Sensitivity is not a type, but a property. Both oily, combination, and dry skin can acquire it for some external or internal reasons. Care for sensitive skin should be tailored to the current condition: the presence of redness or rashes, dehydration or soreness. How to choose cosmetics to care for sensitive skin? Let's figure it out.
Sensitivity can be expressed in different ways: some experience redness, some have microdamage and peeling, others are bothered by itching and a burning sensation - there are many options! It is important to remember that in most cases, sensitivity is temporary and can be corrected with care.
What skin is considered sensitive?
Sensitive skin is one that reacts too sharply to environmental factors: cold, wind, certain components of cosmetics or food. Often such skin has a damaged epidermal barrier. At the slightest contact with an irritant, a reaction appears: redness, peeling, itching and rash. Sensitive skin is no longer a type, but a condition, and both dry and oily skin can be sensitive, especially if it is burdened with acne. Whatever your skin is, it needs special care both outside and inside.
Clinical researches
The effectiveness, safety and tolerability of La-Cri products have been clinically proven. The products are recommended by the Union of Pediatricians of Russia. During clinical studies, specialists were able to record impressive results.
Cleansing gel “La-Cri”:
- gently cleanses the skin;
- relieves redness and itching;
- restores and nourishes the skin.
Sources:
- Churolinov Petr, Herbal medicine in dermatology and cosmetics, Medicine and Physical Education, 1979.
- Reken Martin, Schaller Martin, Sattler Elke, Burgdorf Walter, Atlas of Dermatology, MEDpress-inform, 2022.
- Chapman M. Shane, Habiff Thomas P., Zug Catherine A., Dinoulos James G. H., Campbell James L., Dermatology. Handbook of differential diagnosis, MEDpress-inform, 2014.
Care for sensitive skin
Cleansing
The most important stage of facial skin care is cleansing. Contaminants that accumulate on the surface of the skin during the day can block the ducts of the sebaceous glands and provoke inflammation. Free radicals, together with UV rays, form oxidative stress in the skin. Therefore, it is necessary to regularly remove obvious dirt, city dust, makeup residues and excess sebum from the skin of the face, and this must be done carefully, without damaging its protective hydrolipidic mantle. To cleanse your skin, use micellar water, foam or soft milk. For example, Micellar Water Cream Effect from Black Pearl will help you remove makeup without unnecessary rubbing.
Night face cream 36+
50 ml
Completes the cleansing procedure and prepares the skin for further care. Caring comfort tonic for dry and sensitive skin from Black Pearl. When cleansing your facial skin, you should massage it not with a hard sponge, but with cotton pads, a konjac sponge or fingertips. Use warm water, as extremely cold or hot water can cause irritation.
Day face cream 36+
50 ml
After washing, pat your face dry with a towel and apply moisturizer.
Try Day Face Cream for Dry and Sensitive Skin Nourishment from Black Pearl. Protection
To create a feeling of comfort on your facial skin during the day, use thermal water, it will relieve the feeling of tingling and dryness.
How to care for your skin from the inside?
Glowing, healthy skin starts with focusing on the overall well-being of the body. Watch your diet, avoid fast food, fatty and spicy foods, eat more fruits and vegetables and drink enough water daily. After consulting with a specialist, try using various dietary supplements, be it collagen or hyaluronic acid.
Causes
As we know, there are four types of facial skin: normal, oily, dry and combination. If the skin reacts violently to any external manifestations and irritants, then they often speak of a sensitive type. The reasons why the skin has become sensitive may lie in damage to the epidermal barrier. In other words, if the skin on your face suddenly begins to react more sharply to external or internal stimuli, then it’s time to think about what could serve as a catalyst for change. Cold wind in the off-season, frost and cold in winter, scorching summer heat, and just a banal reaction of the body to new beauty products and now we are in a hurry to ring the bells and sound the alarm. However, you should not immediately fall into hypochondria and make an appointment at the nearest aesthetic medicine clinic, as soon as you feel a slight tingling sensation and see a crimson blush on your face.
Interesting!
According to some surveys, approximately 2/3 of European women complain of increased sensitivity of facial skin.
