Briefly about the treatment method
Skin grafting using a split skin flap is the easiest way to heal large wound surfaces.
The meaning of this plastic surgery is to use a thin 0.1-0.8 mm surface layer of skin, which is removed with a special instrument called a dermatome. This skin flap is perforated, which allows its area to be increased several times.
After this, it is placed on the prepared receptive wound and fixed with separate sutures.
As a result of the operation, the transplanted skin grows into the wound and closes it. The area from which the skin was taken heals on its own, since the germinal part of the skin remains in place.
Free skin grafting is divided into:
Vascularized
To perform such plastic surgery, microsurgical instruments, suture material, an operating surgical microscope and a complex flap for transplantation are used.
The flap is complex because the vascular network is preserved in it, and during transplantation it is anastomosed (connected) with the vessels of the affected limb of a person.
Vascularization is the formation of new vessels (usually capillaries) inside the tissue.
Nonvascularized
Initially, small pieces of the epidermis were used to perform such plastic surgery, but now this practice is rare.
Currently, thanks to the invention of a special medical instrument - a dermatome - it is possible to take and transplant large areas of skin (Thirsch skin grafting).
There are layered flaps, which cover the entire depth of the dermis, and split flaps, which contain only the superficial layers of the epidermis. After the transplant, the site where the layer-by-layer donor flap is taken is subjected to secondary plastic surgery, but after the split flap is taken, this is not necessary, since the new epithelium forms independently thanks to the preserved skin appendages.
Advantages of treatment at the ISC
Compared to other clinics in our country, the Innovative Vascular Center has undeniable advantages in the use of plastic surgery methods to treat vascular patients. In our clinic, the closure of skin wounds and trophic ulcers is carried out in a specialized department for the treatment of critical ischemia. Thus, wound treatment is carried out by surgeons, who ensure the restoration of blood circulation necessary for successful wound healing.
We are well aware of the course of wound processes in patients and we select for each case the required time and method of closing the trophic ulcer or wound. To prepare wounds for skin grafting, we use active wound surface preparation methods. Dressings and antibacterial drugs are prescribed taking into account the sensitivity of the wound microflora.
Thanks to innovative technologies, we are able to heal wounds that no other clinic in our country can handle!
"Stratagraft": effectiveness and safety
The phase III clinical trial STRATA2016 (NCT03005106) (randomized, open-label, multicenter) tested the effectiveness and safety of “Stratagraft” among adult patients (n=71) in the task of autologous regeneration of skin tissue in complex thermal skin lesions, burns of which affect the entire epidermis and more than two third dermis.
Burns to the body, arms, or legs that still contained intact dermal elements had to be eligible for excision and autologous transplantation procedures.
Randomization was carried out on each patient, when two similar burn areas of the same patient underwent either standard autodermoplasty therapy or Stratagraft treatment.
Two primary efficacy endpoints were established at 3 months post-treatment: the percentage of wound area that required an additional standard autodermoplasty procedure, and the proportion of patients who achieved wound closure without the need for autodermoplasty—100 percent reepithelialization without drainage or dressing use at two consecutive assessments at least 2 weeks apart but not more than 5 months apart, including or spanning the 3rd month time point.
Based on the results, an average of 4.3% (95% CI: 0.0–9.4) of burn areas to which Stratagraft was applied required an additional procedure of standard autodermoplasty - versus 102.1% (95% CI: 99.0 –105.2) areas that initially passed through it. In other words, Stratagraft reduced the need for traditional skin grafting by 98% (95% CI: 93.9–101.7) (p<0.0001).
83.1% (95% CI: 74.4–91.8) of patients treated with Stratagraft recorded closure of burn wounds. When standard treatment was used, 85.9% (95% CI: 77.8–94.0) of patients achieved healing.
In terms of cosmetic results, according to the Patient Observer Scar Assessment Scale (POSAS), they were better with Stratagraft. Thus, the average overall observer score (such characteristics of scars as vascularization, pigmentation, thickness, relief, pliability, surface area are assessed; less is better) was 6.3 ± 1.7 - versus 16.3 ± 7.7 (p< 0.0001).
