterine fibroids, endometrial hyperplasia, recurrent polyps, adenomyosis, hyperthecosis, tecomatosis and polycystic ovaries, mastopathy. Post-stress changes occur in the endocrine system after an abortion. Increased production of corticoid hormones, estrogens, follicle-stimulating, adrenocorticotropic hormones [2, 19]. Of course, complications can be associated not only with abortion, but also with other reasons - genetic, environmental, environmental and others, but in these cases, against a complicated background, abortion causes even more irreparable harm [2, 12, 19].
Recently, experience has been gained in the use of combined oral contraceptives (COCs) for the purpose of post-abortion rehabilitation [19, 20]. Hormonal therapy to restore the endometrium and its secretory function after abortion is a mandatory component of rehabilitation [20]. The authors recommend monophasic oral contraceptives containing modern progestogens and low doses of estrogens (0.15 mg desogestrel and 0.03 mg ethinyl estradiol) [19]. Others believe that the prescription of contraceptives with dienogest is justified by the fact that artificial termination of pregnancy increases the risk of proliferative diseases, primarily endometriosis [21]. There are certain rules for the use of COCs after an abortion: start of use - 1st day after surgery; composition - low-dose monophasic COCs; dosage regimen: 21 + 7-day break or 24 + 4; duration: at least 3 months; after 3 months, the question of the advisability and duration of further use of this COC will be decided [17, 22].
In the early period after abortion, the use of COCs provides: reduction in the severity (elimination) of bleeding; inhibition of proliferative processes; anti-inflammatory and regenerative effect at the endometrial level; decreased excitability of the GGJ and decreased gonadotropic activity; elimination of estrogen and progestin deficiency; and finally, contraception. However, there are contraindications to the use of COCs in women who do not want to take the estrogen component. For this group of women, “purely progestogen” hormonal contraceptives may be recommended [12].
Insertion of an intrauterine device (IUD) immediately after abortion as part of a rehabilitation program is a good and safe method of contraception with minimal risk of expulsion and a high level of protection against recurrent abortions in the future [3]. An IUD can be installed immediately after medical or surgical abortion performed at all stages of pregnancy [9]. Other authors believe that an IUD can be inserted immediately after an abortion performed only in the first trimester of pregnancy, but if the abortion is performed in the second trimester, it is better to wait until the uterus involution occurs [6].
The best period for the onset of a subsequent pregnancy after the loss of a previous pregnancy is considered to be the first 6 months [23]. Compared with later onset of pregnancy, the incidence of recurrent miscarriage, ectopic pregnancy, preterm birth, low birth weight, cesarean section and induced labor is reduced. A recent analysis of 677 pregnancies following pregnancy loss found no association of adverse outcomes with an even shorter interval of 3 months. The data obtained do not support traditional recommendations about the need for a 3-month break after pregnancy loss [24].
Folic acid subsidies to women who have had an abortion due to congenital malformations of the fetus that are incompatible with life are extremely necessary. All women planning pregnancy need supplemental folic acid (daily dose 400–800 mcg) at least 1 month before pregnancy and throughout the first trimester (up to 12 weeks of pregnancy) [25]. Adequate saturation of the body with folates with daily use of at least 400 mcg occurs within 8–12 weeks [26, 27].
Abortion is one of the main causes of breast diseases [20]. Late abortions are absolute indications for suppression of lactation [28]. The most appropriate and rational method of inhibiting lactation is the use of prolactin inhibitors, which are agonists of dopamine 2 receptors and stimulate the production of the prolactin-inhibiting factor - 2-bromo-alpha-ergocryptine. According to studies by other authors, the effectiveness of non-hormonal rehabilitation with herbal medicine (Mastodinon) after medical termination of pregnancy has been proven [29].
The danger of the post-stress (post-abortion) period lies in the development of not only hyperplastic processes in the reproductive system, but also neuroendocrine (metabolic) syndrome. To prevent disturbances in the GGJ after abortion, along with the use of COCs and herbal medicine, the principles of rational nutrition and physical activity should be observed, physical inactivity should be reduced, and adverse environmental influences should be avoided if possible. According to the recommendations of some experts, additional rehabilitation measures after abortion may include physiotherapeutic procedures (electrophoresis, low-intensity laser), diet therapy, and adaptogens. Psychotherapy plays a significant role in rehabilitation treatment [2].
Physical factors used for rehabilitation after abortion have specific and nonspecific effects, cause general and local effects, therefore contraindications to their use should be taken into account. In the post-abortion period, preformed factors with pronounced anti-inflammatory, anti-edematous, analgesic, uterotonic, desensitizing, immunomodulatory and sedative effects are used for restorative purposes. Acting on receptor fields, functionally active zones, centers of nervous, endocrine and immune regulation, physical energy conductors restore the natural processes of homeostatic regulation of the body's functional systems. The success of such regulation is determined by the functional state of the body, the correct choice of factor, mode, localization and parameters of its action. The use of physical factors in the early post-abortion period is used for preventive purposes, in the presence of complications - for therapeutic purposes in combination with antibacterial or other therapy, and in the long-term period for the purpose of restoring reproductive health. In the post-abortion period, magnetic therapy, laser therapy, combined magneto-laser exposure, extremely high-frequency therapy, low-intensity pulsed low-frequency field therapy (infectious therapy), and electrotherapy (dynamic, interference currents) are used [30]. The researchers also presented an analysis of the effectiveness of using magnetic laser therapy in the correction of metabolic disorders after abortion [2].
