- How common is nasal and sinus cancer?
- Risk factors for developing cancer of the nasal cavity and paranasal sinuses
- Prevention of cancer of the nasal cavity and paranasal sinuses
- Diagnosis of cancer of the nasal cavity and paranasal sinuses
- Symptoms of cancer of the nasal cavity and paranasal sinuses
- Stages (prevalence) of tumors of the nasal cavity and paranasal sinuses
- Treatment of cancer of the nasal cavity and paranasal sinuses
- Results of treatment of tumors of the nasal cavity and paranasal sinuses
- What happens after treatment is completed?
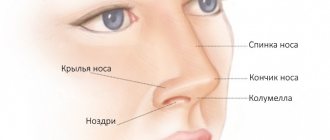
The paranasal sinuses (sinuses) are normally filled with air, but when infected they can contain mucus and pus.
The nasal cavity and paranasal sinuses are lined with a mucous membrane containing various (squamous epithelial, glandular, nerve, etc.) cells, which can become a source of the development of malignant tumors.
- Squamous cell carcinoma arises from flat epithelial cells, is the most common and accounts for 60-70% of all tumors of this localization.
- Adenocarcinoma develops from glandular cells and occurs in 10-20% of cases.
- Lymphomas arise from cells of the immune system and account for 5% of all tumors of the nasal cavity and paranasal sinuses.
- Melanoma is a malignant tumor of pigment cells, which is detected in 3% of patients.
- Esthesioneuroblastoma is a rare tumor that develops from nerve cells.
Risk factors for developing cancer of the nasal cavity and paranasal sinuses
Prolonged contact with wood and flour dust , participation in the production of textiles and leather goods increases the risk of malignant tumors of the nasal cavity and paranasal sinuses.
Other less significant risk factors include exposure to adhesives, formaldehyde, solvents used in furniture and footwear, nickel and chrome dust, isopropyl alcohol and radium.
Smoking increases the risk of developing cancer of the nasal cavity and paranasal sinuses, along with tumors of the lungs, mouth, larynx, esophagus, bladder, kidneys and other organs.
Who does BKR choose?
Basal cell skin cancer (BCS) most often affects men over 70 years of age - approximately 2 times more often than women of the same age group. However, there is no consensus on the predominance of BCC in people of different sexes - most authors believe that BCC occurs with approximately the same frequency in people of both sexes; in the samples of some authors, the predominance of BCC is indicated in either men or women. In case of BCC, a single lesion was found in different years in 94–99%, multiple lesions (from 2 to 7) – on average in 2.5% of patients in different areas of the skin [ 6
].
In the development of BCC, great importance is attached to genetic factors, the presence of xeroderma pigmentosum, immune disorders, adverse external influences - intense insolation, contact with carcinogenic substances, arsenic compounds, previous radiation therapy, increased photosensitivity, work with sources of ionizing radiation, contact with petroleum products, resins, local mechanical trauma [ 8
].
The main importance is given to excessive insolation. The greatest danger is posed by ultraviolet radiation, especially UV rays type A. A special risk group consists of people with fair skin and low melanin content (type I and II skin) [ 9
].
Symptoms of cancer of the nasal cavity and paranasal sinuses
- Long-term nasal congestion
- Pain above or below the eyes
- Unilateral obstruction of the nasal passage
- Nosebleeds
- Discharge of pus from the nasal passages
- Decreased sense of smell
- Numbness or pain in the face
- Loose teeth
- Swelling on the face, nose, or roof of the mouth
- Constant watery eyes
- Unilateral bulging eyes or blurred vision
- Pain or pressure in the ears
- Difficulty opening the mouth
- Enlarged cervical lymph nodes
Many of these symptoms can occur with other conditions, such as an infection in the nasal cavity or paranasal sinuses.
However, only a doctor can confirm or exclude the diagnosis of a tumor. In addition, you need to remember that the earlier a tumor is detected, the higher the likelihood of successful treatment.
After examination by a medical specialist and preliminary examination, additional research methods may be recommended.
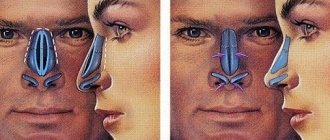
X-ray examination of the paranasal sinuses allows us to judge the condition of the sinuses, identify an inflammatory or tumor process in the sinuses and nearby lymph nodes, and prescribe additional examination.
Computed tomography (CT), in some cases with additional contrast, is an effective method for diagnosing tumors in these locations.
Magnetic resonance imaging (MRI) can provide additional information and can distinguish a malignant tumor from a benign process.
A biopsy (taking a piece of the tumor for microscopic examination) is a mandatory final examination method, which makes it possible to make a final diagnosis and justify the planned treatment tactics for the patient.