The safety profile of Stratagraft, assessed in its four clinical trials, is comparable to that of autodermograft. The most common side effect was itching, experienced by 11% of patients. All negative reactions were mild or moderate in severity. No local infection was noted.
Preparing for treatment
For skin grafting to be successful, a number of conditions must be met. The human body must be stabilized in terms of blood and protein synthesis. It is necessary to stop the infectious process. Conditions for performing skin grafting must be local:
- Good bleeding of the wound edges, active juicy granulations.
- The wound is in the granulation stage (without signs of active infection or purulent inflammation).
- The wound must be well supplied with blood (blood circulation must first be restored).
- The wound must be kept free of dead tissue using physical and chemical methods.
General conditions for performing skin grafting:
- The protein level in the blood must be at least 60 g/liter.
- Hemoglobin level is at least 90 g/liter.
- The patient must be stabilized in general condition
Direct preparation for surgery involves shaving the skin graft site, catheterization of the bladder, and installation of an epidural catheter for anesthesia.
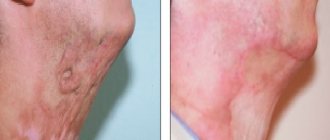
Scar correction with plastic surgery
Anesthesiology and resuscitation
| Service code | Internal code | Name | Price, rub |
| B01.003.004.007 | 37.1.1 | Spinal anesthesia lasting up to 1 hour | 8 000 |
| B01.003.004.006 | 37.1.2 | Epidural anesthesia lasting up to 1 hour | 14 000 |
| B01.003.004.008 | 37.1.3 | Spinoepidural anesthesia lasting up to 1 hour | 20 000 |
| B01.003.004.009 | 37.1.4 | Total intravenous anesthesia up to 20 minutes | 6 000 |
| B01.003.004.009 | 37.1.5 | Total intravenous anesthesia from 20 minutes to 60 minutes | 12 000 |
| B01.003.004.010 | 37.1.6 | Endotracheal anesthesia from 1 hour to 2 hours | 20 000 |
| B01.003.004.010 | 37.1.7 | Endotracheal anesthesia from 2 hours to 3 hours | 26 000 |
| B01.003.004.010 | 37.1.8 | Endotracheal anesthesia from 3 hours to 4 hours | 34 000 |
| B01.003.004.010 | 37.1.9 | Endotracheal anesthesia from 5 to 6 hours | 58 000 |
| B03.016.011 | 37.1.10 | Express analysis of blood gases and electrolytes | 2 000 |
| B03.016.011 | 37.1.11 | Advanced express analysis of blood gases and electrolytes | 2 500 |
| B03.016.011 | 37.1.12 | Artificial ventilation for 12 hours | 7 200 |
| B01.003.004.010 | 37.1.13 | Endotracheal anesthesia up to 1 hour | 14 000 |
| B01.003.004.010 | 37.1.14 | Endotracheal anesthesia from 4 to 5 hours | 40 000 |
| B01.003.004.002 | 37.1.15 | Conduction anesthesia of the 1st category of complexity | 4 000 |
| B01.003.004.005 | 37.1.16 | Infiltration anesthesia (large volume or area) up to 30 minutes | 3 000 |
| B01.003.004.005 | 37.1.17 | Infiltration anesthesia up to 15 minutes | 1 400 |
| B01.003.004.004 | 37.1.18 | Application anesthesia | 1 000 |
| B01.003.004.009 | 37.1.19 | Drug sedation with hemodynamic monitoring | 3 000 |
| B01.003.004 | 37.1.20 | Prolonged regional anesthesia (days) | 8 000 |
| A11.12.001 | 37.1.21 | central vein catheterization | 10 000 |
| A11.23.002 | 37.1.22 | TAP TEST | 12 500 |
| A11.23.001 | 37.1.23 | Diagnostic spinal (lumbar) puncture | 3 500 |
| B01.003.004.007 | 37.1.1.2 | Spinal anesthesia from 1 hour to 2 hours | 14 000 |
