Modern plastic surgery has a whole arsenal of tools that allow you to achieve excellent results. In the case of surgery to correct the shape and volume of the mammary glands, this is especially evident. Thousands of patients remain satisfied with the results of mammoplasty. This became possible not only due to the achievement of the desired aesthetic effect, but also due to the minimal risk of complications. At the same time, one should not deny that, although rare, they are possible. One of the complications after mammoplasty is seroma.
When does seroma appear?
Lifetime warranty on implants
There is no specific time interval between surgical intervention and the formation of seroma. It is difficult to name the factors that stimulate fluid accumulation. However, the general likelihood of developing this anomaly is as follows: the greater the extent of surgery, the greater the likelihood of developing seroma. Seroma can appear in any part of the body that has been injured or undergone surgery.
It is diagnosed during a mammological examination, but, as a rule, the accumulation is clearly visible to the naked eye and is easily palpable.
How does seroma manifest after breast augmentation?
| As a rule, in typical cases, seroma appears 4-7 days after surgery. However, it should be remembered that seroma can form at any time, even many months after surgery. The cause in such cases is most often hypothermia or injury. |
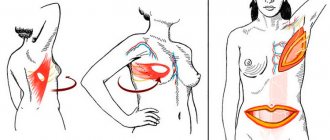
Signs of seroma are:
- Changing the shape of the breast. When serous fluid accumulates, the breasts increase in size. Fluid accumulates between the implant and the soft tissue of the breast. The contours of the mammary gland change, the volume increases.
- Swelling of the soft tissues of the chest. In the area of fluid accumulation, swelling of the surrounding tissues is noted. There may be some pain on palpation in this area.
- Pain in the seroma area. In typical cases, there is slight to moderate pain. With pressure or physical activity, the pain may intensify. With large and long-standing seromas, the pain may be more intense and have a bursting character.
- Redness of the skin in the area of seroma accumulation. Most often, the color of the skin does not change due to the accumulation of serous fluid. In some cases, with a large volume of seroma, the skin may turn red. This indicates the need to remove serous fluid as quickly as possible.
- Discharge of serous fluid through the edges of the wound. Happens rarely. If the seroma exists for a long time, a fistula tract may form through which the fluid will be released out. This occurs more often in patients with thin soft tissues and recent surgery.
Seroma formation
Seroma is not related to malignant neoplasms, but requires removal. It increases the risk of infection entering the operated area, so it requires timely treatment.
The formation of seroma is possible from a hematoma. Sometimes it is formed from lymphatic fluid due to capillary leakage. “Leakage” from blood vessels is also possible if there are breaks in them. Another risk factor is dying or damaged cells, which can cause inflammation.
Causes
With this disease there is usually no pain. Only sometimes they can appear, but only if the volume of serous fluid is very large. Therefore, it is almost impossible to immediately recognize the presence of seroma.
Most often, seroma occurs as a result of damage to a large number of lymphatic capillaries , which are not able to thrombose as quickly as blood vessels. This leads to the accumulation of serous fluid. Due to the presence of blood, the seroma acquires a reddish color.
Other causes of this complication:
- Traumatic work with tissues.
Seroma postoperative
The surgeon must work with soft tissues very carefully. He should not grab them roughly or use tools that can crush the tissue. The cuts must be made very carefully, in one motion. Numerous incisions increase the area of damaged tissue several times , which contributes to the formation of seroma.
- Excessive use of coagulation.
Used if tissue burns occur. Any burn causes necrosis, accompanied by the formation of inflammatory fluid (exudate). Coagulation should be used in isolation only to cauterize the bleeding vessel.
- Greater thickness of subcutaneous fat.
It should be no more than 5 cm, otherwise a seroma almost always forms . Therefore, if the thickness of the subcutaneous fat exceeds more than 5 cm, liposuction must first be performed. Three months after this, abdominoplasty can be done.
Other causes of seroma are: old age, high blood pressure, diabetes.
Prevention and treatment
Prevention of this phenomenon is quite simple. It consists of gentle, light pressure with your hand on the operated area. In this case, you should avoid massaging the scar or pressing on it at an angle, as this can lead to sutures coming apart.
To prevent fluid from accumulating after surgery, plastic surgeons leave drainage tubes in place until the fluid has completely stopped flowing. However, accumulation is possible even after removal of the drainage.
The accumulation can resolve on its own, but the process itself can take several weeks, and its result can be a knot of calcified soft tissue. They are not harmful to the body and are clearly visualized during diagnostic studies.