The uniform can be not only military
Basaliomas can be multiple. Primary – multiple form of BCC, according to K.V. Daniel - Beck and A.A. Kolobyakova (1979) [ 10
], occurs in 10% of cases, the number of tumor foci can reach several dozen or more, which may be a manifestation of non-basocellular Gorlin-Goltz syndrome.
The cardinal symptom is the appearance in the early period of life of multiple basal cell carcinomas, accompanied by odontogenic cysts of the jaws and anomalies of the ribs [ 11
].
The following forms of BCC are distinguished: nodular-ulcerative (ulcus rodens), superficial, scleroderma-like (morphea type), pigmentary and fibroepithelial. Histologically, BCC is divided into undifferentiated and differentiated types [ 2
].
Currently, various methods of treating BCC are used, which include: surgical excision, laser therapy, photodynamic therapy, cryodestruction, radiation therapy, electrocoagulation, as well as the administration of prospidin followed by cryodestruction, intralesional injection with intron A, the use of spirobromine and leukinferon, radio wave surgery. The goal of all treatment methods is to remove the tumor with minimal damage to nearby tissues, achieve a good cosmetic effect, reduce postoperative complications and the number of possible relapses of the disease. However, none of the listed treatment methods prevents the development of relapses [ 14, 15, 16, 17, 18
].
Treatment of cancer of the nasal cavity and paranasal sinuses
Surgery
The extent of surgical intervention depends on the extent of the tumor process and may consist not only of removing the tumor within healthy tissue, but also excision of lymph nodes in the neck.
The anatomy of the nasal cavity and paranasal sinuses is very complex because the most important nerves, blood vessels and other structures are located near this area.
The proximity of the brain, eyes, mouth and carotid arteries, which provide nutrition to the brain, greatly complicates the performance of operations.
In this case, it is necessary to take into account the appearance of the face and the subsequent ability to breathe, speak, chew and swallow.
Unfortunately, in some cases, by the time of diagnosis, the tumor may have spread to the orbital area. In this situation, during surgery, not only the main tumor is removed, but also the eye and orbital tissue.
For nasal cavity cancer, a wide excision of the lesion within healthy tissue is performed.
This may require partial or complete removal of the nasal septum. If the outer part of the nose is affected, it may be necessary to partially or even completely remove the nose and then reconstruct it from the surrounding tissue. In addition, there are now cosmetic prosthetic noses made from artificial materials.
For tumors of the paranasal sinuses, extended surgical interventions are possible with the removal of bone tissue of the face, jaw, and orbit.
Endoscopic operations are performed using special telescopic instruments for small tumors or for palliative purposes, when the patient for some reason cannot undergo complex extended surgery. Typically, such operations are combined with subsequent radiation therapy.
Cancer of the nasal cavity and paranasal sinuses sometimes metastasizes to nearby lymph nodes.
For this reason, depending on the extent of the process, removal of several or all affected lymph nodes is performed.
In patients with cancer of the nasal cavity and paranasal sinuses, radiation therapy can be used either as an independent method or as an addition to surgery.
Radiation therapy as an independent method may be recommended for patients with small tumors. In this case, a complete cure is possible while maintaining good cosmetic results.
Radiation may be used in patients with poor general condition who cannot undergo complex surgery.
If the main tumor is not completely removed, radiation therapy is prescribed to destroy the remaining tumor cells. Radiation can be effective if used for palliative purposes to stop pain, bleeding, improve swallowing function, and also for cancer metastases to the brain.
Temporary side effects of radiation therapy include skin damage, loss of appetite, decreased taste, sore throat, hoarseness, difficulty swallowing, and increased fatigue.
These phenomena resolve on their own soon after cessation of irradiation.
Radiation therapy can cause blurred vision, dry mouth due to damage to the salivary glands, bone damage, and dysfunction of the thyroid gland.
The most commonly used antitumor drugs in patients with cancer of the nasal cavity and paranasal sinuses are: 5-fluorouracil, bleomycin, cyclophosphamide, vinblastine and methotrexate.
The drugs can be used individually or in combination.
Chemotherapy kills tumor cells, but can also damage normal cells, leading to side effects and complications, including nausea, vomiting, loss of appetite, baldness, mouth ulcers, increased susceptibility to infection, and bleeding.
After stopping treatment, most side effects go away.
Where is cancer hiding?
Basal cell skin cancer (BCS), according to the WHO classification, or basal cell carcinoma, is the most common skin tumor of varied structure, consisting of small cells resembling the cells of the basal layer of the epidermis. In terms of its prevalence among tumor diseases, BCC ranks third after stomach and lung cancer [ 1
]. Among malignant epithelial skin tumors, the incidence of BCC ranges from 45 to 90% of cases [
2
].
BCC is characterized by locally destructive growth and practically does not metastasize [ 3
].