| B01.003.004.007 | 37.1.1.3 | Spinal anesthesia from 2 hours to 3 hours | 17 000 |
| B01.003.004.007 | 37.1.1.4 | Spinal anesthesia from 3 hours to 4 hours | 20 000 |
| A11.23.003.001 | 37.1.2.1 | Placement of an epidural catheter | 8 000 |
| B01.003.004.006 | 37.1.2.2 | Epidural anesthesia from 1 hour to 2 hours | 17 000 |
| B01.003.004.006 | 37.1.2.3 | Epidural anesthesia from 2 hours to 3 hours | 21 000 |
| B01.003.004.006 | 37.1.2.4 | Epidural anesthesia from 3 hours to 4 hours | 24 000 |
| B01.003.004.006 | 37.1.2.5 | Epidural anesthesia from 4 hours to 5 hours | 28 000 |
| B01.003.004.008 | 37.1.3.1 | Spinoepidural anesthesia from 1 hour to 2 hours | 22 000 |
| B01.003.004.008 | 37.1.3.2 | Spinoepidural anesthesia from 2 hours to 3 hours | 26 000 |
| B01.003.004.008 | 37.1.3.3 | Spinoepidural anesthesia from 3 hours to 4 hours | 27 000 |
| B01.003.004.008 | 37.1.3.4 | Spinoepidural anesthesia from 4 hours to 5 hours | 30 000 |
| B01.003.004.009 | 37.1.5.1 | Total intravenous anesthesia from 1 hour to 2 hours | 20 000 |
| B01.003.004.009 | 37.1.5.2 | Total intravenous anesthesia from 2 hours to 3 hours | 24 000 |
| B01.003.004.010 | 37.1.9.1 | Endotracheal anesthesia from 6 to 7 hours | 65 000 |
| B01.003.004.010 | 37.1.9.2 | Endotracheal anesthesia from 7 to 8 hours | 70 000 |
| B01.003.004.002 | 37.1.15.1 | Conduction anesthesia of the 2nd category of complexity | 5 000 |
| B01.003.004.002 | 37.1.15.2 | Conduction anesthesia of the 3rd category of complexity | 6 000 |
General hospital services
| Service code | Internal code | Name | Price, rub |
| S01.001.001 | 37.0.1 | Stay in a hospital ward (daily) | 6 000 |
| S01.001.002 | 37.0.2 | Stay in a hospital ward (daytime until 21:00) | 3 000 |
| S01.001.003 | 37.0.3 | Stay in the ward for accompanying persons (daily) | 6 000 |
| S01.001.004 | 37.0.4 | Stay in hospital room VIP 1 (daily) | 10 000 |
| S01.001.005 | 37.0.5 | Stay in hospital room VIP 2 (daily) | 16 000 |
| S01.001.006 | 37.0.6 | Stay in a hospital ward (daily, without meals) | 3 400 |
| S01.001.007 | 37.0.7 | Stay in the intensive care unit from 6-24 hours | 8 000 |
| B01.047.009 | 37.0.9 | Supervision by a therapeutic physician (1 visit) | 2 500 |
| A11.12.003 | 37.0.10 | Infusion therapy of expensive drugs | 4 000 |
| A23.01.001 | 37.0.11 | Extraction of surgical material using delivery means (calculated price) | 1 000 |
| A18.05.013 | 37.0.22 | Treatment using blood products (calculation, price) | 1 000 |
| A11.12.003 | 37.0.23 | Treatment using additional drug therapy (calculation, price) | 1 000 |
| A23.01.001 | 37.0.24 | Selection of implants (calculation, price) | 1 000 |
| S01.002.001 | 37.0.25 | Selection of compression garments (calculation, price) | 1 000 |
| B01.057.001 | 37.0.28 | Appointment with an operating specialist | 0 |
| A11.01.014 | 37.0.29 | Hemostasis using local hemostatic agent Zhelplastan 2.5 g | 6 600 |
| A11.01.014 | 37.0.30 | Hemostasis using local hemostatic agent Zhelplastan 5.0 g | 12 700 |
| A11.12.003.002 | 37.0.31 | IV drip infusion of Ferinject 500 mg (Ferinject, 50 mg/ml, 2 ml No. 5 in ampoules or 50 mg/ml, 10 ml in a bottle), duration up to 30 minutes | 8 000 |
| А11.12.003.003 | 37.0.32 | IV drip infusion of Ferinject 1000 mg (Ferinject, 50 mg/ml, 10 ml in bottle No. 2), duration up to 30 minutes | 15 000 |
| S01.001.008 | 37.0.1.1 | Stay in a hospital room (overnight) | 3 000 |
