Pigmentation after chemical peeling.
Many cosmetologists refuse to do chemical peels for people with skin type 4 or higher. The reason is that keratinocytes “lie” close to the surface of the skin in people with skin type 4+, much closer than in people with other skin types. Therefore, chemical peeling can damage them, which will lead to age spots. The second reason for pigmentation after peeling is that chemical peeling is a burn to the skin, which causes inflammation in the skin, which in turn in the sun will accelerate the occurrence of photodamage, which will lead to skin pigmentation. Therefore, the main rule after chemical peels is maximum sun protection for the skin at any time of the year. And maximum attention to the correct choice of this protection.
We act without fanaticism
So, procedures are by no means always the only cause of pigmentation disorders. But they add this risk. Therefore, even when peeling within the stratum corneum, it is important to act “without fanaticism.” If you get too carried away and practice such peels every day, pigmentation may eventually appear. For well-groomed skin, one procedure per month is quite enough. And to reduce pores, you can use not only peelings, but also special masks, creams and lotions.
“We must really understand that it is impossible to make the skin fundamentally better than what nature intended,” warns Natalia Polonskaya. - There is no need to traumatize and tease her endlessly. If you really want to take care of yourself, in addition to traumatic manipulations, there are massages, gymnastics, and fairly effective non-traumatic cosmetic procedures. Yes, the arsenal of cosmetic products has expanded. We began to take better care of ourselves. But at the same time, getting carried away, trying to escape from age and problems, sometimes we do a lot of unnecessary things. As a result, we encounter not only skin pigmentation disorders, but also dilated blood vessels, dehydration, and increased skin sensitivity. Alas, no global miracle has happened yet. It is impossible to stop time and replace old skin with new one. This must be accepted and stopped in time. So that later you don’t have to cover up the traces of intensive self-care with a thick layer of makeup.”
Pigmentation from cosmetics.
Marketers force manufacturers to make cosmetics that the client “expects”, and not those that work “correctly”. And this is not even a question of the safety of ingredients, it is a question of demand, which generates supply. A simple example: The composition of a day cream includes ingredients that should not be there, but which will greatly increase sales. For example, anti-aging ingredients - Vitamin A, Retinol. More recently, Retinol was found even in sunscreens, which is unacceptable. Using Retinol during the day can lead to serious photodamage, which will result not only in pigmentation. Another danger is “unfair” sunscreens. These are creams that protect only from one type of radiation, or creams with a maximum level of protection of 50+, which cause a false sense of security. Another danger is using cleansers, toners, acne-fighting products or other alcohol-based cosmetics before going outside. Alcohol in cosmetics, when it comes into contact with the skin, increases the skin's photosensitivity, which can lead to pigmentation.
Correction of post-traumatic pigmentation after aggressive laser procedures
Bragina Irina Yurievna, candidate of medical sciences, dermatologist, cosmetologist, physiotherapist, gerontologist.
Expert instructor of the European Laser Academy of Health LA&HA, vice-president of the Medical Laser Academy of Russia (MLAR), member of the American Society of Laser Medicine and Surgery (ASLMS), member of the Society of Aesthetic Medicine of Russia (OEM), specialist in the field of laser technologies and rehabilitation. Scientific director of the laser direction and curator of the Fotona brand of the SportMedImport Group of Companies. Post-inflammatory hyperpigmentation (PIH)
is the most common acquired pigmentation disorder. The prevalence and intensity of this aesthetic problem are associated with the cause, duration and intensity of inflammation preceding pigmentation.
Post-inflammatory hyperpigmentation is darkening of the skin that occurs after an inflammatory rash or skin trauma. This condition is the result of a response of melanocytes to skin damage, which causes an increase in melanin production and/or its redistribution.
Pathogenesis of PIH
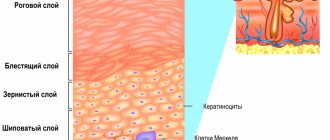
Hyperpigmentation has the following development mechanism. Inflammatory processes in the dermis and epidermis lead to the release and oxidation of arachidonic acid with the formation of prostaglandins, leukotrienes, etc. These inflammatory factors damage the functioning of immune cells and melanocytes. Depending on the depth of the lesion, epidermal or dermal melanosis develops.
