I did lymphatic drainage massages - to no avail. How to remove bags on the cheekbones that only old people have, but I have had since childhood?
What methods of elimination are there and what are the reasons for the formation of paint bags - we will tell you today in this article.
Photos from open sources
Diseases
Not always, swelling and bruising under the eyes are a sign of an unhealthy lifestyle. Often, the reason is the presence of certain diseases:
- Allergies. Accompanied by lacrimation, sneezing, redness of the eyes, difficulty breathing and coughing;
- Inflammation of the sinuses (sinusitis and sinusitis). They occur with painful sensations localized in the forehead and under the eyes, as well as copious discharge from the nose;
- Kidney diseases. When they occur, fluid retention occurs in the body, which causes not only swelling of the eyes, but also lower back pain and headaches;
- Diseases of the thyroid gland. Due to dysfunction of the thyroid gland, hormonal imbalance occurs - general weakness increases, body weight increases, the menstrual cycle changes, edema occurs;
- Heart failure. It is accompanied by shortness of breath and fatigue. Swelling and bruising under the eyes, almost invisible in the morning, appear in the late afternoon;
- Skin diseases - eczema and dermatitis.
How to remove puffiness under the eyes
There are many techniques for improving the condition of the periorbital zone. But first you need to pay attention to your general health and the presence of accompanying warning signs: difficulty breathing, prolonged pain of any intensity localization, organ dysfunction, problems with blood pressure, and so on. In such cases, immediate consultation with a doctor and examination is required.
If bags and bruises are only a cosmetic defect, you can get rid of them using different techniques.
Heart failure
In the case when the appearance of bags under the eyes is accompanied by shortness of breath, pain in the heart, and peripheral edema, the cause may lie in heart failure. If the functioning of the heart is disrupted, then the entire body suffers from a lack of nutrients and oxygen. First, swelling forms in the legs, and then spreads to other tissues and organs. Facial swelling is a sign of anasarca, which threatens the patient's life and is an extreme manifestation of heart failure. To confirm the diagnosis, you need to perform an ultrasound of the heart, an ECG and a number of other studies.
In men and women, the incidence of swelling under the eyes is approximately the same, but in children this symptom rarely occurs, therefore, in some cases it goes unnoticed.
Bag under the right eye and its treatment
When, as a result of a comprehensive examination, the causes of swelling on the face are identified, an effective method of therapy is outlined.
If doctors, based on the results of the examination, have determined that swelling under the eye is a symptom of some disease, efforts should be focused on getting rid of the disease itself. Well, if it is determined that the bag under the right eye is the result of a cosmetic defect, you should slightly change the environment and behavior habits, in particular:
- Radically change the lighting of the place where the main daytime is spent - office, kitchen, garage. Provide rooms with as much natural light as possible;
- Be sure to take 5-10 minute breaks for every 1.5 - 2 hours of work in front of a computer monitor;
- Women who use cosmetics, which may be the reason why a bag appeared right under the right eye, should remove makeup with special cosmetic solutions and face creams before going to bed;
- Before a night's rest, avoid spicy foods, plenty of liquids, beer and other alcoholic beverages. Such dietary restrictions also reduce the risk of developing a bag under the right eye;
- A healthy eight-hour night's sleep improves complexion and the condition of the areas around the eyes of the facial skin. The right pillow does not provoke contraction of the neck muscles.
Bags, hernias or swelling?
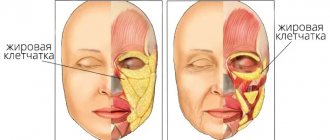
First, let's list all the formations that can be found in an older patient.
The formations under the eyes can be swelling, they can be sagging skin of the lower eyelid, or they can be fatty hernias.
Fig.1. 1 - swelling under the eyes; 2 - ridge of the lower eyelid during facial activity; 3 - lower eyelid hernia; 4.5 — manifestations of the nasolacrimal groove; 6 - sagging skin of the lower eyelid, facial wrinkles.
