This is a serious defect in plastic surgery, which is often associated with the use of low-quality implants and individual nuances of the patient’s breast anatomy, which the surgeon did not determine before the intervention began. If such a complication occurs, repeated intervention is necessary to correct the defect. Today, such a complication occurs infrequently, since experienced plastic surgeons conduct a preliminary examination of a woman, determine all the structural features of her breasts and perform operations using the most modern implants, carefully monitoring the rehabilitation process.
Reasons for the development of complications
Plastic surgeons identify a number of reasons for the development of double bubble folds. These can be complications both in the early stages after surgery (during the first two months) and late (in the period from 2 to 5 months after the intervention).
Causes of early defects:
- insufficient experience or qualifications of the operating plastic surgeon;
- choice of low quality prostheses, incorrect selection of size or shape for a particular woman;
- incorrect performance of the operation from the technical side, the wrong place for placing the implants was chosen;
- during the intervention, part of the fat layer was removed in the area of the submammary fold, where a cavity was subsequently formed into which the implant was lowered;
- the skin on the chest and chest is elastic and thin, while the fold area under the breast is quite convex;
- before plastic surgery, the woman had a pronounced asymmetry of the folds under the breast, which was not taken into account in advance by the surgeon when choosing tactics and the type of endoprostheses;
- the woman did not follow the recommendations during the rehabilitation period (refused to wear shapewear, slept on her stomach, started physical activity early).
In the later period, the development of such a complication is due to:
- slipping of the implant from its place due to various circumstances, which causes a “waterfall effect” with the nipple and areola of the breast lowering below the normal line with their deformation;
- displacement of the implant below the fold under the breast due to deformation of the prosthesis itself with its contouring under the skin;
- arbitrary migration of the implant in the pocket created by the surgeon;
- the presence of a congenital breast defect with underdevelopment of its lower pole;
- violation of the tactics of choosing a prosthesis in relation to its shape, type and size, as well as the anatomical features of the breast and surrounding tissues of the patient;
- the formation of a capsule of fibrous tissue around the prosthesis, compressing the product and displacing it downward, towards less tissue resistance.
Preparing for breast correction
The preparatory period for re-operation to correct the complication that has arisen is identical to the preparatory period for the primary breast augmentation operation.
Before breast correction, it is necessary to do an ultrasound of the mammary glands or computed tomography and undergo all the necessary clinical examinations.
To reduce the risk of complications, you must stop smoking immediately 2 weeks before and 2 weeks after surgery.
Stop taking aspirin-containing medications, as well as medications that affect blood clotting.
Which patients are at risk?
Women from certain categories who have features in the anatomy of the mammary gland are especially at risk of encountering such a complication of mammoplasty:
- Tubular-shaped breasts with a too narrow base and a large areola, an inflated location of the inframammary fold against the background of a large volume of glandular tissue in the area of the upper pole of the gland.
- The breast is cone-shaped with a gland that is much wider than the area of the nipple and areola (shaped like a pyramid).
- The folds under the bust are sharply exaggerated.
- There is a congenital and quite pronounced asymmetry of the mammary glands, which sharply increases the risk of errors during surgical intervention if the calculations and selection of implants are carried out incorrectly.
Options for correcting complications
If the bubble-double effect develops after mammoplasty, it is important to consult a doctor as soon as possible for advice. But only an experienced plastic surgeon will eliminate such a complication. In many ways, the volume and nature of the intervention depends on the severity of the deformity, the specific area of localization of the protruding implant and the individual characteristics of the patient’s breast.
It is possible to perform a repeat operation under general anesthesia and excision of deformed breast tissue, breast straightening, and formation of an inframammary fold in a new location. The doctor makes an incision, releases the compressed tissue, fixes it correctly and forms a new fold, which allows the formation of the natural shape of the gland.
Another intervention option is transfer of the submammary fold using special sutures. This intervention allows you to eliminate breast deformation after previous plastic surgery, creating ideal shapes.
Additional manipulations are also possible:
- removal of the previous implant and replacing it with a high-quality one that is correct in size and shape;
- performing capsulotomy with removal of fibrous formations around the prosthesis;
- lipofilling of the mammary gland with the transplantation of one's own adipose tissue from one zone to the area of the mammary gland to give the desired volume and correct shape of the gland.
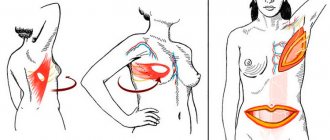
Lipofilling is a manipulation indicated for a slightly pronounced double-bubble effect. By injecting fatty tissue into the right places, the problem can be corrected. Fat is taken from the back and abdomen, thighs or riding breeches; it does not lead to tissue rejection and is safe when used correctly. It allows you to correct the asymmetry of the glands and create more ideal forms, but the effect does not last so long, so courses need to be repeated.