Thus, the addition of the order of the Ministry of Health of the Russian Federation [9] with detailed documents made it possible to quickly bring the regulatory framework of medical institutions in line with the requirements of the time and introduce modern methods in order to improve the quality of medical care for women with forced termination of pregnancy at a late stage. The introduction of the clinical protocol “Medical termination of pregnancy” also makes it possible to effectively use the experience of foreign countries and specialized communities in conducting safe abortion in the second trimester of pregnancy for medical reasons. At the same time, the tactics of managing patients after artificial termination of pregnancy, especially in the later stages, should not include only standard therapy for the treatment of complications, but also include the prophylactic use of COCs, herbal medicine, suppression of lactation, subsidies of folic acid, and physiotherapy to prevent any consequences which can negatively affect a woman’s health. With timely implementation of rehabilitation measures, the number of complications will decrease, which will lead to a significant improvement in the reproductive health of the female population.
Literature
- Kvashenko V.P., Aykashev S.A. On the issue of preserving reproductive health when terminating an unwanted and unplanned pregnancy // Women’s Health. 2010. No. 4. pp. 24–28.
- Serov V.N., Zavalko A.F. Prevention of metabolic syndrome after medical abortion // Obstetrics and Gynecology. 2010. No. 6. P. 54–59.
- Devyatova E. A., Tsaturova K. A., Esmurzieva Z. I., Vartanyan E. V. Safe abortion // Obstetrics and gynecology: news, opinions, training. 2015. No. 3. P. 52–59.
- Kolombet E.V., Kravchenko E.N., Sabitova N.L., Yaminova D.M. Experience of medical termination of pregnancy at different stages of gestation // Vesti MANEB of the Omsk region. 2014. No. 1 (4). pp. 22–23.
- Kravchenko E. N., Kolombet E. V. Termination of pregnancy in late stages / In the book: Obstetric almanac. Ed. E. N. Kravchenko. Omsk: Antares, 2016. pp. 202–220.
- Speroff L., Darney F.D. Clinical guidelines for contraception: trans. from English / Ed. V. N. Prilepskoy. M.: BINOM. 2009.
- Melnik T.N., Serova O.F. Rehabilitation after medical abortion is the way to preserve women’s reproductive health // Russian Medical Journal. 2007. T. 15. No. 17. P. 1266–1269.
- Filippov O. S., Tokova Z. Z., Gata A. S., Kuzemin A. A., Gudimova V. V. Abortion: features of statistics in the Federal districts of Russia // Gynecology. 2016. T. 18. No. 1. P. 92–96.
- Order of the Ministry of Health of Russia dated November 12, 2012 No. 572n “On approval of the Procedure for providing medical care in the field of obstetrics and gynecology (except for the use of assisted reproductive technologies).”
- Clinical recommendations of the Ministry of Health of the Russian Federation on medical termination of pregnancy in the first trimester // Status Praesens. Gynecology, obstetrics, infertile marriage. 2015. No. 6 (9). pp. 135–145.
- Kravchenko E. N., Kolombet E. V., Kuklina L. V. Modern aspects of late pregnancy termination // Mother and Child in Kuzbass. 2016. No. 1. P. 9–13.
- Lasachko S. A., Shudrikova N. V. Prevention of possible complications and rehabilitation of women after medical abortion // Medical and social problems of the family. 2013. No. 8 (3). pp. 100–104.
- Adamyan L.V., Kuzmin V.N., Arslanyan K.N., Kharchenko E.I., Loginova O.N. Features of the use of antibacterial drugs in obstetric practice. The problem of antibiotic therapy // Attending Physician. 2015. No. 11. P. 51.
- Kuzmin V.N. Modern approaches to the treatment of inflammatory diseases of the pelvic organs // Consilium Medicinum. 2009. No. 6 (11). pp. 21–23.
- Kuzmin V.N., Adamyan L.V., Pustovalov D.A. Sexually transmitted infections and women’s reproductive health. M.: AlPrint. 2010.
- Revenko O. O. Suchasna comprehensive antibiotic prophylaxis of post-abortion inflammatory conditions // Women’s Health. 2012. No. 3 (69). pp. 11–15.
- Polyakova V. A. Practical obstetrics. Tyumen: Pechatnik Publishing House, 2012.
- Savelyeva I. S., Plotko E. E., Baykova M. K. Reducing the risk of infectious complications during artificial termination of pregnancy and the possibility of subsequent rehabilitation // Obstetrics and Gynecology. 2011. No. 7–2. pp. 60–66.