Patients often refer to swelling of the lower eyelid area as bags. Their origin has nothing to do with the redistribution of fat packets; usually it is fluid stagnation and problems with the lymphatic drainage system.
What diseases can cause swollen eyes?
This symptom accompanies not only ophthalmological pathologies. It may be associated with systemic diseases. For example:
- gastrointestinal diseases;
- pathologies of the pituitary gland, thyroid gland;
- diseases of the gastrointestinal tract;
- infectious, viral diseases;
- liver and kidney diseases.
The list goes on, because there are more than 70 diseases that are accompanied by swelling of the eyelids. This could indicate problems with almost any organ.
Prevention measures
It is impossible to completely prevent the formation of hernias under the eyes.
Remember! But you can prevent their rapid development by following these preventive recommendations:
- from time to time wipe your face with ice cubes , for the preparation of which it is better to use not water, but decoctions of medicinal herbs;
- avoid abuse of alcohol, fatty, smoked and spicy foods and, if possible, quit smoking;
- go to bed on time and not disturb the established daily routine;
- Regularly take at least half an hour walks to improve the overall tone of the body.
Causes
There are dozens of pathological and non-pathological reasons for the development of puffiness under the eyes. As a rule, in these cases the symptom occurs simultaneously under the left and right eye.
Harmless reasons
Relatively harmless non-pathological causes include:
- sleep disorders (irregular sleep, insomnia, sleeping at different times);
- problems with excess weight (in this case, a violation of the water-salt balance develops, and some of the fluid accumulates under the eyes);
- exposure to regular long-term stress ;
- excessive consumption of alcoholic beverages;
- unhealthy diet (abuse of fatty and salty foods in particular);
- constant exposure of the skin to sunlight and wind , frequent changes in ambient temperature;
- excessive physical activity or, on the contrary, a sedentary lifestyle . In both cases, the balance of fluid in the body is also disturbed and its uneven distribution occurs.
With such problems, eliminating the root cause yourself is usually not difficult, and swelling can be eliminated at home using cosmetics or traditional medicine.
Diseases
Remember! It is worse if the cause of such a violation is pathological conditions and lesions, for which the intervention of specialists cannot be avoided.
Such reasons include:
- Problems with venous or lymphatic drainage . In such situations, the outflow pathways of venous blood or lymph are blocked, as a result of which such fluids stagnate in different parts of the body. But such places of congestion under the eyes are especially noticeable, since the skin here is quite thin. Such disorders can occur both in various ophthalmological inflammatory diseases and as a result of unsuccessful cosmetic procedures.
- Pathologies of internal organs . Disturbances in circulatory processes are characteristic of diseases of the thyroid gland, kidneys and cardiovascular system.
- Ophthalmological diseases accompanied by inflammatory processes. Most often, barley, conjunctivitis, chalazion and furunculosis. In these cases, swelling does not occur due to fluid accumulation, but due to structural changes in the affected tissues.
- Diseases of the paranasal sinuses (any type of sinusitis). Swelling in this case is explained by the close location of the pathological areas to the organs of vision. And the swelling itself does not develop in the under-eye area, but spreads from the maxillary sinuses, where it initially appears.
Important! Often the cause of the development of swelling is allergic reactions, with additional symptoms being irritation, redness of the conjunctiva, itching, sneezing, and lacrimation.
Heredity should not be ruled out: some people have a genetic predisposition to puffiness under the eyes.
And this is often observed in newborns, in whom such a disorder can persist in the first few months of life and then disappear.
Symptoms
Hernias under the eyes can be recognized by the following signs:
- decreased visual acuity;
- increased lacrimation;
- swollen areas of skin under the eyes do not decrease or increase during the day or when drinking large amounts of water;
- the skin of the eyelids, under which hernias form, takes on a bluish or reddish, plum color;
- the vascular network may more or less appear on the skin of the eyelids.
such hernias also form above the eye - then from the outside it seems that the person’s eye shape is reduced and the swelling affects the periocular area in a circle.