| S01.001.009 | 37.0.4.1 | Stay in hospital room VIP 1 (no more than 12 hours) | 5 000 |
| S01.001.010 | 37.0.5.1 | Stay in hospital room VIP 2 (no more than 12 hours) | 8 000 |
Scar removal
| Service code | Internal code | Name | Price, rub |
| A16.01.022.001 | 37.24.1 | Correction of scars up to 5 cm with local plastic surgery, category 1, complexity | 2 000 |
| A16.01.022.001 | 37.24.2 | Correction of scars up to 5 cm with local plastic surgery, category 2, complexity | 5 000 |
| A16.01.022.001 | 37.24.3 | Correction of scars up to 5 cm with local plastic surgery, category 3, complexity | 10 000 |
| A16.01.023 | 37.24.4 | Elimination of skin scars up to 10 cm with local plastic surgery (1 cat) | 15 000 |
| A16.01.023 | 37.24.5 | Elimination of skin scars up to 10 cm with local plastic surgery (2 categories) | 25 000 |
| A16.01.023 | 37.24.6 | Elimination of skin scars up to 10 cm with local plastic surgery (3 categories) | 35 000 |
| A16.01.023 | 37.24.7 | Elimination of skin scars 10-20 cm with local plastic surgery (1 cat) | 20 000 |
| A16.01.023 | 37.24.8 | Elimination of skin scars 10-20 cm with local plastic surgery (2 cat) | 30 000 |
| A16.01.023 | 37.24.9 | Elimination of skin scars 10-20 cm with local plastic surgery (3 cat) | 40 000 |
| A16.01.023 | 37.24.10 | Elimination of skin scars over 20 cm with local plastic surgery (1 cat) | 30 000 |
| A16.01.023 | 37.24.11 | Elimination of skin scars over 20 cm with local plastic surgery (2 categories) | 45 000 |
| A16.01.023 | 37.24.12 | Elimination of skin scars over 20 cm with local plastic surgery (3 categories) | 60 000 |
| A16.01.023 | 37.24.13 | Excision of scar with autotransplantation of tissue (1 category) | 100 000 |
| A16.01.023 | 37.24.14 | Excision of scar with autotransplantation of tissue (2 categories) | 150 000 |
| A16.01.023 | 37.24.15 | Scar excision with tissue autotransplantation (category 3) | 200 000 |
| A16.01.023 | 37.24.16 | Elimination of skin scars - I category of complexity | 65 000 |
| A16.01.023 | 37.24.17 | Elimination of skin scars - II category of complexity | 100 000 |
| A16.01.023 | 37.24.18 | Elimination of skin scars - III category of complexity | 200 000 |
| A16.12.038.004 | 37.24.19 | Autotransplantation of the flap - I category of complexity | 150 000 |
| A16.12.038.004 | 37.24.20 | Autotransplantation of the flap - II category of complexity | 200 000 |
| A16.12.038.004 | 37.24.21 | Autotransplantation of the flap - III category of complexity | 250 000 |
How the treatment method works
The patient is placed on the operating table so that good access to the wound is provided. After treating the surgical field and covering the surgical area with sterile sheets, surgical treatment of the trophic ulcer or wound is performed. During this treatment, all remaining necrotic tissue areas are removed and pinpoint bleeding from the granulations is ensured.
After this, a split skin flap is harvested. A saline solution is injected into the thickness of the skin, which lifts the skin itself and facilitates its separation. After creating such a “water cushion,” the flap is harvested using a special instrument—an electrodermotome. This is a special circular knife that is adjusted to a certain thickness of the required flap. After this, the razor of this dermatome removes the thinnest skin flap of the required size.