Recommendations for choosing products for sensitive skin
When choosing a product, be sure to consider your skin type and time of year. Eliminate peelings and scrubs from your skincare routine that contain rough, irregularly shaped abrasive particles that can aggravate the condition of already reactive skin. Instead, give preference to delicate cleansing and soothing masks. During the cold season, sensitive skin may need increased support and protection from weather factors - the care cream may become thicker and richer, or you can try applying your usual care in 2 layers.
2356
rate the material
Sensitive skin can be defined as skin with erythema and/or abnormal tingling, burning, tingling (occasionally pain or itching) in response to various factors, which may be physical (UV radiation, heat, cold and wind), chemical (cosmetics , soaps, water and pollutants) and sometimes psychological (stress) or hormonal (menstrual cycle) nature. Diagnosis, pathophysiology, epidemiology and treatment are still under debate. Sensitive skin occurs most often due to neurogenic inflammation following excessive activation of sensory proteins in keratinocytes and nerve endings. Skin sensitivity is a very common condition due to the fact that it can be detected in approximately half of the population. Treatment is primarily caution when using cosmetics or using cosmetics without preservatives and surfactants or containing inhibitors of neurogenic inflammation.
Introduction
The term “sensitive skin” is in most cases used to describe many unpleasant sensations of varying intensity and transient in nature. Although the presence of sensitive skin has been debated in the past, it is now accepted that sensitive skin can be identified clinically as the presence of abnormal tingling, burning, pain, itching or stinging in response to various factors that may be physical (UV radiation, heat, cold and wind), chemical (cosmetics, soaps, water and pollutants) and sometimes psychological (stress) or hormonal (menstrual cycle) nature. Erythema is an irregular symptom, but can often take place among the complaints. Despite this, from the moment this syndrome was identified to the present day, its single, consensus definition is still missing.
Sensitive skin is also known as reactive or over-reactive skin, intolerant skin or irritable skin. The term "reactive skin" seems to be preferable to "sensitive skin", which can be confused with sensitized skin in allergic diseases. Although the pathophysiology of sensitive skin remains unclear, the underlying mechanism is not immune or allergic.
Tests that can help make the diagnosis include the prick test, the heat temperature sensitivity test, and the capsaicin test. However, diagnosis depends on history, which is obviously a more reliable method, demonstrating, as defined by the syndrome, skin sensitivity in response to various factors.
Classifications
A number of classifications have been proposed but have not received general acceptance. Yokota et al. proposed a classification of 3 different types based on physiological parameters:
Type 1: group with low barrier function of the patient's skin, transdermal water loss and abnormal desquamation.
Type 2: inflammatory group with normal barrier function and inflammatory changes.
Type 3: neurosensitive group with normal barrier function and no inflammatory changes.
Mills and Berger proposed dividing sensitive skin into 4 groups, according to dermatological background:
Group 1: people with chronic skin disorders.
Group 2: Similar visible dermatologic disease as Group 1, but symptoms are minimal or atypical.
Group 3: normal people who have had significant trauma in the past, such as sunburn or contact allergies; many years later, the injured areas will be unusually tender but appear unchanged.
Group 4: People who do not fit into any of the previous categories but report abnormal sensitivity to topical agents without visible skin changes.
Willis and de Lacharrière divided sensitive skin into 3 subgroups, according to trigger factors:
- severely sensitive skin: very high skin reactivity to all types of factors;
— skin sensitivity to topical factors;
- skin sensitivity to environmental factors.
Instead, according to severity, I propose a classification into 4 groups:
- very sensitive skin
- sensitive skin
- slightly sensitive skin
- insensitive skin
Pathophysiology
Histological examination rarely demonstrates vasodilatation with an inflammatory infiltrate. In general, there are no histological abnormalities. The usual absence of infiltration indicates that in this case the innate or acquired immune response does not play any role. Skin sensitivity is most commonly reported by patients with atopic dermatitis or other allergic conditions, but most patients with sensitive skin do not have atopy.