Keep in mind! For the vast majority of people, this problem appears only under the eyes.
What will not help in the fight against paint bags:
1. Botox. Promotes even more bag formation. The injected muscle becomes inactive as before, and the outflow of lymph becomes more difficult. Swelling appears above the paint bags - another swelling that will further focus attention on the problem.
2. Fillers with hyaluronic acid, if they are injected superficially. The problem is that any drugs that are injected superficially into this area cause swelling. Because paint grease is very hydrophilic and attracts water.
3. Injections of direct lipolytics (which destroy fat). May lead to atrophy. Indirect - have a lymphatic drainage effect and reduce swelling (but do not destroy fat.
Photos from open sources
Diagnostics
It is worth noting! If you are sure that such processes occur due to possible diseases of the eyes or internal organs, you need to contact a therapist who will prescribe a number of diagnostic procedures, including:
- Blood pressure measurement.
- Donating blood to perform a general analysis , which can show the presence of inflammatory processes in the body.
- Analysis of urine . It also allows you to diagnose inflammation, provided that an increased number of leukocytes is detected in the material for analysis.
- Radiography . It is not always prescribed, but only if there is suspicion of compression of blood vessels by neoplasms of various origins in the eye area, which leads to swelling.
- Ultrasound of the kidneys.
- Additional blood tests to determine the level of thyroid hormones. Additionally, an ultrasound of the thyroid gland may be performed. In these cases, it is possible to identify changes in this organ that lead to hormonal imbalance.
- Echocardiography and electrocardiography . The methods allow us to identify disorders of the cardiovascular system.
Attention! If necessary, examinations by other specialists can be prescribed, and based on the diagnostic results, a diagnosis will be made with subsequent treatment.
Borzokh Olga Borisovna
Candidate of Medical Sciences, dermatovenerologist, cosmetologist, researcher at the Center for Collective Use "Molecular and Cellular Technologies" of Krasnoyarsk State Medical University, Country Expert Teoxane Russia, Voronezh
The periorbital area continues to be the focus of attention of cosmetologists, since, on the one hand, this is one of the most popular requests from patients, and on the other hand, many unresolved questions remain regarding the choice of techniques or drugs. In this article, I propose to somewhat expand the focus of our attention and discuss the correction of not only the infraorbital sulcus, but also other areas around the eyes - the temporal region, the forehead, the middle third, since all these zones can influence the aging process in the periorbital region [1] .
But first of all, you need to understand what the goal of aesthetic correction is when working with age-related changes. The goal of most patients is to correct age-related manifestations, but without traces of intervention, while the most common concerns of patients are unnatural results, contouring of the drug, and swelling in the periorbital area. In my opinion, it is possible to help achieve a better result and natural correction by choosing the right indications and technique for performing the procedure, based on the Teoxane approach.
The Teoxane approach was developed to achieve the most effective and natural-looking aesthetic treatment results while maintaining the safety of injection procedures. When working with the Teoxane approach, we always follow the three Ps (A-T-P) - anatomy (including assessment of the aging process and patient indications), technique and drug selection.
Anatomy
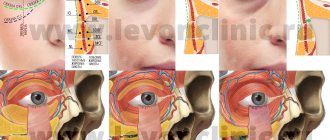
One article or even one book is not enough for the anatomical features of the area around the eyes, so I propose to dwell only on some of the anatomical aspects necessary for work.
Speaking about the area under the eyes, first of all it is necessary to understand the features of the layer-by-layer structure of the zone of the lower edge of the orbit (Fig. 1) [2].