This is usually seen in the metatypical type of BCC. In world practice, only about 200 cases of BCC metastasis have been registered [ 4
].
BCC is predominantly localized in open areas of the body – on the scalp and neck in 80–98% of cases. The most typical localization of BCC is the skin of the parietal region, where BCC occurs in 5.5% of cases, the skin of the forehead in 20%, the skin of the back, wings of the nose, brow ridges, ears, infraorbital region - in 69%, the skin of the lips, chin, cheeks – in 5.5% [ 5
]. BCC also occurs on other areas of the skin: in previously untreated patients - on the skin of the head and neck in 75.5% of cases, the skin of the chest in 3.1%, the skin of the back in 5.3%, the skin of the upper extremities in 8%, skin of the lower extremities in 8.1% (Fig. 1-11).
| Rice. 1 BKR of the skin of the right wing of the nose. | Rice. 2 BKR skin of the back of the nose, lips |
| Rice. 3 BKR of the skin of the right wing of the nose. | Rice. 4 BKR breast skin |
| Rice. 5 BCC of the skin of the right subclavian region. | Rice. 6 BKR of the scalp |
| Rice. 7 BKR of the skin of the left shoulder. |
What happens after treatment is completed?
After cessation of special treatment, the patient should be under the supervision of doctors and periodically undergo examinations in order to identify and treat complications, as well as early diagnosis of a possible relapse (return) of the disease.
If you smoked and/or drank alcohol, you need to quit these bad habits. This will help improve your condition faster and contribute to a speedy recovery.
If necessary, a nutritionist will help you choose the right diet, taking into account the surgery, radiation and chemotherapy you have undergone, and doctors of other specialties will do everything possible to restore your lost functions of speech, swallowing, chewing, etc.
Literature
- Paches A.I. Tumors of the head and neck. M., Medicine, 1983
- Apatenko A.K. Epithelial tumors and skin malformations. M., Medicine, 1973.
- Kraevsky N. A., Smolyannikov A. V., Sarkisov D. S. Pathological diagnosis of human tumors. Help Guide. M., Medicine, 1982.
- Malignant skin tumors. Edited by Anthony JJ Emmett, Michael GE O,Rourke. Churchill Livingstone 1991.
- Atlas of cancer of the skin. Edited by Gunter Burg, MD. Churchill Livingstone, 2000.
- Denisov L. E., Kurdina M. Ipotekaev., N. S., Volodin V. D. Active detection of malignant neoplasms of the skin. Moscow, 1995.
- Basal cell carcinoma in chronic arsenicism occurring in Queensland, Australia, after ingestion of asthma medication. Waranya Boonchai, MD, Adele Green, MBBS, PhD, Jack Ng, PhD, Anthony Dicker, MBBS, and Georgia Chenevix – Trench, PhD Brisbane, Queensland, Australia. Journal of the American Academy of Dermatology, October 2000, volume 43, number 4.
- Basal Cell Carcinoma. Dermatology, O. Braun-Falco, G. Plewig, HH Wolff, RK Winkelmann. Springer-Verlag Berlin Heidelberg 1991.
- Daniel - Bek K.V., Kolobyakov A.A. Malignant tumors of the skin and soft tissues. M., Medicine, 1979.
- Berenbein B. A., Lezvinskaya E. M., Krasnoshchekova N. Yu., Ilyinskaya T. B. Gorlin-Goltz syndrome. Vestn. dermatology. 1993, no. 5, p. 63 – 67.
- Vavilov A. M. Skin tumors. Russian Medical Journal, vol. 9, no. 3 - 4, 2001.
- Novikova Z. I. The effectiveness of laser surgery for basal cell carcinomas. Bulletin of postgraduate medical education. Special issue. Moscow 1999
- Sukhova T. E., Tretyakova E. I., Khlebnikova A. N., Belova N. I. Experience in the treatment of primary and recurrent basal cell carcinoma in the Moscow region. Moscow Scientific Research Clinical Institute named after. M. F. Vladimirsky. Scientific and practical conference: Current issues in the treatment of sexually transmitted infections and chronic dermatoses. Abstracts of scientific works. Ekaterinburg 2002
- Dubensky V.V., Redko R.V., Garmonov A.A. Skin neoplasms in the practice of a dermatovenerologist. Tver, publishing house "Triad", 2002.
- Kozlov V.I., Terman O.A., Stranadko E.F. Hemocirculation in basal cell carcinoma during photodynamic therapy. Scientific and practical journal Laser Medicine, volume 1, issue 2, 1998.
- Zakiya Yassin. Clinical features of skin basal cell carcinoma and pathogenetic rationale for therapy with argon laser and immunocorrective drugs (T-activin and sodium nucleinate). Dissertation for the degree of Candidate of Medical Sciences, 1991.