The barrier function of the skin, damaged in some patients, leads to transdermal water loss, which may facilitate contact with trigger factors. However, damaged barrier function is not found in all people with sensitive skin. It is assumed that sensitive skin and dry skin are different phenomena, because... No association was found to suggest that dry skin and damage to the skin barrier could contribute to skin sensitivity by facilitating contact with trigger factors. On the contrary, skin sensitivity can contribute to dry skin. Dry skin and skin sensitivity may also be the result of a similar pathogenetic mechanism, in the case of a combination of both conditions. Regular use of moisturizers is believed to improve skin sensitivity.
Abnormal sensitivity and vasodilation reflect involvement of the cutaneous nervous system. Neurotransmitters such as substance P, calcitonin gene-related peptide, and vasoactive interstitial peptide can cause neurogenic inflammation with vasodilation and mast cell degranulation. Neurogenic inflammation is determined by the release of neuropeptides (nerve endings) that cause inflammation.
The fascinating and mysterious aspect of sensitive skin is that the triggering of the pathological process is due to very diverse factors. Although it has never been demonstrated, the role of transient receptor potential (TRP) channels in cutaneous sensitivity is clear. Sensitive skin is characterized by a response to numerous factors, which can be physical and/or chemical, and TRP channels are the only molecules that can be activated by these individual factors. Abnormal or excessive activation of TRP channels seems highly likely. In the skin, TRP channels are expressed on nerve endings, Merkel cells, and keratinocytes. TRPV1 is activated by capsacin, phorbol esters, heat, and hydrogen ions; TRPV3 – heat and camphor; TRPV4 – heat, mechanical stress, hypoosmotic stress and phorbol ester derivatives. Cold and menthol activate TRPM8. TRPA1 is activated by cold, wasabi, mustard, horseradish and bradykinin. TRP channels are best activated by other substances found in cosmetics. Activation of TRP channels is accompanied by the flow of calcium ions into the cell and then depolarization. Interestingly, activation of TRPV4 on keratinocytes causes damage to the skin barrier.
In summary, it is hypothesized that epidermal TPR channels are overstimulated or overexpressed by various factors in sensitive skin. Consequently, this leads to the release of neurotropins and neurotransmitters, which cause neurogenic inflammation of the skin.
Skin explants are convenient models for dermatological studies. Explants together with neurons can be a very interesting model for studying cutaneous sensitivity in vitro. Neurons and keratinocytes cultured together are another valuable model for in vitro studies of sensitive skin. Cells from a neuronal cell line can also be cultured with keratinocytes. In these models, neurogenic inflammation can be measured based on neuropeptide release or electrical activity. The calming effect of substances used in cosmetics can also be measured.
Functional MRI was used to evaluate the neuronal response when lactic acid was applied to the face of women with and without sensitive skin. Lactate-induced skin discomfort resulted in increased activity in the contralateral primary sensorimotor cortex and in the bilateral frontoparietal network. In patients with sensitive skin, group activity extended only to the ipsilateral primary sensorimotor cortex and the bilateral periinsular secondary somatosensory area. These findings in turn also show an increase in neural activity. These results suggest central nervous system involvement and provide insight into the role of stress in sensitive skin.
Thus, the pathophysiology of skin sensitivity remains poorly understood due to difficulties in defining and diagnosing the condition and because sensitive skin can be a heterogeneous phenomenon. Sensitive skin is an excess of physiological reactions with a key role in this of the nervous system. With sensitive skin, the skin sensitivity threshold is abnormally low.
Testing
Reproducible tests are needed to estimate the prevalence and count of sensitive skin, but unfortunately, there are no simple, reliable tests. Due to the tremendous variability in the manifestations of sensitive skin, research in this area is very difficult. Moreover, it is not clear whether a patient with a low threshold for any one stimulus is susceptible to all other stimuli.