- 1st layer - skin : in the periorbital area it is thin due to a decrease in the number of layers of the epidermis and thinning of the dermis itself;
- 2nd layer - subcutaneous fat : thin, often in Caucasian patients it can be practically absent in the area of the medial corner of the eye;
- 3rd layer - orbicularis oculi muscle : attached to the bony edge of the orbit with the help of the orbicularis oculi ligament (ORL), while its attachment is stronger in the medial corner of the eye, resulting in the formation of the tear groove;
- 4th layer - layer of deep fat pads : presented mainly lateral to the medial canthus of the eye in the form of a deep infraorbital fat pad (SOOF);
- 5th layer - periosteum.
When working in this area, the following are distinguished (Fig. 2) [3]:
- palpebral wrinkles (wrinkles on the skin of the eyelid);
- tear trough - a line of depression running from the medial edge of the eye down to the midpupillary line;
- palpebromalar groove - a lateral continuation of the lacrimal groove;
- midbuccal groove - continuation of the lacrimal groove downwards;
- nasolabial fold - in the middle third.
In the supraorbital region, the five-layer structure is preserved, but, unlike the infraorbital region, the skin is thicker, the subcutaneous fat is full, the deep fat pack is represented by the supraorbital fat pack (ROOF) (Fig. 3) [4].
The temporal region is an area where many questions remain regarding the anatomical structure. Regarding the number of layers of tissue in this area, most experts believe that 10 layers can be distinguished in it.
It is more important in this area to designate safer zones and caution zones (Fig. 4) [5]. Thus, a safer compartment is the superior temporal compartment (UTC), located between the temporal crest (superior temporal septum - STS) and the inferior temporal septum (ITS), in the inferior temporal compartment (LTS) blood vessels and nerves are located.
In the forehead area there are also 5 layers of soft tissues of the face (Fig. 5) [6]: skin, subcutaneous fat, SMAS (represented by the frontal muscle, or aponeurosis), a layer of deep fat packets and periosteum.
A safer level is the layer of deep fatty packets under the SMAS; the main vessels above the safety line (it runs 2 cm above the bony edge of the orbit) are in the superficial fatty layer, below the line - in the deep.
In the area of the midbuccal groove, five layers are also preserved: skin, superficial and deep fat packets, SMAS, periosteum [7–9]. The main level when working with volumizers is the level of deep fat packs (medial deep infraorbital fat pack and deep medial zygomatic fat pack); with pronounced age-related changes, the goal of correction is also the superficial medial fat pack.
In addition to anatomy, the first point of the Teoxane approach involves understanding the aging process in different layers:
- the skin becomes thinner, fibroblasts reduce their synthetic activity, the skin becomes overstretched and its elasticity decreases;
- in subcutaneous fatty tissue and deep fatty tissues, a decrease in fatty tissue and redistribution of fat occurs - a change in the ratio of different fatty tissues;
- muscles, as a rule, undergo atrophy, the ligamentous apparatus stretches and loses its strength;
- the periosteum (or rather, the bone) also undergoes resorption.
As a result of all these processes, we see volume deficits in the upper and middle third of the face, as well as ptosis of the eyebrows, upper eyelid, and the appearance of furrows in the infraorbital region, which appear as a result of loss of support from overlying structures.
Thus, there is a connection between volume deficits and ptosis of certain structures; therefore, replenishment of lost volume will reduce the manifestations of ptosis.
Last but not least, what we look at with the Teoxane approach in point one is patient assessment. In fact, correctly determined indications made on the basis of complaints and examination of the patient are of great importance on the path to ideal aesthetic correction of the periorbital region.
At the same time, it is important that the patient himself points out the areas that he does not like about himself, since each person has his own ideas about beauty, and areas in the patient that are incorrectly identified and corrected by the doctor can give an unsatisfactory result after the procedure. If our patient cannot decide on areas of concern to him, you can give him a mirror and “introduce him to yourself.”
Selection of equipment
The next point in Teoxane's approach is technique. This paragraph assumes the plural because, in our opinion, there is no one correct correction technique - we use our own, using a needle or cannula, but these techniques must “respect” the anatomy in terms of safety and effectiveness. To do this, on the face we highlight areas of increased attention, safety lines, and areas with a lack of volume (Fig. 6).