- Serov V.N. Hormonal contraception as a method of rehabilitation after abortion // Gynecology. 2010. T. 12. No. 2. pp. 26–28.
- Khamoshina M. B., Savelyeva I. S., Zorina E. A., Tulupova M. S., Zulumyan T. N. Post-abortion rehabilitation - facets of the problem: what can combined oral contraceptives do // Gynecology. 2013. No. 1. Issue. 15. pp. 60–63.
- Karahalis L. Yu., Ryabinkina T. S. Abortion and endometriosis: a walk through a minefield. Therapeutic strategy for post-abortion rehabilitation to combat endometriosis // Status praesens. 2015. No. 2 (25). pp. 87–94.
- Prilepskaya V.N., Kuzemina A.A. Abortion in the first trimester of pregnancy. M.: GEOTAR-Media, 2010.
- Love ER, Bhattacharya S., Smith NC Bhattacharya S. Effect of interpregnancy interval on outcomes of pregnancy after miscarriage: retrospective analysis of hospital episode statistics in Scotland // BMJ. 2010; 341: c. 3967.
- Wong LF, Schliep KC, Silver RM et al. The effect of a very short interpregnancy interval and pregnancy outcomes following a previous pregnancy loss // Am. J. Obstet Gynecol. 2015; 212(3):375.
- FIGO Working Group on Best Practice in Maternal–Fetal Medicine // International Journal of Gynecology and Obstetrics. 2015; 128:80–82.
- Lamers Y., Prinz-Langenohl R., Brämswig S., Pietrzik K. Red blood cell folate concentrations increase more after supplementation with [6 S]-5-methyltetrahydrofolate than with folic acid in women of childbearing age // Am. J. Clin Nutr. 2006; 84(1):156–161.
- Pietrzik K., Lamers Y., Brämswig S., Prinz-Langenohl R. Calculation of red blood cell folate steady state conditions and elimination kinetics after daily supplementation with various folate forms and doses in wom- en in childbearing age // Am J Clin Nutr. 2007; 86:1414–1419.
- Shmakov R.G., Emelyanova A.I., Polushkina E.E. Modern aspects of lactation suppression // Attending Physician. 2011. No. 9.
- Sandakova E. A., Skryabina V. V., Rylova O. V. Rehabilitation of women after medical abortion // Obstetrics and gynecology. 2010. No. 6. pp. 119–122.
- Ipatova M.V., Malanova T.B., Kubitskaya Yu.V. Modern physiotherapy in the prevention and treatment of complications after artificial termination of pregnancy in the first trimester // Gynecology. 2015. T. 17. No. 2. pp. 81–84.
E. N. Kravchenko1, Doctor of Medical Sciences, Professor E. V. Colombet
Federal State Budgetary Educational Institution of Higher Education Omsk State Medical University of the Ministry of Health of the Russian Federation, Omsk
1 Contact information
Where to do vacuum aspiration
Vacuum abortion, like any other type of abortion, is performed only in a medical institution.
Our clinic has a fully equipped gynecologist's office, as well as an operating room for more complex surgical interventions.
Advantages of choosing our clinic to receive vacuum cleaning services:
- our own laboratory makes it possible to quickly pass all the necessary tests before an abortion within the walls of one institution and obtain accurate results;
- all medical personnel work in one team, so any specialist can be involved in solving problems with abortion;
- extensive experience in vacuum aspiration has been gained;
- medical confidentiality is guaranteed;
- attentive and polite attitude, help from a psychologist.
Abortion of any kind causes damage to a woman’s body. Choosing a clinic and doctor is very important to minimize risks and give birth to a healthy child in the future.
Publication date 2019-12-03
Answers to frequently asked questions:
- How to get tested for gynecological diseases?
- What diseases does a gynecologist treat?
- What tests can be done by a gynecologist?
- How to prepare for an appointment with a gynecologist?
- Where to go with a gynecological problem?
- What symptoms should you consult a gynecologist for?
- How often should you visit a gynecologist?
- What diagnostics can a gynecologist perform in your clinic?
- What gynecological equipment do you have in your clinic?
- Gynecological care in the clinic
- Gynecological care at home
- How to call a gynecologist at home?
- How to make an appointment with a gynecologist?
Reviews of doctors providing the service - Curettage of the uterine cavity
This is a Doctor with a capital D.
Competent, thinking, analyzing, sensitive, you will never leave with an unsolved problem, ever. You will always get the help you need, competent, balanced treatment, they will support you and instill faith that everything will be fine! I am eternally grateful to the doctor for the pregnancy, for her... Read the full review Irina Aleksandrovna Yu
22.07.2021
I am very grateful to Dmitry Anatolyevich Zaporozhtsev, the head of the gynecological department and my attending physician. Thank you very much for your professional and humane approach to solving my problem of treating fibroids. Good health to you, Dmitry Anatolyevich, live long and happily. I also want... Read full review
Tatyana Mikhailovna T
17.07.2021