Mariott et al. carried out an analysis of various test methods. Thus, the Frosch and Kligman tingling test consisted of applying lactic acid to the nasolabial folds, followed by a subjective assessment of the intensity of the symptoms. Previous articles suggested that this was the most appropriate method. However, Mariott et al. showed that the nasolabial test is a poor predictor of overall skin sensitivity. They tested 4 chemicals that produced different enhanced sensory effects (lactic acid, a tingling sensation; capsacin, a burning sensation; menthol, a cooling sensation; and ethanol, a mixture of burning and tingling sensations) on 58 patients. There was a large number of variations in reactivity towards the compounds tested. Increased reactivity with one compound was not predictive of increased response with the other compound. Moreover, Marriott et al. used strong skin irritants (anionic surfactants and cations) and virtually non-irritating substances such as amphoteric compounds. Although volunteers who showed a positive response to amphoteric compounds were expected to have a strong response to strong stimuli, which could indicate sensitive skin, only some subjects had a strong response to all stimuli. The results of most patients did not show a response to other chemical compounds, even if they had similar effects. Green and Schaffer demonstrated that patients accurately differentiated responses to 2 different compounds. Topical application of capsaicin has been proposed as a test of cutaneous neurosensitivity and a tool for diagnosing sensitive skin. A recent study on women identified 2 subgroups with different reactions to capsaicin: those with a low threshold of sensitivity and those with a high one. These two subgroups accurately differed in their response to the perception of sensitive skin irritation. The higher the declared sensitivity, the lower the reaction threshold.
Reviews of possible diagnostic test options for sensitive skin were presented in 3 articles. The authors suggested the temperature test, prick test, occlusive application of sodium lauryl sulfate, pruritus assessment, wash and immersion aggravation test, transdermal water loss assessment, corneometry, laser Doppler velocimetry, colorimetry, squamometry, surface corneometry, and quantitative sensory testing for diagnosing or scoring sensitive skin ( the latter method is time consuming and mostly limited to clinical studies).
Overall, it is clear that only a small subclass of individuals will respond to all stimuli on all tests. A response to just one test does not mean that these people do not suffer from sensitive skin or that they do not respond to other stimuli.
Not all tests are diagnostic tools, and some tests can be used for follow-up. Because sensitive skin is defined by abnormal sensitivity and erythema in response to various factors, the best method for diagnosis is the use of scales. Unfortunately, we lack valid questionnaires. To the best of our knowledge, only one questionnaire has been proposed at the moment: the Score d'Irritabilité Global Local (SIGL). And we proposed another questionnaire to assess the sensitivity of the scalp.
Epidemiology
Reactive skin is widespread in France, with approximately 50% of respondents (59% of women and 41% of men) reporting reactive skin. These figures vary slightly among European countries, the USA and Japan. Reactive skin is without a doubt a common cosmetic problem.
This prevalence increases in summer and a role has been suggested for UV exposure, but no association with skin phototype has been identified. Although the skin is free of rashes in most cases, reactive skin can also occur in individuals who have other skin conditions (eg, atopic dermatitis, seborrheic dermatitis, or rosacea).
Sensitive skin is more common in women than men, and the incidence increases with age. Interestingly, this is associated with increased expression of TRPV1 in the skin with age. The connection to ethnicity is controversial. 3 large epidemiological studies reported no racial differences in sensitivity. Cultural factors have been reported to be relevant in determining sensitive skin and symptoms and for lifestyle likely to contribute to some of the trigger factors. The study found that fair-skinned people with sensitive skin were significantly more likely to report changes in skin color, while African-Americans were more likely to report discomfort. Japanese women responded more intensely than German women, although there were no differences in the neurosensory innervation of their skin. Opinions have also been expressed about the role of phenotype.
Etiology
The role of internal factors in the etiology cannot be excluded, but the effects of environmental factors are included in the very definition of sensitive skin. The variety of trigger factors for skin reactivity is very large and has been described in detail in many studies, including cold, heat, sun, wind, conditioned air, pollution, cosmetics, water, dry air, stress, etc.
Stress and climatic conditions cannot be changed quickly. The impact of pollution is subject to debate due to the fact that pollution is not an acute trigger of skin reactivity, and air and water pollution is less pronounced than in previous decades.
Cosmetics are the most obvious and easily changeable factor in skin reactivity. Chronic use may contribute to the development of chronic sensitive skin and may cause an increase in frequency with age.