When working with the upper and middle third of the face, we must remember the location of the angular artery (in the inner corner of the eye), the exit of the infraorbital and supraorbital neurovascular bundles (along the midpupillary line), supratrochlear (1 cm medial to the supraorbital), zygomatic (1 cm below the lateral bony edge of the orbit), the location of the transverse artery (along the lower edge of the zygomatic arch) and the temporal vessels (most often visualized on the patient’s face).
Of the safety lines, we are interested in the midbuccal line and the line in the projection of the zygomatic major muscle - it is safer to work in the superolateral quadrant when these lines intersect. In the temporal region, the safety line runs between the tragus and the lateral edge of the orbit - it delimits the superior temporal compartment. In the forehead area, the safety line is 2 cm above the bony edge of the orbit.
When augmenting the forehead area, we may use a cannula or a needle. The drug is administered at the SMAS; before the procedure, it is important to note areas of volume deficiency, and when working with a cannula, the injection points are determined (between visible vessels) (Fig. 7). When working with a cannula, you can use one (for a more flattened forehead area) or 2 injection points (for a more rounded one); a 25G cannula is safer; a 22G cannula has a smaller diameter and is closer in sharpness to a needle. The drug is distributed fan-wise using a retrograde technique. The SMAS zone requires a distributed, dynamic drug with average G' values; we will talk about the choice of drug in the next paragraph.
To lift the eyebrow, an injection point is used, located under the eyebrow, lateral to the midpupillary line. The drug is located supraniosteally, in the region of the deep supraorbital fat pad (ROOF) (Fig. 8). Typically, when performing this technique, I raise the eyebrow and use a small bolus of drug (0.2 ml) with a high G'.
When working with the temporal region, it is safer to administer the drug deeply (under the temporalis muscle) in the superior temporal compartment. The injection point for the shot gun technique is 1 cm below the temporal crest and 1 cm above the lateral bony rim of the orbit (Fig. 9). The procedure is carried out with a needle, safer 25 mm long (a shorter needle may not be completely on the bone). The injection is made between visible vessels until it touches the bone, then the needle must be tilted so that the needle hole is as close as possible to the bone. The drug will be distributed between the fibers of the temporal muscle, since the muscle is firmly attached to the bone and there is no space under it. Due to the location of the drug, a drug with maximum G' and cohesiveness is required.
When working with infraorbital grooves, injections are carried out strictly in the area of volume deficiency; in the case of working with a cannula, you can select one injection point between the lacrimal and palpebromalar grooves, bypassing the projection of the infraorbital foramen (Fig. 10A, B). When working with a cannula, it is safer to choose larger diameter cannulas (25G, 22G). The drug is administered under the orbicularis oculi muscle. Considering the complex and delicate anatomical structure of the infraorbital region, you should carefully select the drug based on its viscoelastic properties.
When correcting the midbuccal sulcus, the volume of zygomatic fat pads is corrected, but there may be a difference in the technique in patients of the older and middle age groups.
In patients of the middle age group, in young people, with initial manifestations of volume deficiency in the area of the midbuccal sulcus in the pathogenesis of age-related changes, as a rule, only deep fatty packets are involved, therefore, in them, the introduction of a volumizer is carried out only at the level of the medial infraorbital fatty packet or at the level of the deep medial fat pack.
In older patients, volume loss occurs at the level of the superficial medial fat pad, therefore, for a full result, a multilayer technique for correcting the middle third is necessary, as we mentioned in the article [10].
When working with a needle, boluses of the drug are located supraniosteally, lateral and above the safety lines. When working with a cannula, the injection point is located lateral to the midbuccal line and the cannula passes at the level of deep fatty bags. For convenience, you can lift the tissues with your second hand and pass under them in the area of the medial infraorbital fat pad and the medial deep zygomatic fat pad (Fig. 11).