To increase the area of the skin flap, it is passed through a special instrument - a perforator. A puncher makes small incisions in the flap in a checkerboard pattern. Now the flap, when stretched, can cover an area several times larger than its original size.
After perforation, the flap is placed on the wound surface and modeled according to the shape of the wound. For the purpose of fixation, it is sutured with the finest sutures to the edges of the wound and pressed with a pressure bandage.
The donor site is covered with a kennel bandage with an antiseptic.
What is "Stratagraft"
StrataGraft, the equivalent of healthy human skin tissue, is a bioengineered allogeneic cellular structure (BACC) developed for the treatment of severe burns.
“Stratagraft”, which actually replicates the structure of natural skin, is assembled from two layers: an internal one, similar to the dermis, and an external one, similar to the epidermis.
The Stratagraft design includes normal human dermal fibroblasts and fully stratified (multilayered) biologically active epidermis derived from the NIKS cell line, an immortalized, genetically stable, non-tumorigenic and pathogen-free keratinocyte progenitor cell line isolated from infant tissue. Both layers are encased in collagen gel.
Metabolically active cells in Stratagraft produce and secrete various growth factors and cytokines. They, as well as extracellular matrix proteins, are involved in wound repair and regeneration. The Stratagraft provides a strong primary barrier function through the stratum corneum, a key component of the fully stratified epithelial layer, and can be connected and secured to the wound bed using adhesives, staples or sutures.
"Stratagraft", devoid of acute immunogenicity, does not cause rejection and does not lead to immune responses against NIKS.
Mallinckrodt took over the Stratagraft project after purchasing its originator, Stratatech, in August 2016. The development was carried out with financial assistance from the US Biomedical Advanced Research and Development Authority (BARDA), which, as of the fall of 2022, had invested $100 million of the planned $261 million in the project.
"Mosmedpreparaty"
Possible complications during treatment
It is advisable to do the first dressing after transplanting the flap 2-3 days after the operation. During this time, most of the flap adheres to the granulation tissue and does not come off when changing the dressing. In any case, the dressing must be changed very carefully, removing it layer by layer using a tool.
During dressing, the transplanted flap is fixed to the granulations, and pieces of skin that are not stuck are removed. If a local infection is noted, a culture is taken and bandages with antiseptics are used.
The donor wound does not need to be opened if there are no signs of infection. It is enough to change the bandage on top. Over time, the skin will epithelialize and the bandage will come off on its own. Usually 14 - 21 days after surgery.
general information
Surgery involving skin grafting is called dermatoplasty. The operation is prescribed for the treatment of burns and large-area wounds for victims of any age, as well as in a number of other cases:
- burns;
- wounds, including after surgery;
- diabetic foot, accompanied by ulcerative defects that do not respond well to conservative treatment methods;
- operations related to limb defects, as well as elephantiasis.
Skin grafting is contraindicated at elevated temperatures, wound infection and in the presence of decompensation of somatic diseases. Material for skin grafting can be taken from 3 sources:
- skin of the patient or donor;
- animal skin, after special preparation;
- artificial materials from biological polymers and cell coatings.
The material is selected based on clinical indications and its availability. According to the classification of dermatoplasty operations, the following types of surgical intervention are distinguished:
- autodermoplasty;
- allodermoplasty;
- application of cellular products.
Involves using the patient's own skin. It is carried out if skin defects occupy no more than 35–50% of the entire body. A thin layer of skin is cut off from a healthy part of the back or leg and transplanted onto the injured area.
In this method, the rehabilitation process is especially complex. According to studies, after autodermoplasty repairs, up to 10% of first-degree burns, 55 to 62% of second-degree burns, and 30 to 40% of third-degree burns develop keloid and hypertrophic scars.
They are the most problematic and sensitive of possible scars, because in the process of development they cause inconvenience to a person: they aesthetically spoil the appearance, cause itching, redness, and increased temperature at the site of injury. And a hypertrophic scar also grows in size over time, capturing healthy areas of the skin.
It is prescribed if damaged skin makes up more than 50% of the entire body or if there are contraindications to autodermoplasty. In this case, donor, animal or synthetic skin is used.
