Skin structure
The skin consists of 3 layers: epidermis, dermis and subcutaneous fat (SAT) (Fig. 1). The epidermis is the thinnest of them and is a stratified keratinizing epithelium. The dermis is the middle layer of the skin. Mainly composed of fibrils of the structural protein collagen. PFA contains fat cells - adipocytes. The thickness of these layers can vary significantly depending on the anatomical location.
Fig.1. Skin structure
Epidermis
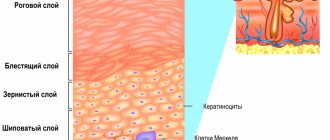
Rice.
2. Epidermis The epidermis is a constantly exfoliating epithelial layer of the skin, which consists mainly of 2 types of cells - keratinocytes and dendritic cells. Melanocytes, Langerhans cells, Merkel cells, and intraepidermal T lymphocytes are present in small quantities in the epidermis. Structurally, the epidermis is divided into 5 layers: basal, spinous, granular, shiny and horny, differing in the position and degree of differentiation of keratinocytes, the main cell population of the epidermis (Fig. 2).
Keratinization. As keratinocytes differentiate and move from the basal layer to the stratum corneum, their keratinization (keratinization) occurs - a process that begins with the phase of keratin synthesis by keratinocytes and ends with their cellular degradation. Keratin serves as a building block for intermediate filaments. Bundles of these filaments, reaching the cytoplasmic membrane, form desmosomes necessary for the formation of strong contacts between neighboring cells. Further, as epithelial differentiation progresses, epidermal cells enter the degradation phase. The nuclei and cytoplasmic organelles are destroyed and disappear, metabolism stops, and cell apoptosis occurs when it is completely keratinized (turns into horny scales).
The basal layer of the epidermis consists of a single row of mitotically active keratinocytes, which divide on average every 24 hours and give rise to new cells in the overlying epidermal layers. They are activated only in special cases, such as when a wound occurs. Next, a new cell, a keratinocyte, is pushed into the spinous layer, where it spends up to 2 weeks, gradually approaching the granular layer. The movement of the cell to the stratum corneum takes another 14 days. Thus, the lifespan of a keratinocyte is about 28 days.
It should be noted that not all cells of the basal layer divide at the same rate as keratinocytes. Epidermal stem cells under normal conditions form a long-lived population with a slow proliferation cycle.
The spinous layer of the epidermis consists of 5-10 layers of keratinocytes, differing in shape, structure and intracellular content, which is determined by the position of the cell. Thus, closer to the basal layer, the cells have a polyhedral shape and a round nucleus, but as the cells approach the granular layer, they become larger, acquire a flatter shape, and lamellar granules appear in them, containing various hydrolytic enzymes in abundance. Cells intensively synthesize keratin filaments, which, gathering into intermediate filaments, remain unconnected on the nuclear side, but participate in the formation of multiple desmosomes on the membrane side, forming connections with neighboring cells. The presence of a large number of desmosomes gives this layer a spiny appearance, for which it received the name “spinous.”
The granular layer of the epidermis is composed of still living keratinocytes, distinguished by their flattened shape and a large number of keratohyalin granules. The latter are responsible for the synthesis and modification of proteins involved in keratinization. The granular layer is the most keratogenic layer of the epidermis. In addition to keratohyalin granules, keratinocytes of this layer contain large quantities of lysosomal granules. Their enzymes break down cellular organelles during the transition of the keratinocyte to the phase of terminal differentiation and subsequent apoptosis. The thickness of the granular layer can vary; its value, proportional to the thickness of the overlying stratum corneum, is maximum in the skin of the palms and soles of the feet.
The shiny layer of the epidermis (so named for its special shine when viewing skin preparations on a light microscope) is thin, consists of flat keratinocytes, in which the nuclei and organelles are completely destroyed. The cells are filled with eleidin, an intermediate form of keratin. It is well developed only in some parts of the body - on the palms and soles.
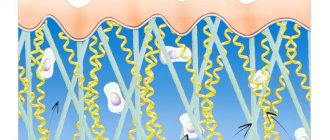
The stratum corneum of the epidermis is composed of corneocytes (dead, terminally differentiated keratinocytes) with a high protein content. The cells are surrounded by a waterproof lipid matrix, the components of which contain compounds necessary for exfoliation of the stratum corneum (Fig. 3). The physical and biochemical properties of cells in the stratum corneum vary depending on the position of the cell within the layer, directing the exfoliation process outward. For example, cells in the middle layers of the stratum corneum have stronger water-binding properties due to the high concentration of free amino acids in their cytoplasm.