The epidermal form of post-inflammatory pigmentation is characterized by increased production and transport of melanin into surrounding keratinocytes. Clinically, the deposition of melanin granules results in darkening of the skin. The intradermal form of PIH results from inflammation-induced damage to basal keratinocytes, which secrete large amounts of melanin. The free pigment is phagocytosed in the upper dermis by macrophages, now called melanophages, and gives the skin a blue-gray appearance at the site of injury.
Other factors in the formation of PIH:
- the influence of UV radiation, which provokes tyrosinase-dependent melanogenesis. Melanomas are transferred to keratinocytes;
- genetics, taking medications, antibiotics. In these cases, melanostimulating hormone is released, which leads to increased sensitivity of the skin to UV;
- endocrinopathies, COCs (estrogen), pregnancy. The production of tyrosinase is activated, resulting in increased melanin synthesis.
Women are several times more likely to develop PIH than men. The role of the endocrine and immune systems in the development of post-traumatic pigmentation
The formation of PIH largely depends on the functioning of the immune and endocrine systems. Stress hormones play a significant role in the formation of post-traumatic pigmentation. Corticotropin stimulates the secretion of adrenocorticotropic hormone from the pituitary gland and cortisol. In addition, under its influence, hormones of the sympathetic nervous system are released from the nerve ganglia and nerve endings. Under stress, the concentration of androgenic hormones in the blood increases. Testosterone causes spasm of skin blood vessels in areas with a high content of receptors. There is a deterioration in local tissue reactivity. These processes, even with minor trauma or inflammation of the skin, can lead to chronic inflammation and the appearance of keloid scars.
Stress has a suppressive effect on the immune system, mainly due to an increase in the concentration of glucocorticoids. They inhibit the production of a number of pro-inflammatory cytokines (IL1, IL6, TNFa, etc.), reduce the number of circulating lymphocytes, macrophages and basophils, and with long-term exposure cause apoptosis of lymphocytes and thymic atrophy.
In depression, there is an excess of cortisol secretion in the adrenal cortex.
This hormone cannot affect the hypothalamus and pituitary gland and stop the production of stress hormones. The immune system turns out to be weakened, since for a long time all the body’s forces were thrown into overcoming a stressful situation, neglecting the interests of the immune system. The influence of hormones on processes in the skin
| Corticosteroids and pituitary adrenocorticotropic hormone | Inhibits the mitotic activity of fibroblasts, but accelerates their differentiation |
| Mineralocorticoids | Strengthen the inflammatory response, stimulate the development of all elements of connective tissue, accelerate epithelization |
| Somatotropic hormone of the pituitary gland | Enhances cell proliferation, collagen formation, granulation tissue formation |
| Thyroid hormones | Stimulates the metabolism of connective tissue cells and their proliferation, the development of granulation tissue, collagen formation and wound healing |
| Sex hormones (estrogens) | Lack of hormones slows down reparative processes |
| Sex hormones (androgens) | Activate fibroblast activity |
Hormonal imbalance leads to deterioration of microcirculation and a decrease in the skin's ability to regenerate.
Consequences of these processes:
- decreased elasticity of vascular walls and increased permeability. This prolongs the period of edema after the procedure;
- dysfunction of neurohumoral regulation, which causes persistent vasodilation. These processes lead to blood stasis;
- expansion of the capillaries of the superficial vascular network, which triggers the development of erythema, vascular mesh, telangiectasia;
- increasing the period of wound epithelization.
Prevention of PIH formation:
- Careful collection of anamnesis (and its recording in the patient’s chart)
- Avoidance of active work with high parameters in patients of phototypes III – IV
- Mandatory use of sunscreen after any procedures involving skin trauma
- Controlling the prescription of medications with photosensitizing properties
To prevent PIH, substances that perform the following functions are used:
- prevention of post-inflammatory hyperpigmentation (anti-inflammatory, antiseptic, astringent effect). Tranexamic acid and fern extract (Fernblok) are used;
- protection from UV radiation, which stimulates the development of pigmentation (sunscreens);
- antioxidant effect. It is provided by: fern extract (Fernblok),
- procyanidin (vitamin P, catechins);
- interference in the hormonal regulation of melanogenesis.