Choice of drug
Sometimes the choice of drug is not given due attention, as a result, the risks of an unnatural correction result, low effectiveness of the correction, contouring and swelling, especially in the periorbital area, increase. It is important to understand that each zone and each tissue layer may require different viscoelastic properties of the drugs. We have already spoken about the rheological properties of drugs quite a large number of times [11, 12]. Let's take a closer look at the choice of drugs based on the anatomical features of each area.
When augmenting the forehead, the space under the SMAS is quite small, there is not a large amount of tissue above it, so the pressure exerted on the injected drug is relatively low, but at the same time the zone is mimically active (movable), so an elastic drug is required, with an average G' index, capable of stretching . Teosyal® RHA2 and Teosyal® RHA3 have these properties (Table 1). Teosyal® RHA is a collection of dynamic fillers that are stretchable and, as a result, maximally adapted to the dynamics of the face. When using them, we obtain maximum efficiency in the area of administration with maximum naturalness of the result. For thinner skin, thin soft tissues and a slight lack of volume, the most suitable drug is Teosyal® RHA2, for greater thickness and the need for volume - Teosyal® RHA3. In my practice, I sometimes use Teosyal® RHA4, but only in cases of large thickness of soft tissues and pronounced loss of volume in the forehead area, when greater volumizing abilities of the drug are needed while maintaining its elastic properties. In this case, the drug should be administered as delicately as possible, avoiding overcorrection.
Table 1. Comparative characteristics of Teosyal® RHA2 and Teosyal® RHA3
| Teosyal® RHA2 _ | Teosyal® RHA3 _ | |
| Compound | Reticulated HA 23 mg/ml | Reticulated HA 23 mg/ml |
| Degree of modification (MoD) | 3,1% | 3,6% |
| Rheological properties | High tensile strength Moderate compression force | Good tensile strength High compression force |
| Indications | Moderate dynamic wrinkles and lip correction | Moderate dynamic wrinkles and lip correction |
When working with the area of the infraorbital grooves, you should choose the drug especially carefully. The anatomical features of the zone dictate the need for a lightly distributed drug (to prevent compression of the lymphatic drainage) (reducing the risk of contouring in an area with a deficiency of fatty tissue) with low residual hygroscopicity. Such a drug is Teosyal® Redensity 2 (Table 2). Teosyal® Redensity 2 was developed specifically for the correction of this delicate area, it has low residual hygroscopicity and is a light, spreadable hyaluronic acid gel. Moreover, it has official indications - correction of infraorbital grooves.
Table 2. Characteristics of the drug Teosyal® Redensity 2
| Teosyal® Redensity 2 | |
| Compound | Reticulated HA 15 mg/ml |
| Degree of modification (MoD) | 5,5% |
| Rheological properties | Good distribution, plasticity, low hygroscopicity |
| Indications | Correction of the lacrimal and palpebromalar grooves |
| Insertion depth | Under the orbicularis oculi muscle |
I have already mentioned the need to use a drug with the highest G' and the highest possible cohesiveness when augmenting the temporal region due to the location of the gel along the muscle fibers of the temporal muscle. Such drugs are Teosyal® RHA4 and Teosyal® Puresense Ultra Deep (Table 3). I generally prefer Teosyal® RHA4 for younger patients and Teosyal® Puresense Ultra Deep for older patients. Both drugs contain 0.3% lidocaine, which is extremely important when working in the area of the temporal fossa.
Table 3. Comparative characteristics of Teosyal® Puresense Ultra Deep and Teosyal® RHA4 volumizers
| Teosyal® Puresense Ultra Deep | Teosyal® RHA4 _ | |
| Compound | Reticulated HA 25 mg/ml | Reticulated HA 23 mg/ml |
| Degree of modification (MoD) | 10,0% | 4,0% |
| Rheological properties | Very high cohesiveness High elasticity | High tensile strength Very high compression force |
| Indications | Insufficient volume in a limited area: cheekbones, chin, etc. | Insufficient volume in the tensile or dynamic area: cheeks, facial contour, etc. |
| Insertion depth | Deep fat pads (nanoperiosteal) | Superficial and deep fat packets |
To carry out eyebrow lifting, I usually use the remainder (0.1–0.2 ml) of the volumizer that was used to correct the middle or upper third of the face.