Rice. 3. Schematic representation of the stratum corneum with the underlying granular layer of the epidermis.
Regulation of proliferation and differentiation of epidermal keratinocytes. Being a continuously renewing tissue, the epidermis contains a relatively constant number of cells and regulates all interactions and contacts between them: adhesion between keratinocytes, interaction between keratinocytes and migrating cells, adhesion with the basement membrane and underlying dermis, the process of terminal differentiation into corneocytes. The main mechanism for regulating homeostasis in the epidermis is supported by a number of signaling molecules - hormones, growth factors and cytokines. In addition, epidermal morphogenesis and differentiation are partially regulated by the underlying dermis, which plays a critical role in maintaining postnatal skin structure and function.
Treatment of hyperkeratosis
If symptoms of hyperkeratosis occur, you should consult a dermatologist. For an experienced, qualified specialist, it is not difficult to diagnose the presence of hyperkeratosis. Only in isolated cases, to clarify the nature of the formations, a biopsy of suspicious areas of the skin is required.
To effectively eliminate the problem of hyperkeratosis, especially affecting the skin of the face, complex therapy is required. It is also necessary to prescribe treatment for the disease that provoked its development, if one has been detected. To do this, the patient may need to consult not only a dermatologist, but also an endocrinologist or other specialist.
As part of the treatment of hyperkeratosis itself, drug therapy and cosmetic procedures are prescribed. The first is the use of retinoids, vitamin C, and sometimes topical corticosteroids. For faster skin restoration and elimination of cosmetic imperfections, the following is recommended:
- paraffin therapy;
- mild chemical peels;
- UV therapy;
- mesotherapy.
The use of scrubs and other mechanical exfoliation products is not indicated for hyperkeratosis. This will only worsen the situation and can lead to skin infection. But it is always recommended to apply emollients to the skin, which moisturize and soften the skin. They contain natural lipids or natural oils that nourish dry skin and saturate it with the substances it needs. As a result, it is possible to restore the skin’s natural protection and restore its natural smoothness.
In case of seborrheic hyperkeratosis, accompanied by the formation of growths, they can be removed using electrocoagulation, laser or cryodestruction.
Unfortunately, hyperkeratoses often accompany chronic diseases, which cannot be completely eliminated. Recovery can only be achieved in situations where thickening and peeling of the skin is caused by mechanical factors or treatable diseases, such as mycosis. In other cases, when dryness and thickening of the skin are caused by chronic dermatological or other pathologies, it is only possible to reduce the frequency of their exacerbations and the severity of the course, that is, to achieve a stable and long-term remission. But this requires the correct selection of treatment tactics, constant skin care, and often diet.
Drug therapy
First of all, vitamin A, also called retinol, and vitamin C are prescribed internally and externally. Normally, a person receives the necessary vitamins from food, but today rarely anyone can boast of a balanced diet.
Vitamin A, in addition to regulating cell growth, is necessary to maintain visual acuity, hair and nail growth, and also performs a number of other functions. For hyperkeratosis, vitamin A in the form of synthetic derivatives called retinoids is used for general and local therapy.
Some of the brightest representatives of this kind of drugs are Roaccutane, in which isotretinoin is the active ingredient, and Neotigazon, containing acitretin. These compounds are derivatives of retinoic acid. In the case of the development of follicular hyperkeratosis, the use of topical retinoids, in particular adapalene, is indicated.
If hyperkeratosis, especially follicular hyperkeratosis, is accompanied by an inflammatory process, topical corticosteroids are prescribed, for example, drugs based on hydrocortisone, prednisolone, fluacinolone, clobetasol. Most modern drugs in this group are available in several dosage forms: emulsions, creams, ointments. Moreover, the effectiveness of treatment largely depends on the correctness of its choice. Additionally, corticosteroids help accelerate the exfoliation of dead cells.