In Russia, we call this phenomenon of operated mammary glands a double fold; Western surgeons call this offensive situation that occurs after breast prosthetics a “double bubble” or “double bubble.” The terms are different, but the situation is the same... We will use both of these terms in the article, using the abbreviation “D-B”.
The main reason for the appearance of a double fold is restrictive, that is, a shortened, reduced or underdeveloped lower pole of the mammary glands, when the main part of the glandular tissue is concentrated on top of the mammary gland (in its upper pole). Most often these are tubular, cone-shaped breasts and “well-formed” mammary glands, but with exaggerated inframammary folds (Fig. 1).
Rice. 1:
1a - tubular mammary glands;
1b - cone-shaped mammary glands;
1c — combination of cone-shaped (left) and tubular (right) deformation of the mammary glands in the same patient;
1d - correctly formed mammary gland with an elevated inframammary fold.
In order to correct this deficiency during mammoplasty, it is necessary to supplement the missing lower pole of the gland with an implant. In this case, the surgeon is forced to artificially form the inframammary fold much lower than the natural one.
But first, a little anatomy (Fig. 2). The mammary gland is located on the chest wall and has the following landmarks relative to the ribs. The origin (upper pole) is located at the level of the II-III rib. The nipple and areola are located at the level of the V-VI ribs. The inframammary fold is at the level of the VII-VIII ribs. The tissues involved in the formation of this organ are the following (from the surface inwards):
1) Leather;
2) Subcutaneous fat;
3) Superficial fascia with a network of Cooper's ligaments, which is woven into the gland;
4) Mammary gland;
5) Fascia of the pectoral muscles;
6) Pectoral muscles;
7) Ribs.
All structures are involved in the formation of the inframammary fold. Basically the Cooper's ligamentous apparatus, in which all the glandular tissue is suspended like in a hammock. It is these ligaments, coming almost from the skin and intertwining with the fascia of the pectoral muscles, perforating the glandular tissue, that form the inframammary fold. Naturally, such a complex structure is difficult to separate. D-B occurs when the natural inframammary fold cannot be destroyed and there are two of them: artificially formed under the implant and natural. That is, there is a “conflict” between the implant and tissues. This is the reason for the formation of so-called early double folds, which become visible immediately after surgery or after the swelling has subsided. Late double folds may occur within a few months after surgery or several years later. The causes of late D-B are different, as are the timing of their occurrence. But more on that later.
Let us consider in more detail the anatomical “calculations” of early D-B, methods for their elimination and the nuances of surgical techniques that prevent their occurrence.
So, the “risk group” is tubular, cone-shaped and “normally formed” mammary glands with elevated (above the VI-VII ribs) inframammary folds.
Tubular (or tubular) are called mammary glands with an excessively narrow base and excessively large areolas in diameter, such that the dimensions in diameter of these two landmarks are almost equal (Fig. 3a). Naturally, the inframammary fold is greatly exaggerated. The lower pole of the gland is practically absent, the glandular tissue is concentrated in the upper pole and has a tube structure. When eliminating this deformation, it is necessary to strictly select the shape of the implant and be sure to adapt the gland tissue. In Fig. 3b: Reasons for the formation of a double fold during tubular breast prosthetics.
The ideal way to eliminate tubular breasts is, in our opinion, to use ultra-high-profile anatomical implants with a truncated base and opening of the distal (part of the glandular tissue under the areola) section of the tubular gland in the form of an “umbrella”. In addition, at the same time, the areola hernia is eliminated using the “purse-string” method. The glandular tissue concentrated in the upper pole finds its place in the upper part of the truncated implant and easily fits into its slope, without subsequently forming a protrusion (Fig. 3c).
This is not a public offer!
There are contraindications. Before use, consultation with a specialist is required. We consider a similar approach to be the most justified in cases of eliminating cone-shaped deformation of the mammary glands. The only difference is that with a cone there is no need to eliminate the areolar hernia and reduce the diameter of the areola.
Cone-shaped is a shape in which the width of its base is 3-4 orders of magnitude greater than the distal (areolar) part of the gland, while the glandular tissue has the shape of a pyramid.
In Fig. 4: Cone-shaped breast prosthetics were performed using an ultra-high-profile anatomical implant with a truncated base.