Anatomical places
Skin reactivity is not limited to the face alone. For example, a study found that 70% of patients reported reactive facial skin with involvement of other skin areas, including the arms (58%), scalp (36%), legs (34%), neck (27%), torso ( 23%) or back (21%). Genital involvement has probably been underestimated. Another study found 77% of people had sensitive facial skin, 61% had sensitive body skin, and 56% had sensitive genital skin.
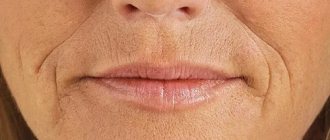
Face
The face is the most common site of sensitive skin, and the most common spontaneous complaints of sensitive skin are related to the face. The nasolabial folds are considered the most sensitive area and tests are performed in this area. These are followed by the cheekbones, chin, forehead and upper lip.
Scalp
The incidence of sensitive scalp is around 40% among French people. On the scalp, the symptoms are slightly different: itching and tingling are the most common (compared to burning and erythema of the face). Dandruff is not considered a symptom of sensitive skin. The main trigger factors are also different: heat, emotions and shampoos. No other area of skin sensitivity specifically associated with sensitivity of the scalp was identified. The sensitive scalp increases with age. A new assessment of the scalp, the 3S questionnaire distinguishes between subjects with mild sensitivity, sensitivity and severe sensitivity.
Itchy scalp is common among people with and without dandruff. The high frequency of itching of the scalp and skin sensitivity is associated with the neuroanatomical complex of the scalp, with the abundance of sensitive nerve endings of the components of the pilosebaceous complex. From a physiological point of view, the scalp can be considered as an organ with the function of class C aberrant nerve fibers.
Genital area
Cutaneous/mucosal sensitivity in this area is poorly described in men but well described in women. The role of feminine hygiene products is still controversial. It is difficult to distinguish between hyperreactivity, irritation and immunological sensitization in this area.
Differential diagnosis
In the presence of erythema, sensitive skin must be differentiated from a large number of skin diseases. But the connection with abnormal sensitivity (tingling and tingling is stronger than itching); trigger factors; and the transient nature of the erythema are strong arguments in favor of the diagnosis of sensitive skin. One of the main points of differential diagnosis is the presence or absence of a rash, which is most difficult to determine in patients with the initial form of rosacea.
In the absence of erythema, the diagnosis of sensitive skin is simple. But it must be remembered that abnormal sensitivity without any objective symptoms can also be associated with pathology of small and large nerve fibers or neuropathy due to compression of the spinal cord. Unlike sensitive skin, the anatomical distribution of symptoms in pathology of the nervous system is associated with innervation. A differential diagnosis is also made with somatoform skin diseases.
In some cases of sensitive scalp, differential diagnosis should exclude neuropathy, other causes of scalp itching, and trichodynia. Trichodynia is a painful sensation on the scalp that is localized in the area of hair loss (androgenetic alopecia, telogen effluvium, or alopecia areata).
Treatment
Treatment for sensitive skin is still under debate. There are no controlled, randomized or double-blind studies yet. It is recommended to use well-tolerated cosmetics or cosmetics with calming effects. For example, trans-4-tetra-butyl cyclohexanol (a selective TRPV1 antagonist) has recently been proposed. In general, a large number of funds were proposed. Obviously, treatment requires a comprehensive approach, which consists of stopping the use of all topical cosmetics, fragrances and sunscreens. The fewer ingredients a cosmetic contains, the better.
Expert commentary
The high frequency and complex nature of sensitive skin poses a challenge to dermatologists, who are faced with increasing demands to treat this condition. Because Symptoms of skin sensitivity are mostly subjective and transient; describing symptoms in individuals with sensitive skin is the best method of diagnosis. To conduct research on this topic, standardized questionnaires are needed that will allow calculations in a reproducible form and accessible to reflect changes in skin condition. Therapeutic approaches are debated, but reducing the use of cosmetics or using cosmetics with a soothing effect and/or minimal irritants is necessary.
Five-year perspective
All aspects regarding sensitive skin will be subject to debate, which is necessary for a consensus decision. Once this decision is made, epidemiological studies will be more accurate and studies on pathophysiology and treatment can be conducted.