Paraffin therapy
Paraffin therapy is a cosmetic procedure in which special cosmetic molten paraffin is applied with a brush to a previously cleaned face or other areas of the body affected by hyperkeratosis. The procedure takes on average 20-60 minutes and promotes:
- gentle removal of dead cells;
- cleansing pores of impurities;
- activation of microcirculation;
- moisturizing the skin;
- reducing inflammation.
Peelings
For hyperkeratosis, chemical peelings are indicated, in particular using acids such as:
- salicylic;
- glycolic;
- dairy;
- lemon;
- apple;
- tartaric.
All of them have a good exfoliating effect, and also additionally open pores and moisturize the skin. As a result, it is possible to effectively solve the problem of excessive dryness and flaking of the skin, as well as improve its tone and texture, restoring velvety.
UV therapy
Ultraviolet irradiation helps eliminate the manifestations of hyperkeratosis by suppressing pathogenic microorganisms, including fungi, activating blood circulation and metabolism, suppressing the inflammatory process, and providing a regenerative and desensitizing effect.
Mesotherapy
Mesotherapy is a well-known cosmetic procedure, which consists of introducing into the skin the substances necessary for its proper functioning using numerous injections or using hardware. As a result, it is possible not only to saturate the tissues with vitamins, but also to achieve effective hydration, which helps reduce the manifestations of hyperkeratosis and improve the condition of the skin in general.
Thus, hyperkeratosis is a very common disorder, although it does not affect the face as often as, for example, the feet, elbows, skin of the legs and back. However, with excessive dryness and thickening of the facial skin, even in the form of small papules, a serious aesthetic disadvantage occurs. But with a timely visit to a dermatologist and the start of complex therapy, including the use of modern cosmetic procedures, it is possible to significantly improve the condition of the skin of the face and other parts of the body or even completely eliminate the signs of hyperkeratosis.
5 4 votes
Article rating
Dermis
The dermis is a complex, loose connective tissue consisting of individual fibers, cells, a network of blood vessels and nerve endings, as well as epidermal outgrowths surrounding the hair follicles and sebaceous glands. The cellular elements of the dermis are represented by fibroblasts, macrophages and mast cells. Lymphocytes, leukocytes, and other cells are capable of migrating into the dermis in response to various stimuli.
The dermis, making up the main volume of the skin, performs primarily trophic and supporting functions, providing the skin with such mechanical properties as plasticity, elasticity and strength, which it needs to protect the internal organs of the body from mechanical damage. The dermis also retains water, participates in thermoregulation and contains mechanoreceptors. Finally, its interaction with the epidermis supports the normal functioning of these layers of skin.
In the dermis there is no such directed and structured process of cell differentiation as in the epidermis, however, it also exhibits a clear structural organization of elements depending on the depth of their occurrence. Both the cells and the extracellular matrix of the dermis also undergo constant renewal and remodeling.
The extracellular matrix (ECM) of the dermis, or intercellular substance, which consists of various proteins (mainly collagen, elastin), glycosaminoglycans, the most famous of which is hyaluronic acid, and proteoglycans (fibronectin, laminin, decorin, versican, fibrillin). All these substances are secreted by dermal fibroblasts. The ECM is not a random accumulation of all components, but a complexly organized network, the composition and architectonics of which determine such biomechanical properties of the skin as rigidity, extensibility and elasticity. Epidermal keratinocytes, which are closely connected to each other, are attached to the ECM proteins. They form a dense protective layer of the skin. The structure of the ECM is also capable of exerting a regulatory effect on the cells immersed in it. Regulation can be either direct or indirect. In the first case, ECM proteins and glycosaminoglycans directly interact with cell receptors and initiate specific signal transduction pathways in them. Indirect regulation is carried out through the action of cytokines and growth factors retained in the cells of the ECM network and released at a certain moment to interact with cell receptors. The ECM structural network is subject to remodeling by enzymes from the matrix metalloproteinase (MMP) family. In particular, MMP-1 and MMP-13 initiate the degradation of collagen types I and III. The density of the ECM network of the dermis is uneven - in the papillary layer it is looser, in the reticular layer it is much denser, both due to the closer arrangement of the fibers of structural proteins and due to the increase in the diameter of these fibers.