- The use of hardware technologies (LLLT, LED, MCT, UST) helps prevent post-inflammatory hyperpigmentation and also has an antioxidant effect on the skin.
Preparing to work with post-traumatic pigmentation
The preparatory period before PIH correction is especially important when working with patients at risk:
- smokers;
- patients in a state of hormonal, vitamin, microelement deficiency;
- persons experiencing chronic stress;
- patients with a symptom complex of microcirculation disorders (edema).
Objectives of the preparatory period:
1. Reducing the patient’s rehabilitation time:
- restoration of microcirculation;
- strengthening antioxidant status;
- control of inflammation.
2. Reducing the risk of side effects and complications after laser procedures:
- increasing immunity;
- improvement of microcirculation;
- increased antioxidant status;
- normalization of melanogenesis.
3. Increasing the efficiency of procedures:
- increase in the amount of “addressed” chromophore;
- reduction in the number of competitive chromophores;
- introduction of specialized sensitizers.
In the process of preparing for the correction of PIH, external agents, pharmacotherapy, physical factors, and injection methods are used. Their tasks:
- increased antioxidant status;
- activation of collagen synthetic function;
- decreased skin reactivity;
- prevention of pigmentation.
Patient management: choice of technologies taking into account the phase of the wound process Patient management at the acute stage
| Technology | AFT (warm and hot modes) | Peeling (warm and hot modes) |
| Wound process phase | Old phase |
| Objectives of the rehabilitation period | Control of the inflammatory process, formation of crusts, maintaining a moist environment in the wound, protection against infection |
| Form of medicine | Aerosols, sprays, gels, emulsions, balms, dressings |
| Means by mechanism of action | — Reparative and wound-healing drugs. - Painkillers. - Anti-inflammatory drugs. - Antiviral drugs. - Antioxidants. | — Reparative and wound-healing drugs. - Antiviral drugs. — Antibacterial drugs. - Anti-inflammatory drugs. - Antioxidants. |
Patient management at the acute stage of the wound process is carried out using open, closed and conditionally closed methods. When the wound surface becomes infected, the following drugs are used: Actovegin, Dioxyzol, Levosin, Levomekol, Mephenate, Acerbin, Olazol. The use of a low-intensity therapeutic infrared laser allows you to achieve the following results:
- reduction of intense swelling and tension in tissues;
- reducing the duration of inflammation phases;
- increasing the speed of blood flow and increasing the absorption of oxygen by tissues;
- decreased receptor sensitivity;
- an increase in the number of new vascular collaterals;
- activation of transport substances through the vascular wall;
- analgesia and inflammation relief;
- activation of blood microcirculation, increasing the level of trophic provision of tissues;
- stimulation of immunity and reparative processes;
- reflexogenic effect on the functional activity of various organs and systems;
- activation of cell metabolism, increasing their functional activity.
- Effects of using LILI
| DNA damage | Protein kinases involved in the formation of mRNA, as well as protein synthesis (RNA, DNA) are activated |
| Inflammation | The accumulation and release of ATP are activated. IL-6 mRNA levels decrease, modulation of PDGF, TGF-β, interleukins (IL-13 and IL-15, MMP), which are also associated with abnormal wound healing |
| Immunosuppression | There is an indirect effect on the cellular and humoral components of the immune system involved in antiviral reactions, and not a direct inactivating effect of the virus. Possible systemic inhibitory effect on delayed hypersensitivity reactions. Activation and proliferation of lymphocytes and macrophages, as well as the synthesis and expression of cytokines |
| Damage to the extracellular matrix | The increase in collagen production occurs due to an increasing effect on PDGF and fibroblast production, which occurs due to decreased apoptosis, increased vascular perfusion, bFGF and TGF-β. Decreasing IL-6 and increasing TIMPs, which in turn decrease MMPs, all help in reducing collagen degradation. Activation of ATP accumulation and release |
Management of a patient at the proliferative stage
| Requirements for the drug | AFL | Plane |
| Foam preparations, ointment forms |
Patient management at the reconstructive stage
| Requirements for the drug | AFL | Plane |
| Inflammatory phase | 3rd, remodeling phase |
| Form of medicine | Emulsions, creams |
| Objectives of the rehabilitation period | — High-quality restoration of the epidermis — Activation of metabolic and reparative processes in the dermis — Prevention of hyperpigmentation — Reduction of the severity of post-traumatic erythema — Restoration of TEWL |
| Means by mechanism of action | — Reparative — Antioxidant — Blocking melanin synthesis — Complex drugs |
Classification of pigmentation correction methods by mechanism of action:
- methods that reduce melanin production (depigmenting drugs, mesotherapy, oral agents);
- exfoliating procedures (peelings, microdermabrasion);
- those that destroy melanin (laser therapy, IPL (Intense Pulsed Light) therapy).