Ultrasound diagnosis of an incompetent scar on the uterus in the long-term postoperative period
Ultrasound scanner HS60
Professional diagnostic tools.
Assessment of tissue elasticity, advanced 3D/4D/5D scanning capabilities, BI-RADS classifier, options for expert cardiological studies.
Introduction
Caesarean section is the most frequently performed abdominal operation, surpassing appendectomy and hernia repair combined in frequency. The increase in the frequency of cesarean sections creates a new problem, as the number of women with an operated uterus increases, and a scar on the uterus in the future is often the only indication for re-operation. Issues of the optimal frequency of cesarean section are at the center of discussions among obstetricians and gynecologists; a significant increase in the frequency of surgical delivery both abroad and in Russia has become an “alarming problem”, since the desire to solve all obstetric problems through surgery has proven untenable. The rate of cesarean section in MONIIAG, which also includes patients with an operated uterus, was 23.7% in 2008 and 24.9% in 2009; in the Moscow region this figure varies from 17.7 to 20.6% , while there is a tendency to increase the number of surgical births in the Moscow region as a whole, which accordingly entails an increase in the number of postoperative complications.
It is known that the risk of complications in the mother during abdominal delivery increases by 10-26 times [1]. During emergency operations, the frequency of these complications reaches 18.9%, and during planned operations - 4.2% [2]. Until now, endometritis is the most common (from 17 to 40% of cases). If previously endometritis developed after a planned cesarean section in 5-6% of cases, and after an emergency - in 22-85%, then the use of antibiotic prophylaxis made it possible to reduce these figures by 50-60% [3]. Postpartum endomyometritis is the main cause of the formation of a defective scar on the uterus. An important problem in the formation of a successful scar is the activity of tissue repair in the area of the wound on the uterus. The course of the healing process is determined by a large number of factors, which include: the state of the macroorganism, the surgical technique, the suture material used, the duration of the operation and blood loss, and the course of the postoperative period. Endometritis and more severe complications are often hidden behind the following masking diagnoses: bleeding in the postpartum period, subinvolution of the uterus, lochio- and hematometra, etc. In recent years, doctors are increasingly faced with the problem of incompetence of the uterine scar in the late postoperative period and at the stage of planning the next pregnancy .
The purpose of the study is to predict pregnancy complications in women with a uterine scar after cesarean section.
Material and methods
35 patients with uterine scar failure were examined, 4 patients in the first trimester of pregnancy, 31 at the stage of preconception preparation. The average age of postpartum patients was 29 years. The reason for visiting a doctor was chronic pelvic pain; exacerbation of “chronic inflammation of the appendages”; dysuric disorders; secondary infertility; pregnancy planning; confirmation of a previously made diagnosis of an incompetent scar.
Caesarean section in the lower uterine segment was performed within a period of 1 to 5 years before the study, both routinely and for emergency indications. Six examined patients underwent a repeat cesarean section, 2 with excision of the first scar, 4 without excision of the area of the previous scar. Information about previous operations was obtained only from the words of the patients; statements about the indications for surgery, features of the operation and the postoperative period were absent in most observations. Only with careful collection of anamnesis and careful questioning was it possible to identify the features of the course of the previous pregnancy and the postoperative period. The development of complications was facilitated by an “inflammatory” obstetric and gynecological history: 34.2% of patients had endometritis after childbirth; mastitis - 8.5%; wound infection - 23.5%; endometritis after abortion - 18.2%; cervical erosion - 22.8%; acute salpingoophoritis - 11.4%, chronic - 22.8% of patients; a history of previous infertility occurred in 25.7% of postpartum women; wearing an IUD prior to actual pregnancy – 5.7%.
Analysis of the birth history, which is not available in all cases, made it possible to determine the presence of technical errors during the operation: the use of rough manual techniques for removing the head (11.2%), the use of a continuous suture for suturing the uterus (34.2%), the use of reactogenic material (11 .2%), carrying out inadequate hemostasis (8.5%); the duration of the operation was more than 2 hours (5.7%), the presence of pathological blood loss (8.5%).
Features of the course and management of the postpartum period in patients were: a long period of low-grade fever (85.7%); bowel dysfunction (14.2%); the presence of urinary syndrome - episodes of frequent and/or painful urination (31.4%); presence of wound infection (17.1%); the use of various methods of local sanitation of the uterus in 74.3% of postpartum women (hysteroscopy, vacuum aspiration, cavity curettage, lavage); prescribing massive infusion therapy and long-term or repeated courses of antibacterial therapy in the postoperative period (85.7%).