Collagen is one of the main components of the ECM of the dermis. Synthesized by fibroblasts. The process of its biosynthesis is complex and multi-stage, as a result of which the fibroblast secretes procollagen into the extracellular space, consisting of three polypeptide α-chains folded into one triple helix. Procollagen monomers are then enzymatically assembled into extended fibrillar structures of various types. In total, there are at least 15 types of collagen in the skin; in the dermis, types I, III and V of this protein are most abundant: 88, 10 and 2%, respectively. Type IV collagen is localized in the basement membrane zone, and type VII collagen, secreted by keratinocytes, plays the role of an adapter protein for attaching ECM fibrils to the basement membrane (Fig. 4). Fibers of structural collagens of types I, III and V serve as a framework to which other ECM proteins are attached, in particular collagens of types XII and XIV. It is believed that these minor collagens, as well as small proteoglycans (decorin, fibromodulin and lumican), regulate the formation of structural collagen fibers, their diameter and the density of the formed network. The interaction of oligomeric and polymeric collagen complexes with other proteins, ECM polysaccharides, various growth factors and cytokines leads to the formation of a special network with certain biological activity, stability and biophysical characteristics important for the normal functioning of the skin. In the papillary layer of the dermis, collagen fibers are located loosely and more freely, while its reticular layer contains larger strands of collagen fibers.
Rice. 4. Schematic representation of skin layers and distribution of different types of collagens.
Collagen is constantly renewed, degrading under the action of proteolytic enzymes collagenases and being replaced by newly synthesized fibers. This protein makes up 70% of the skin's dry weight. It is the collagen fibers that “withstand the blow” under mechanical influence on it.
Elastin forms another network of fibers in the dermis, giving the skin such qualities as firmness and elasticity. Compared to collagen, elastin fibers are less rigid and curl around collagen fibers. It is with elastin fibers that proteins such as fibulins and fibrillins bind, to which, in turn, latent TGF-β-binding protein (LTBP) binds. Dissociation of this complex results in the release and activation of TGF-β, the most potent of all growth factors. It controls the expression, deposition and distribution of collagens and other matrix proteins in the skin. Thus, the intact network of elastin fibers serves as a depot for TGF-β.
Hyaluronic acid (HA) is a linear polysaccharide consisting of repeating dimers of D-glucuronic acid and N-acetylglucosamine. The number of dimers in the polymer varies, which leads to the formation of HA molecules of different molecular weights and lengths - 1x105-107 Da (2-25 μm), which, accordingly, have different biological effects.
HA is a highly hydrophilic substance that affects the movement and distribution of water in the dermal matrix. Thanks to this property, our skin, normally and in youth, has high turgor and resistance to mechanical pressure.
HA easily forms secondary hydrogen bonds both within one molecule and between neighboring molecules. In the first case, they ensure the formation of relatively rigid spiral structures. In the second, association with other HA molecules and nonspecific interaction with cell membranes occurs, which leads to the formation of a network of polysaccharide polymers with fibroblasts included in it. Shorter molecules of proteoglycans (versican, lumican, decorin, etc.) “sit” on a long HA molecule, like on a thread, forming aggregates of enormous sizes. Extended in all directions, they create a scaffold, contributing to the stabilization of the ECM protein network and fixing fibroblasts in a specific matrix environment. Taken together, all these properties of HA endow the matrix with certain chemical characteristics - viscosity, density of “cells” and stability. However, the ECM network is a dynamic structure that depends on the state of the organism. For example, under conditions of inflammation, HA aggregates with proteoglycans dissociate, and the formation of new aggregates between newly synthesized HA molecules (renewed every 3 days) and proteoglycans is blocked. This leads to a change in the spatial structure of the matrix: the size of its cells increases, the distribution of all fibers changes, the structure becomes looser, the cells change their shape and functional activity. All this affects the condition of the skin, leading to a decrease in its tone.
In addition to regulating water balance and stabilizing the ECM, HA plays an important regulatory role in maintaining epidermal and dermal homeostasis. HA actively regulates dynamic processes in the epidermis, including keratinocyte proliferation and differentiation, oxidative stress and inflammatory response, maintenance of the epidermal barrier and wound healing. In the dermis, HA also regulates fibroblast activity and collagen synthesis. By remodeling the matrix, HA controls the functioning of cells in the matrix, influencing their availability to various growth factors and changing their functional activity. Cell migration and the immune response in tissue depend on the action of GC. Thus, changes in the distribution, organization, molecular weight and metabolism of GCs have significant physiological consequences.