To lighten the skin and relieve inflammation, plant antioxidants and natural extracts are used.
The acceleration of exfoliation of keratinocytes with accumulated melanin is facilitated by the use of retinol, AHA acids, enzymatic peelings and ultrasound peeling. The main idea of these procedures is natural exfoliation of the skin without inflammation or suppression of this process. The role of photoprotection in the correction of post-traumatic pigmentation
To prevent the formation of pigmentation, patients must use sunscreen. Without the use of photoprotection, any procedures will have minimal effectiveness.
The following types of sunscreens are distinguished:
- chemical protection: Avobesin (UVA), Oxybenzone;
- physical protection: titanium dioxide, zinc oxide;
- combined protection (physical + chemical): Octyl methoxycinamate + zinc oxide, Parsol, Mexoril, Tinosorb S, M, Eusolex;
- natural filters: shea butter, caffeic acid, aloe, etc.;
- antioxidants;
- reparants (aloe, panthenol, hyaluronic acid).
To protect skin with post-traumatic pigmentation, sunscreens with a protection level of 30 or higher are suitable.
Patients are advised to avoid sunlight, as well as protect the skin with hats, clothing, and glasses. Depigmentation therapy: hardware methods
The use of laser technologies for the correction of PIH allows achieving clinical effects due to the absorption of light energy by skin chromophores. During the procedures, melanocytes are heated and damaged by thermal diffusion from heated melanosomes. The pigmented lesion darkens and peels off after 1-3 weeks.
Hardware technologies and features of their application
The use of Q-Switch lasers shows high efficiency in the treatment of PIH. They combine short (nanosecond) and ultrashort (picosecond) pulse durations. Features of picosecond lasers compared to nanosecond lasers are the impact on chromophores with a higher peak power and extremely short pulse duration. The duration of laser pulses for removing nanosized targets should be in the picosecond range. For this reason, picosecond laser processing allows for more efficient targeted energy transfer to significantly smaller chromophores. Picosecond pulses allow the use of lower fluences by enhancing the photoacoustic effect. This leads to a reduction in collateral damage due to less heating of surrounding tissues and less active formation of cavitation bubbles.
The absorption of a huge amount of energy in a short period of time leads to the implementation of a predominantly photoacoustic effect. The target "explodes" with the formation of many tiny "debris". In the case of using nanosecond lasers, results are also achieved mainly due to the photoacoustic effect. In this case, the energy of the target is transmitted over a longer period of time, due to which it is crushed into large fragments. Around the destroyed target chromophore in the epidermis or dermis, high-intensity zones of microdestruction are formed, caused by the impact of a “blast wave”. It is assumed that these areas of microtrauma are a trigger for the launch of remodeling processes in the dermal layer and the production of new collagen, mucin and elastin. These processes improve the condition of wrinkles and atrophic scars.
Fotona's StarWalker technology combines the high-energy capabilities of nanosecond lasers with the ultra-short pulse peak powers of traditional picosecond lasers. This combination allows you to influence a larger number of particles of different sizes than pico and nano separately. This feature increases the effectiveness of action on target tissues.
StarWalker's unique TMD (transverse mode) laser oscillator technology, combined with ASP pulse control, delivers very short (5 nsec) Q-switching pulses, consisting of a high-energy stream of ultra-short pulses of energy, in trillionths of a second.
This provides a photomechanical effect to break up tiny skin objects without damaging the surrounding skin. When using this device, handpieces with both full and fractional beams are used. High-energy capabilities of nanosecond lasers with ultrashort pulses peak powers of traditional picosecond lasers
When choosing the wavelength, they are guided by the principle of subcellular selective photothermolysis. In accordance with this principle, it is necessary to use high peak power and ultrashort pulse duration [5 ns]. This causes only the melanin in the target cell to be destroyed and leaves the cell alive. This technology is radically different from traditional treatment methods. They were based on the principle of selective photothermolysis, which leads to the destruction and death of pigment-containing cells.