All patients underwent transvaginal and transabdominal ultrasound examination and three-dimensional reconstruction. In some cases, hydrosonography and hysteroscopy were used to confirm the diagnosis.
Results and discussion
The following signs were considered as criteria for the consistency of a uterine scar in the long-term postoperative period:
- typical position of the scar (Fig. 1);
- absence of deformations, “niches”, areas of retraction from the serous membrane and the uterine cavity;
- myometrial thickness in the area of the lower uterine segment;
- absence of hematomas in the structure of the scar, connective tissue inclusions, fluid structures;
- visualization of ligatures in the myometrium depending on the duration of the operation and the suture material used;
- adequate blood flow;
- condition of the vesicouterine fold, pouch of Douglas, parametria.
Rice. 1.
Atypical position of the scar, heterogeneity of structure.
In 4 cases, an incompetent scar was detected in the first trimester of pregnancy. One patient underwent a corporal cesarean section and a Stark cesarean section. Failure was defined as a rupture of the corporal scar with prolapse of the fertilized egg under the serous membrane of the uterus (2.8%). In 3 (8.6%) cases, a sharp thinning of the scar was detected with preservation of the myometrium no more than 2 mm, retraction of the outer contour, retraction from the side of the uterine cavity. Due to the high risk of obstetric complications, termination of pregnancy and plastic surgery of the lower uterine segment were performed in all cases (Fig. 2, 3).
Rice. 2.
The perfect scar.
Rice. 3.
Pregnancy 7 weeks. Two scars on the uterus, rupture of the uterus along the scar.
1 - independent scar after cesarean section according to Stark; 2 - uterine rupture, the fertilized egg protrudes through the corporal scar.
Signs of scar failure outside pregnancy manifested themselves in the form of deformation of the outer contour of the uterus in the lower segment and at the level of the isthmus (Fig. 4), retraction of the serous membrane (Fig. 5), sharp thinning of the myometrium (Fig. 6), the presence of a “niche” on the side of the cavity uterus or destructive changes in the scar zone with the formation of multiple cavities in the myometrium (Fig. 7, 8).
Rice. 4.
Incompetent scar. A deep “niche” in the scar area. The myometrium is not defined.
Rice. 5.
Incompetent scar. Cross section. Retraction of the vesicouterine fold.
Rice. 6.
Partial failure of the scar. Thinning of the myometrium, connective tissue inclusions in the scar area.
Rice. 7.
Retrodeviation of the uterus. Tissue defect in the scar area (1).
Rice. 8.
Insolvent scar after three caesarean sections. Liquid inclusions in the lower segment. The myometrium is not defined.
In 3 (8.57%) cases, the reason for visiting a doctor was dysuric manifestations; the patients were observed and treated by a urologist for several years after the previous operation. Ultrasonography revealed inconsistency of the uterine scar, a pronounced adhesive process between the uterus and the bladder, and endometriosis of the bladder. Surgical treatment was performed: in 2 cases - laparoscopic access, in 1 case - laparotomy with excision of the endometrioid infiltrate, plastic surgery of the lower uterine segment (Fig. 9, 10).
Rice. 9.
Incompetent scar, myometrium in the area of the scar is not determined, endometriosis of the bladder.
1 - cervix; 2 - scar defect, endometriosis.
Rice. 10.
Two scars on the uterus, endometriosis of the vesicouterine fold. The arrows indicate a myometrial defect replaced by endometrial infiltrate.
Diagnosis of an incompetent uterine scar is always difficult, especially at the stage of pregnancy planning or in the early stages of an already established pregnancy. Typically, neither patients nor clinicians are willing to accept a diagnosis based on a single ultrasound examination. Verification of the diagnosis is carried out in all cases during a consultative examination and planning of surgical treatment using hydrosonography and hysteroscopy.
The presence of a “niche” on the side of the cavity in all cases was confirmed by hysteroscopy. In 16 cases, the failure of the scar was confirmed and surgical treatment was performed - excision of the scar and plastic surgery of the lower segment during laparotomy or laparoscopic access. Suture failure, reoperation, and generalization of the process were not noted in any case. Menstrual function was restored in all patients. Pregnancy subsequently occurred in 7 patients; all of them carried the pregnancy to term and were promptly delivered as living children. The remaining 22 patients refused to plan pregnancy at this stage due to the high risk.