And finally, when correcting the midbuccal groove, the most rational use of volumizers (see Table 3). When filling deep fat bags in older patients, patients with pronounced thickness of soft tissues, to create maximum projection, I prefer the classic rigid (that is, hard) Teosyal® Puresense Ultra Deep volumizer; it has a very high G', high cohesiveness, and maximum lifting ability. When using the multilayer technique - filling superficial fat bags with a pronounced deficiency in the area of the midbuccal groove, as well as when working with deep fat bags in patients with small thickness of soft tissues of the face, I prefer Teosyal® RHA4. Teosyal® RHA4 is a dynamic volumizer with a high G', high resistance to repetitive stress, but at the same time “respecting” facial expressions and giving the most natural correction.
Conclusion
When working with the area around the eyes, we most often choose complex techniques. The validity of the choice of complex techniques is confirmed by the peculiarities of the aging process in this area. Thus, by filling the deficit in the upper zones (such as the forehead, temporal region, eyebrow area), we restore support for the eyebrow and upper eyelid, and by restoring the middle third, we improve the results of correction of the infraorbital grooves (Fig. 12). In this example, the patient underwent augmentation of the forehead area (Teosyal® RHA4 - 1.0 ml on each side), augmentation of the temporal area (Teosyal® PS Ultra Deep - 0.4 ml each), eyebrow lifting (Teosyal® PS Ultra Deep - 0.2 ml each), correction of the midbuccal groove (Teosyal® PS Ultra Deep - 0.6 ml each) and filling of the lacrimal and palpebromalar grooves (Teosyal® Redensity 2 - 0.5 ml each). As a result, we made the face more harmonious in the ratio of the upper third to the middle and lower third, the patient looked less tired (by reducing the deficit of the middle third and the severity of the infraorbital grooves), the overhang of the eyelid decreased, and the shape of the forehead area and the deficit in the temporal region were corrected.
At the same time, in terms of complex treatment, one should not forget about restoring the quality of the skin. To fully restore the functional activity of fibroblasts, my favorite is Teosyal® Redensity 1, the results of which can be seen after the first procedure.
The article was published in the magazine “Cosmetics and Medicine Special Edition” No. 2/2021
As an advertisement
Literature
- Pessa JE An algorithm of facial aging: verification of Lambros's theory by three-dimensional stereolithography, with reference to the pathogenesis of midfacial aging, scleral show, and the lateral suborbital trough deformity. Plast Reconstr Surg 2000; 106(2): 479–488
- Vrcek I., Ozgur O., Nakra T. Infraorbital Dark Circles: A Review of the Pathogenesis, Evaluation and Treatment. J Cutan Aesthet Surg 2016; 9(2): 65–72.
- Lee JH, Hong G. Definitions of groove and hollowness of the infraorbital region and clinical treatment using soft-tissue filler. Arch Plast Surg 2018; 45(3): 214–221.
- Mustak H., Fiaschetti D., Gupta A., Goldberg R. Eyebrow Contouring with Hyaluronic Acid Gel Filler Injections. J Clin Aesthet Dermatol 2018; 11(2): 38–40.
- Huang R.L., Xie Y., Wang W., et al. Anatomical Study of Temporal Fat Compartments and its Clinical Application for Temporal Fat Grafting. Aesthet Surg J 2017; 37(8): 855–862.
- Peng JH, Peng PH HA Filler Injection and Skin Quality-Literature Minireview and Injection Techniques. Indian J Plast Surg 2020; 53(2): 198–206.
- Rohrich RJ, Pessa JE, Ristow B. The youthful cheek and the deep medial fat compartment. Plast Reconstr Surg 2008; 121(6): 2107–2112.