The choice of laser radiation wavelength depends on the depth of melanin.
| Melanin depth | Clinical features |
| Epidermal | melanin in the basal and suprabasal layers of the epidermis; clear boundaries; light or dark brown color; Wood's lamp has clear contrast; responds well to treatment |
| Dermal | melanin granules in the dermis; unclear boundaries; gray-blue tint; in Wood's lamp the boundaries are not obvious; difficult to treat |
| Mixed | most common type; a combination of blue, light brown and dark spots; mixed painting in Wood's lamp; highly variable treatments |
StarWalker technology allows you to work with all possible wavelengths to correct post-traumatic pigmentation.
Advantages of StarWalker non-ablative Qs lasers:
- the ability to perform mild procedures that do not require anesthesia;
- very short skin recovery time;
- no side effects.
Fractional handpieces used:
FS20A (Nd:YAG);
- “spot” size: 10 x 10 mm;
- pixel size: 200 µm;
number of pixels: 81 (9 x 9 pixels). FS50 (KTP):
- “spot” size: 10 x 10 mm;
- pixel size: 200 µm;
- number of pixels: 25 (5 x 5 pixels).
FS50B (KTP):
- “spot” size: 5 x 5 mm;
- pixel size: 200 µm;
- number of pixels: 25 (5 x 5 pixels).
Principles of application of Q-Switch lasers
| Q-Switched Lasers (QSwitch) | Depth of exposure in accordance with the level of pigment occurrence | Special indications for use (types of hyperpigmentation) | Notes |
| KTP Nd:Yag laser 532 nm (frequency doubled neodymium (Nd:YAG) laser with wavelength 532 nm) | Epidermal layer of skin to basement membrane | Epidermal pigmentation: epidermal melasma; “café au lait” spots; lentigo | Radiation with a wavelength of 532 nm is well absorbed by oxyhemoglobin. After the procedure, bruising and purpura may appear, which completely disappear after 1-2 weeks |
| Ruby laser 694 nm with QSW (light skin only) | Upper dermis | Epidermal, dermal pigmentation: chloasma; lentigo; café au lait spots | I-II PHOTOTYPE Oxyhemoglobin does not act as a competing chromophore; there is no purpura or bruising after irradiation |
| Alexandrite laser (755 nm) with QSW (for very fair skin) | Middle departments | Epidermal, dermal pigmentation: melasma; chloasma; lentigo; “café au lait” spots; nevus of Ota; Becker's nevus | I-II –III PHOTOTYPE |
| Neodymium Nd:Yag laser 1064 nm with QSW (for all skin phototypes) | Deep layers of the dermis | Epidermal, dermal pigmentation: melasma; chloasma; lentigo; “café au lait” spots; nevus of Ota; Becker's nevus | I-IV-VI PHOTOTYPE |
Combination therapy in the treatment of PIH
Combination therapy shows higher effectiveness in correcting PIH than single use of individual drugs. For the treatment of melasma, the most widely used formula is Kligman's formula (HQ 5%, tretinoin 0.1% and Dexamethasone 0.1%). The combination of azelaic acid with 0.05% tretinoin or 15-20% glycolic acid can lead to earlier and more pronounced skin lightening . Kojic acid 2% in combination with HQ 2% is superior to glycolic acid 10% and HQ 2%. Glycolic acid 10% plus HQ 4% in a vitamin C and E cream and sunscreen was effective in 75% of patients.
The new combination of HQ 4%, tretinoin 0.05% and fluocinolone acetonide 0.01% (Tri-Luma®) was effective in 77% of patients.
Measures to prevent the formation of PIH:
- selection of adequate operating parameters (processing of skin without overlap; competently selected coverage area; selection of parameters corresponding to the impact zone);
- taking into account the general condition of the patients;
- correct choice of anatomical zone.
Proper preparation for laser procedures, taking into account the individual condition of the patient’s skin, as well as the use of suitable operating parameters, can effectively eliminate PIH and prevent its formation.