We consider the same approach justified if, with a normally formed breast, there is a reduced lower pole with a naturally high inframammary fold, as mentioned earlier. In this case, most often only a careful selection of the implant and clear overcoming (surgical separation) of the natural fold is necessary.
In Fig. 5: Correctly formed mammary gland with a naturally elevated inframammary fold. The augmentation was carried out using an ultra-high-profile anatomical implant with a truncated base.
This is not a public offer!
There are contraindications. Before use, consultation with a specialist is required. In this situation, it is necessary to take into account the memory of the shape of the skin of the natural inframammary fold. If it retains its shape even after deep detachment, its tension is overcome by means of through perforation caused by a sharp needle.
To avoid a double fold, a combined installation of the implant is necessary, that is, the formation of a two-plane bed for it. The upper part of the implant stands under the “cut” pectoralis major muscle. (Fig. 3b; 3c). At the same time, when it is in a contracted state, there is correct pressure on the implant from top to bottom, as a result of which it is always in a straightened state and has a constant shape, which allows the formation of a normal lower pole of the gland, overcoming natural restriction.
If the implant is installed completely under the muscle, including the lower pole, then due to the work of the muscles from below, the implant is squeezed upward and the same “D-B” effect is obtained.
In Fig. 6:
Increased deformity in the form of a double fold with tension in the muscles of the chest wall. It occurs only when the implant is placed completely in the muscle bed.
The approaches described above make it possible to eliminate D-B already on the operated mammary glands. In these cases, the surgeon decides to leave the previously placed implant, if it is selected correctly, and adapt the soft tissue of the gland on it or change both (Fig. 6a, 6b, 6c).
In Fig. 6a
: Double fold after tubular breast replacement. Corrected using an ultra-high-profile anatomical implant with a truncated base, flattening the lower segment of the gland and eliminating the areolar hernia.
This is not a public offer!
There are contraindications. Before use, consultation with a specialist is required. In Fig. 6b
: Double fold after cone breast replacement (pictured on the right). Corrected using an ultra-high-profile anatomical implant with a truncated base and flattening of the lower segment of the gland.
In Fig. 6v
: Double fold after prosthetics with a round low-profile implant of normally formed mammary glands with a naturally elevated inframammary fold. Corrected using an ultra-high-profile anatomical implant with a truncated base and plastic surgery of the inframammary fold.
This is not a public offer!
There are contraindications. Before use, consultation with a specialist is required. I would like to note that this is a rather difficult task - eliminating a double fold. It is much easier to prevent this situation! As a rule, when eliminating an existing D-B, it is necessary to perform not one operation, but several minor corrections after the main operation.
The causes of late double folds are as follows:
1. Mammary fibrosis.
2. “Sliding” of the gland from the implant – the “waterfall” effect.
3. Lowering the implant below the formed fold. (Fig. 6c).
The most common situation is the occurrence of D-B due to mammary fibrosis. With it, the capsule is compressed: it compresses the implant, and the soft tissues of the gland are pulled upward, as they are fused to the anterior wall of the capsule, while the implant itself is displaced downward, displaced by these tightened tissues of the gland. In this situation, it is usually sufficient to perform a capsulotomy on the existing implant or replace it if the condition requires it.
In Fig. 7
: Mammary fibrosis on the right, an open capsulotomy was performed.
With the “waterfall effect” - the “flowing down” of the gland relative to the implant - the problem is solved in the same way as with early “D-B”, i.e., a reposition (redistribution of the lower pole) of the mammary gland is performed with the opening of its lower border and areolar ( purse-string) pexy. If the implant continues to comply with the specified configurations, then its replacement is not necessary, otherwise it is replaced with the most suitable one.
In Fig. 8
: Waterfall effect combined with double fold. Corrected by areolar mastopexy with re-prosthetics with ultra-high-profile anatomical implants.
This is not a public offer!
There are contraindications. Before use, consultation with a specialist is required. To communicate with patients who have undergone breast augmentation, lifting or reduction, come to our forum in the Mammoplasty
How to prevent the double breast effect
The most important thing for preventing such complications during mammoplasty is choosing an experienced surgeon who will take into account all the anatomical features of the breast and correctly develop surgical tactics. The experience and qualifications of the specialist are important, as well as the clinic’s equipment, implants of different types and sizes, which are individually selected for each patient.
A competent specialist will determine the future location of breast implants, the method of their installation and the area of incisions.
You first need to conduct a full examination before surgery, as well as meticulous adherence to the milestones of rehabilitation and medical recommendations.
It is also important to wear compression garments to prevent the prosthesis from drooping and to form the correct bed for it. Underwear will need to be selected together with the doctor and worn exactly as long as the doctor deems necessary.