Fibroblasts are the main type of cellular elements of the dermis. It is these cells that are responsible for the production of HA, collagen, elastin, fibronectin and many other intercellular matrix proteins necessary for the formation of connective tissue. Fibroblasts in different layers of the dermis differ both morphologically and functionally. Not only the amount of collagen they synthesize depends on the depth of their location in the dermis, but also the ratio of the types of this collagen, for example types I and III, as well as the synthesis of collagenase: fibroblasts in the deeper layers of the dermis produce less of it. In general, fibroblasts are very plastic cells, capable of changing their functions and physiological response and even differentiating into another cell type depending on the stimulus received. The role of the latter can be played by signaling molecules synthesized by neighboring cells and the restructuring of the surrounding ECM.
The structure of human skin and its main functions
Skin is one of the types of tissue of the human body, which has a number of inherent properties such as: elasticity, strength, some porosity, waterproofness, sensitivity and antibacteriality.
The skin protects the body from the negative effects of the environment (from excess solar radiation, for example), it is capable of secreting fat and producing odorous substances, selectively absorbing some chemicals useful to the body and rejecting others. In addition, the skin has such an important function as regeneration, which gives it the ability to independently recover from damage.
On average, there are about 5 million hairs on the surface of the skin of an adult, with about 200 receptors and 100 pores located on each square centimeter.
Which layers of skin are affected by cosmetics?
In accordance with the legislation of most countries, cosmetic products can only affect the outer layers of the skin; their deep penetration and impact on the living layers of the skin is unacceptable. That is, cosmetics should have exclusively external use, which is its fundamental difference from medications.
It should be noted here that there is no barrier in the lower part of the epidermis that could effectively prevent the penetration of cosmetics into the lymphatic and blood vessels, and, consequently, the distribution of the substances they contain throughout the human body. The possibility of effective exchange between the dermis and epidermis has been proven experimentally; accordingly, the risk of substances crossing the transepidermal barrier is quite high.
What substances are able to overcome the transepidermal barrier and enter the dermis?
It was experimentally established that substances such as caffeine, nicotine, hyaluronic acid, essential oils, vitamin E (it accumulates at the border of the dermis and epidermis). Nanoparticles contained in sunscreens penetrate deep into the skin, as well as liposomes, which easily penetrate into the deep layers of the skin and deliver the necessary nutrients there.
The structure of human skin
The versatility and multifunctionality of the skin is based on the characteristics of its structure. Our skin consists of 3 important layers, each of which performs its own function:
|
Epidermis The epidermis is the outer layer of skin, which consists of keratinized (dead) skin cells. In layers of the epidermis distant from the surface, the cells are living. They actively divide and make a slow movement to the surface, where over time they are replaced by keratinized ones, and then peel off.
The epidermis is an effective barrier to water and aqueous solutions . Fat-soluble substances penetrate the skin through the epidermis much better. This is due to the fact that cell membranes themselves contain a significant amount of fats and fat-soluble substances dissolve in them naturally.
Almost all epidermal cells produce keratin , which is why they are called keratinocytes. These keratinocytes are in constant motion, as a result of which the keratinocyte loses its own nucleus and main organelles, turning into a kind of flat “bag” filled with keratin - a corneocyte. Corneocytes form the stratum corneum of dead epidermal cells and look like flat scales. They are responsible for the barrier function of the epidermis. Corneocytes are held together by a double layer of lipids (ceramides), a kind of plastic “cement.”
The basal layer of the skin contains melanocytes, which produce melanin . Melanin is a pigment that gives our skin color and reduces the effects of external radiation. So, thanks to its presence, the skin completely blocks infrared rays and is partially capable of blocking ultraviolet rays. Often, the formation of pigment spots on the skin will depend on the condition of the basement membrane. The epidermis also contains Langerhans cells, which protect the body from microbes and foreign bodies .
The thickness of the epidermis and the rate of its renewal As a rule, the thickness of the epidermis layer varies from 0.07 to 0.12 millimeters (this is the usual thickness of a sheet of paper or plastic film). Especially rough skin can be much thicker - up to 2 mm. (on the soles of your feet, for example). The process of skin cell renewal is continuous. During our lifetime, we get rid of approximately 18 kg of dead skin, while losing about 10 billion cells every day.