It is carried out in a few medical centers with large scientific departments. For the operation, biological material taken from the patient himself is used.
Based on the timing and rehabilitation, dermatoplasty is divided into primary and secondary. The primary one is carried out during the patient’s hospitalization, without waiting for regenerative processes in the dermis. A secondary transplant is carried out a week later, when granulation tissue from immature connective tissue begins to form.
In addition, in surgery there are concepts of free and non-free skin grafting . In the first case, the flap of skin is completely transferred to the surface of the wound, and in the second, the skin area has a nourishing pedicle, which provides a better healing effect.
In case of severe burns and a large area of damage, it is necessary to contact a combustiologist. This physician treats complex injuries and works closely with radiologist, anesthesiologist, transplant surgeon and other specialists.
Combustiologists use the following working methods:
- Treatment under a bandage . The burn is treated with an antiseptic and prescribed medications, and a bandage is applied. Bandages must be sterile, and be sure to change them every specified period of time.
- Therapy in a bacteria-free environment . A victim with open burns is placed in a special sterile box. This method is used in cases where it is impossible to apply a bandage either due to large areas of the wound or its difficult accessibility (perineum, face).
- Necroectomy and eschar management . Abscesses and dead cells are removed through surgery.
- Skin grafting . It is considered to be the final stage of therapy. It is carried out on large affected areas when natural cell regeneration is impossible.
The surgical expert knows dozens of skin grafting operations. However, in all cases, the operated part of the body must be carefully cared for to avoid the occurrence of a wound after skin grafting.
Find out which method of correcting scars and stretch marks is optimal for you!
doctor Svetlana Viktorovna Ogorodnikova.
doctor
Prognosis after treatment method
If the operation is carried out according to indications, provided that the causes of necrosis and trophic ulcers are eliminated, then the results of skin grafting are very good. Correctly performed surgery is successful in 95% of cases. In the postoperative period, the transplanted skin is gradually replaced by its own epidermis, which is manifested in the appearance of small crusts, under which young skin is noticeable.
Autodermoplasty may be a definitive method of wound closure if the wound is not on a supporting surface or in the area of a large joint. In such places, young skin can be damaged under stress with the formation of trophic ulcers. For supporting and bone surfaces, it is better to use full-thickness skin grafting with flaps on a vascular pedicle.
Main indications and contraindications
Indications for transplantation include the following conditions:
- burns and other thermal damage to the skin;
- traumatic wounds;
- defects after surgical removal of scar formations, tumors, etc.;
- diabetic foot, accompanied by ulcerative defects that are difficult to treat with conservative methods;
- operations for the treatment of malformations of the arms and legs, as well as elephantiasis.
Skin grafting is the “gold standard” for the treatment of burn injuries. Timely skin grafting or the use of artificial wound covering can prevent wound infection, plasma loss, and also improve long-term treatment results.
Surgical interventions are contraindicated in cases where the patient has decompensated somatic diseases, fever or wound infection. The operation is postponed until these conditions are eliminated.
Observation program after treatment method
The operating surgeon must observe the patient until the trophic ulcer or wound to which the skin was transplanted is completely epithelialized.
In the postoperative period, medications may be prescribed that reduce the process of scarring of the skin in the plastic area. These ointments (Kontratubeks) can be rubbed into the wound for 3-6 months and contribute to the formation of a soft, delicate scar.
The final outcome of a skin transplant operation depends on the course of the vascular disease that caused the formation of a trophic ulcer or necrotic wound. Therefore, the main observation is carried out on the results of the vascular stage of treatment.
"Stratagraft": what's next
Mallinckrodt is testing Stratagraft in the Phase II clinical trial StrataSOMA (NCT04765202), testing it in more severe thermal burns involving all layers of skin down to the underlying muscle (full thickness burns - 3rd degree burns): Stratagraft is applied over an autodermal graft .
The previous phase II clinical trial NCT03005054 of treating adults with the above severe burns using Stratagraft alone did not confirm its therapeutic validity.
There are plans to test Stratagraft in the pediatric population.