- Mendelson BC, Muzaffar AR, Adams WP Surgical anatomy of the midcheek and malar mounds. Plast Reconstr Surg 2002: 110(3): 885–896.
- Mendelson BC, Jacobson SR Surgical anatomy of the midcheek. Facial layers, spaces, and the mid cheek segments. Clin Plast Surg 2008; 35(3): 395–404.
- Borzykh O.B. Multi-layer technique for correction of the middle third of the face when working with the periorbital region: addition or necessity? Injection methods in cosmetology 2020; 4:20-27.
- Egorova M.L. A dynamic method of creating volume in the cheekbone area with hyaluronic fillers Teosyal Ultra Deep and Teosyal RHA. An ideal combination for maintaining the natural appearance of the face during its movements. Injection methods in cosmetology 2019; 4:32–38.
- Borzykh O.B. A combination of Teosyal Ultra Deep and Teosyal RHA4 volumizers to create a line of ideal profile. Injection methods in cosmetology 2020; 1:26–31.
Treatment
To eliminate swelling, it is enough to carry out the following measures:
- Wash with cold water. A contrast shower will increase blood circulation, which in turn will increase the outflow of excess fluid.
- Application of cosmetics. Properly cleaning the visual area every day will help prevent swelling. To quickly remove bags, certain lines of cosmetic products have also been developed.
- The development of an allergic reaction in the visual apparatus can be stopped with the help of antihistamines.
- Massage movements will speed up the removal of excess fluid under the eyes.
- A cold compress will constrict the blood capillaries and, accordingly, reduce the flow of fluid to this area. You can apply both cold spoons and ice.
- Compress based on cool water. To do this, you need to moisten a cotton pad in running water and apply it to the area where the bags are formed. If one disk heats up, it must be replaced.
- Mask based on natural ingredients. Among traditional medicine recipes, the effectiveness of potatoes and cucumbers in relieving swelling under the eyes is noted;
- Bags under the eyes can be disguised using foundation or concealer. However, cosmetics will not eradicate the health problem that has arisen.
To eliminate bags caused by internal causes, it is necessary to diagnose pathologies and begin their treatment. Among the traditional medicine methods for eliminating bags under the eyes, the following recipes are effective:
- Aloe compress. Squeeze the juice from the plant, which has the form of a gel, and distribute it under the eyes. The duration of the mask is about 10-15 minutes. It is advisable to let the juice absorb.
- To prepare an anti-puffiness mask, mix 2 tablespoons of gel and half a spoon of cucumber juice. The mixture is applied to the eyes in the evening and remains throughout the night's sleep.
- Egg yolk, which must be beaten first, will help add elasticity to the skin. The mixture is applied under the eyes for 15 minutes, then washed off with cool water.
Treatment of swelling must begin with internal provoking factors and then begin treating the symptoms themselves.
Why does swelling occur in dry eye syndrome?
Dry eye syndrome (DES) is a pathological condition that is based on a violation of the stability of the tear film.
It provides nutrition, hydration and protection to the cornea. But when few tears are produced or their composition changes, the tear film quickly begins to evaporate. Because of this, the mucous membrane dries out, a burning sensation, itching, redness, and swelling appears.
Various reasons contribute to the development of dry eye syndrome. This could be taking antidepressants, antihistamines, working at a computer for a long time, or staying in a room with dry air. Dry eye syndrome may progress during sun exposure (summer) because too much air temperature causes tears to evaporate.
You can compensate for moisture deficiency with the help of tear substitutes. These are special drops that contain moisturizing components. But, despite the fact that they have a composition close to tears, they do not contain mucins and lipids, which help the tear film to adhere to the surface of the eyeball and maintain stability.
One of the effective ways to restore the tear film is the use of Delfanto® in capsules. They contain a record amount of antioxidants (at least 35%), which help stimulate the production of your own tears.