The rate of complete renewal of the outer layer of the epidermis slows down with age. So, if in childhood and adolescence this process takes 21-28 days, then already at 25 years old 35-45, and after 50 years 56-72 days.
The process of division and advancement of mature skin cells is not only slower, but also heterogeneous in different areas, which also affects the aesthetic appearance of the skin. If dead skin cells become layered, the cell division process occurs more slowly, leading to faster skin aging. In addition, the layer of dead cells makes it difficult for oxygen and nutrients to penetrate the skin. Therefore, the older a person is, the more often peelings are required.
Dermis The dermis is the inner layer of the skin, which also contains functional skin glands, thanks to which excess salts and moisture are removed from the body: sweat and sebaceous glands, producing sweat and sebum, respectively.
Sebum protects the skin from the aggressive effects of the external environment and gives the skin such properties as bactericidal (due to the acidic environment it creates and then has a detrimental effect on microorganisms) and water resistance. Sweat glands, in addition, participate in the natural thermoregulation of the body.
Hypodermis The hypodermis is a subcutaneous fat layer that protects us from both excess cold and excess heat, and in addition significantly mitigates damage from impacts.
Subcutaneous fatty tissue is capable of storing fat-soluble vitamins such as A, E, F, and K. An important function of the hypodermis is that it serves as the basis for the outer layers of the skin. Skin whose hypodermis layer is weakly expressed has more folds and wrinkles and is subject to faster aging. Another important function of the hypodermis is the hormone-producing function. Adipose tissue is not only capable of accumulating estrogens, but also stimulating their synthesis.
The hypodermis layer also contains leptin, a unique hormone responsible for the feeling of fullness during meals. Thanks to it, the body is able to regulate our appetite and, as a direct consequence, the amount of fat in the subcutaneous layer.
Subcutaneous fat
Subcutaneous fat, or hypodermis, is the lowest layer of skin, located under the dermis. It consists of fat lobules separated from each other by connective tissue septa containing collagen and penetrated by large vessels. The main cells of fat lobules are adipocytes, the number of which varies in different areas of the body. Currently, PFA is considered not only as an energy depot, but also as an endocrine organ, the adipocytes of which are involved in the production of a number of hormones (leptin, adiponectin, resistin), cytokines and mediators that affect metabolism, insulin sensitivity, reproductive and immune functional activity. systems
Treatment of the disease
Treatment should be carried out by a dermatologist.
You need to visit a specialist after the first appearance of keratomas, since it is important to exclude the malignant nature of the formation. Treatment is long-term and complex, usually including a number of activities.
Conservative therapy
It is carried out with the aim of reducing the number of keratoses before moving on to radical methods of treatment.
Therapeutic agents reduce symptoms and alleviate the course of the disease, but do not cure completely.
Therapeutic agents reduce symptoms and alleviate the course of the disease, but do not cure completely.
To soften keratonic areas, applications using drugs with urea (content - from 12 to 30%) are used: Keratosan, Ureaderm, Ureatop, Akerat..
The following drugs are used in therapeutic treatment: Fluorouracil, Efudex cream, Diclofenac Gel 3%, Imiquimod. Special shampoos are used to treat keratosis of the scalp. Retinoids are taken internally, which help reduce the growth rate of formations, as well as vitamins of groups A, B and C. Additionally, courses of physiotherapy are prescribed.
Radical methods of treating keratosis
Since conservative therapy for keratosis does not guarantee complete cure, it is often necessary to proceed to radical measures - direct removal of the formations. The use of drastic techniques is especially justified if there is a risk of keratosis degenerating into cancer.
The following radical methods of therapy exist:
- Cryodestruction - freezing with liquid nitrogen.
- Radio wave removal. The formation is excised using a radio knife under the influence of radio waves.
- Electrocoagulation - the doctor performs cauterization using high-frequency electric current.
- Laser destruction - a targeted effect of a carbon dioxide laser is applied to the keratoma.
- Photodynamic therapy - methyl aminolevulinate is applied to the affected area with further exposure to a light wave of a certain length. All this leads to necrosis of the affected tissues.
- Surgical removal - the skin is scraped with a curette (special instrument).
- Dermabrasion – removal using an abrasive brush.