Considering the young age of the majority of patients, to paraphrase somewhat, we can unconditionally agree with the opinion of Ya.P. Solsky that “...in terms of its socio-demographic consequences, an unfavorable or disabling outcome of an obstetric complication is much more significant than the outcome of a complication of another etiology.”
It must be recognized that in the near future one should not expect a decrease in the number of postoperative complications. This is due not only to an increase in the number of patients with immunopathology and extragenital pathology (obesity, anemia, diabetes mellitus), but also to a significant increase in operational activity in obstetrics. We are talking, in particular, about a significant increase in the number of abdominal births.
We believe that identifying the main causes of the formation of an incompetent suture on the uterus after cesarean section and early implementation of modern diagnostic and surgical measures will improve the reproductive prognosis in patients with severe postpartum complications and realize reproductive function even in the most difficult clinical situations.
Literature
- Kovganko P.A. Caesarean section operation - past and present (https://www.noviyegrani.com/archives/title/343).
- Mirov I.M. // Ross Bulletin of Obstetrics and Gynecology. 2003. 3; T. 3. P. 58-61.
- Strugatsky V.M. Our experience in managing the postpartum period in high-risk women / E.A. Chernukha [and others] // Obstetrics and gynecology. 2000. N 2. P. 47-50.
- Chernukha E.A. Generic block. M.: Triad-H. 2005; 533 pp.
Ultrasound scanner HS60
Professional diagnostic tools.
Assessment of tissue elasticity, advanced 3D/4D/5D scanning capabilities, BI-RADS classifier, options for expert cardiological studies.
Bubbles have appeared around the seam, liquid is leaking from them, the seam is getting wet, what should I do?
No. 23 760 Surgeon 08/30/2015
A herniated disc was removed 2 weeks ago. The seam was clean, on the 10th day the stitches were removed, but I was allergic to the eraser. Bandages, adhesive plaster. There was redness on the back. On the 5th day after removing the sutures, bubbles appeared around the suture, liquid flowed out of them, and the suture began to get wet. The seams were treated with chlorhexidine and brilliant green. When the seam began to get wet, the doctor prescribed bandages with levomekol, but it didn’t help.
ANSWERED: 08/30/2015
18+ Online consultations are for informational purposes only and do not replace a face-to-face consultation with a doctor. Terms of use
Your personal data is securely protected. Payments and site operation are carried out using the secure SSL protocol.
Do patients who have undergone surgery often develop allergies after surgery ? What is causing this problem? What symptoms does it accompany? Is it possible to get rid of it?
In fact, an allergic reaction is rarely directly related to surgery. After all, by and large, an allergy is a reaction of the nominal system to a particular substance. Therefore, disorders arise already in the postoperative period. But, of course, there are exceptions.
For example, some patients are allergic to latex, which is what surgical gloves are made from. In addition, an allergic reaction may result from tissue contact with certain metals used in surgical instruments. In addition, the immune system often rejects various implants or prostheses, which is accompanied not only by skin manifestations, but also by weakness, the development of an inflammatory process, suppuration and even sepsis.
Options and their features
How breast reconstruction will take place after a mastectomy is determined by several circumstances:
The volume of tissue excised during tumor removal. If the breast was only removed from the tumor, dents and scars may become a problem. This is the easiest option for reconstruction.
Sometimes all organ tissue is removed, leaving the skin and fatty tissue intact. And here restoration will not cause much difficulty. It is more difficult when the gland is completely removed; the pectoralis major muscle, lymph nodes and blood vessels, and subcutaneous fat are affected.
- The patient's condition. It is necessary that she can tolerate general anesthesia without problems.
- Features of the shape and size of healthy breasts. Sometimes it also needs to be adjusted for purely aesthetic reasons. This could be a lift or resizing.
Reconstructive surgery is performed at the same time as a mastectomy or some time after it.
Expander
Breast reconstruction can be achieved using a temporary device. This is an expander, which is a cavity with liquid. It is installed under the skin, then gradually, over several visits to the doctor, the patient is filled with saline solution using a syringe. This is necessary so that a pocket for the implant is formed in the problem area, and the preserved breast tissue is sufficiently stretched.
Breast reconstruction with tissue expander
The expander is used for 3 - 6 months. At this time, the breasts look a little unnatural. In addition, the patient will have to regularly visit the doctor, only he will be able to increase the volume of the device. There is no hurry with this.
Instead of an expander, a vacuum device can be used. This is a whole system that is worn 10-12 hours a day. It is a bowl tightly fixed to the iron. A vacuum is formed inside it, which stretches the skin.
This method is good for small breasts. It will allow you to restore it using lipofilling, that is, reconstruction with your own fat. After this procedure, your breasts will look as natural as possible. And the patient will quickly integrate into normal life after the procedure.
To learn about installing an expander, watch this video:
Musculocutaneous flap transplantation
Breast restoration is possible through transplantation of one's own tissue. Use the latissimus dorsi or rectus abdominis muscle. This method will make the breasts look very natural and will eliminate the danger of the implant moving, because in this case it is not needed. But it lasts up to 5 hours under general anesthesia and is highly traumatic, long-term rehabilitation, and a considerable amount of risks.
Breast reconstruction with tram flap
Breast reconstruction with DIEP flap
Combined method
Delayed breast reconstruction may combine both methods. This operation is appropriate for total tissue removal. First, the adjacent areas of the breast are restored using your own graft. This is done using adipose tissue, that is, by the method of lipofilling. Then the implant is installed and the myocutaneous flap is transplanted.
Of all types of intervention, this is the most difficult. But it allows you to restore the beauty of your breasts after a severe and extensive mastectomy.
Nipple and areola restoration
In almost all cases, part of the reconstructive surgery of the mammary gland is the restoration of the nipple-areolar complex. There are options here too:
- you can use tissue from the same area of another breast;
- perform a skin graft on the labia minora;
- collect the nipple from the tissue of the reconstructed breast, and mark the areola using tattooing.
For information on different options for breast reconstruction after mastectomy, watch this video:
Excessive electrocoagulation
This is another reason that causes suture gray after surgery and to some extent depends on the competence of the doctor. What is coagulation in medical practice? This is a surgical procedure performed not with a classic scalpel, but with a special coagulator that produces a high-frequency electric current. In essence, this is a targeted cauterization of blood vessels and/or cells by current. Coagulation is most often used in cosmetology. She has also proven herself excellent in surgery. But if it is performed by a physician without experience, he may incorrectly calculate the required amount of current or burn excess tissue. In this case, they undergo necrosis, and neighboring tissues become inflamed with the formation of exudate. In these cases, seroma of the postoperative suture is also assigned the code “T 80” in ICD 10, but in practice such complications are recorded very rarely.
Preparation
Preparation for sectoral resection of the mammary gland includes undergoing a thorough examination of the woman, when tests are taken for:
- prothrombin index, INR, fibrinogen, free heparin level;
- thyroid hormone levels;
- prolactin, testosterone, estradiol;
- blood levels of urea, bilirubin, AST, glucose, ALT;
- microscopy of urine sediment;
- determination of blood group and Rh factor.
If the above tests deviate from the norm, you will need to consult with a physician or a specialist specified by the physician. They will tell you what actions need to be taken to normalize the function of an organ whose indicator has deviated. In this case, rehabilitation after resection of the sector should proceed without complications.
In addition, preoperative preparation includes a blood test for the presence of antibodies to the HIV virus, hepatitis B virus, and RW. If the results of at least one test are positive, the intervention will have to be postponed and appropriate treatment will be carried out by an infectious disease specialist (if hepatitis B or HIV is detected) or a venereologist (in the case of a positive RW test).
Before the operation, it is necessary to undergo laboratory tests:
- fluorography;
- ECG;
- Ultrasound of the thyroid gland;
- mammography – ultrasound (up to 45 years) or x-ray (after 45 years).
If sectoral resection is carried out for cancer, distant metastases are excluded using tomography - computed tomography or magnetic resonance imaging - because this involves a completely different operation. Also, as preparation for the intervention, radiation therapy can be performed.
Actions before surgery
Before surgery, a woman must do the following:
- exclude taking birth control pills (in consultation with the operating surgeon and gynecologist who prescribed the drug);
- stop taking vitamin E 5 days before the intervention;
- After consulting with a therapist or cardiologist, at least 3-4 days before surgery, discontinue Aspirin, Warfarin, Curantil, Pentoxifylline or other blood-thinning drugs. Otherwise, sectoral resection may be complicated by severe bleeding;
- stop drinking alcohol or smoking, as this leads to a decrease in blood supply to tissues. The healing period in this case will be longer.
If an intervention is to be performed under general anesthesia, the last meal should be consumed 6-8 hours before, and water 4 hours before.
This is important, since the introduction of anesthesia can be complicated by vomiting, and it is dangerous on a full stomach
When planning a sectoral resection under local anesthesia, you should stop eating and drinking 4 hours before surgery.
Folk remedies
It is important to know that regardless of the reasons for the seroma of the postoperative suture, this complication is not treated with folk remedies.
But at home, you can perform a number of actions that promote healing of the suture and prevent suppuration. These include:
- lubricating the seam with antiseptic agents that do not contain alcohol (“Fukorcin”, “Betadine”);
- application of ointments (Levosin, Vulnuzan, Kontraktubeks and others);
- inclusion of vitamins in the diet.
If suppuration appears in the suture area, you need to treat it with antiseptic and alcohol-containing agents, for example, iodine. In addition, in these cases, antibiotics and anti-inflammatory drugs are prescribed.
In order to speed up the healing of stitches, traditional medicine recommends making compresses with an alcohol tincture of larkspur. Only the roots of this herb are suitable for its preparation. They are washed well from the soil, crushed in a meat grinder, put in a jar and filled with vodka. The tincture is ready for use after 15 days. For a compress, you need to dilute it with water 1:1 so that the skin does not get burned.
There are many folk remedies for healing wounds and scars after surgery. Among them are sea buckthorn oil, rosehip oil, mumiyo, beeswax, melted with olive oil. These products should be applied to gauze and applied to the scar or seam.
What is the danger of seroma?
A fairly common mistake is to underestimate the risk of seroma. You often hear the opinion that seroma will go away on its own without any treatment. Indeed, in most cases this is true. However, in some cases, seroma can lead to very unpleasant consequences, namely:
- Formation of capsular contracture. One way or another, seroma is a manifestation of aseptic inflammation. Where there is inflammation there is always a risk of excess formation of connective tissue. This is a direct road to the formation of capsular contracture during the first year. Treatment of capsular contracture, in turn, may require repeat surgery.
- Suppuration of the implantation pocket. Serous fluid is an ideal environment for bacterial growth. Long-term seroma can lead to suppuration of the implantation pocket. The infection can come from chronic foci (tonsillitis, sinusitis, chronic diseases of the genitourinary system, etc.).
- Formation of serous fistula. Sometimes the serous fluid finds its way out on its own through weak spots in the soft tissue. Most often this is the seam line. In this case, the leakage of serous fluid can last from several days to several weeks. In addition, there is a risk of infection of the implant, which will entail the need for repeated surgery.
How to treat gray?
Treatment of seroma after breast augmentation can be either surgical or medical. The most effective is a combination of both methods, provided that the seroma requires it.
The essence of surgical treatment is to install drainage with active aspiration for continuous removal of serous fluid. Drainage can remain in place for 2-5 days after installation. The amount of discharge is used to determine the possibility of drainage removal. If there is little discharge, the drainage is removed.
Drug treatment can be either independent or complementary to surgical treatment. As an independent method of treatment, it is used for small seromas in cases where the installation of active drainage is impractical. Among the drugs, non-steroidal anti-inflammatory drugs (such as Diclofenac), broad-spectrum antibiotics, as well as steroidal anti-inflammatory drugs (such as Diprospan) firmly occupy the first positions. The duration of drug treatment can vary from 5 to 14 days.
| Experience shows that timely treatment guarantees almost 100% recovery without consequences for the health and aesthetic result of the operation. The incidence of seroma after breast augmentation is 0.2-1%. This largely depends on the surgeon. Despite the low percentage, both the patient and the surgeon must be attentive in the first month after surgery so as not to miss the development of such a complication as seroma of the implantation pocket. |
How does seroma develop after breast augmentation?
| Against the background of a completely satisfactory condition, after 4-14 days the patient suddenly notices that one breast seems to have become more swollen. Most often, the patient does not pay attention to this, since the surgeon warned that at first the swelling after the operation may “walk around”. The next day, the swelling intensifies and it becomes obvious that one breast is larger than the other. At this time, pain may intensify and redness of the skin may appear. |
It's time to contact your doctor. Timely treatment in 90% of cases guarantees complete recovery without any consequences.
Clinical manifestations of seroma of small sutures
If the surgical intervention was on a small area of skin, and the suture turned out to be small (accordingly, the doctor’s traumatic manipulations affected a small volume of tissue), the seroma, as a rule, does not manifest itself in any way. In medical practice, there are cases where patients did not even suspect it, but such a formation was discovered during instrumental studies. Only in isolated cases does a small seroma cause minor pain.
How to treat it and is it necessary to do it? The decision is made by the attending physician. If he deems it necessary, he may prescribe anti-inflammatory and painkillers. Also, for faster wound healing, the doctor may prescribe a number of physiotherapeutic procedures.