Varicose veins, or varicose veins of the lower extremities, is a disease characterized by disruption of the venous valves and is caused by congenital weakness of the vascular wall, which leads to stagnation of blood in the veins of the lower extremities. Varicose veins of the lower extremities are accompanied not only by impaired blood supply and tissue nutrition, which can result in various problems in the form of congestive allergic skin irritations and the occurrence of difficult-to-heal trophic ulcers, but it is also dangerous because slow-flowing blood is prone to the formation of blood clots that can close the lumen of any vessel in the body. If the inflammatory process joins and passes to the venous wall, thrombophlebitis develops, and venous blood flow in the limb is disrupted.
People have been suffering from varicose veins of the lower extremities since ancient times. For many years, doctors wanted to alleviate the suffering of patients and tried various methods to treat this pathology. In Ancient Egypt, mummies showed signs of varicose veins and traces of burns in their place - Egyptian aesculapians used cauterization to treat varicose veins.
In Ancient Greece, Herophilus and Erasistratus described the location of human veins and presented a diagram of the entire vascular bed, and Hippocrates was the first to puncture a varicose vein and present one of the methods of conservative treatment of varicose veins of the lower extremities - local compression of the dilated vessel. Avicenna (980–1037) was the first to propose bandaging limbs for varicose veins. In India and China, at that time the most cultural and progressive centers of the world, they developed preventive exercises, the use of leeches, herbal medicines that thin the blood, contrast baths, and therapeutic nutrition.
In the 17th-19th centuries. Medical science developed rapidly, the advent of the microscope helped to study capillary blood flow and the etiology of varicose veins of the lower extremities. Her treatment began to be guided by scientifically based concepts. Since the end of the 19th century, the development of phlebology began as an independent direction in surgery. The practice of surgeons included methods of surgical treatment that are still used today. The most common intervention for varicose vein disease was the Troyanov-Trendelenburg operation, which consists of ligating the great saphenous vein in the groin; this operation was often supplemented with traumatic incisions on the legs and thighs, trying to ligate or excise damaged saphenous veins.
The principle of thermal ablation of a vein to stop blood flow in it has been used since the 50s of the 19th century. Endovasal electrocoagulation, an analogue of modern laser coagulation (EVLC), as a method of excluding varicose veins from the blood circulation, was tested and proposed for use by Czechoslovak doctors K.Firt, L.Heigal, D.Jrivora in 1959. Instead of removing the vein, they treated the inner surface of the vein with current; the burn caused by the electrode led to scarring of the vein and its ablation (gluing).
Viktor Sergeevich Savelyev played a great role in the development, determination of indications and scientific substantiation of surgical methods for the prevention of pulmonary embolism. He introduced into clinical practice modern medical procedures for the successful treatment of venous trophic ulcers and a vena cava filter to retain detached blood clots.
Get an online consultation
right now.
Get
Sclerotherapy as a method of treating varicose veins has been known since the beginning of the 20th century. This procedure is performed on an outpatient basis. The phlebologist uses a sclerosing drug to prepare foam, which is injected into the lumen of the vessel. Foam displaces blood from the vein and sticks its walls together. Over time, the sclerotic portion of the vein resolves. Compression stockings are placed on the leg and must be worn for 3-4 weeks.
As for the surgical treatment of varicose veins, phlebologists have a large number of techniques, procedures, and operations in their arsenal. In addition, modern instruments and equipment allow you to make the right decision in choosing surgical treatment, taking into account the cost of laser surgery for varicose veins.
In that version of varicose veins, when the saphenous vein is affected, it is correctly called the great saphenous vein, an operation is performed - combined phlebectomy, it is still used, and the technique for its implementation is as follows: two small incisions are made: in the groin and at the level of the ankle. A special probe is inserted into the vein, which is inserted along the entire length of the vein from the ankle to the groin, after which the vein is removed using this probe. The operation is performed in a medical center under spinal anesthesia and requires observation of the patient in the hospital for 24 hours.
Another operation is performed for tributary varicose veins; the indication for it is damage to small-diameter veins that bring blood to the main vein. In this situation, the altered vessels are removed through punctures that are brought out with special hooks, the veins are not ligated, and sutures are not placed on the skin. The puncture is sealed with an aseptic sticker. There are practically no puncture marks left. This operation is called miniphlebectomy and is performed on an outpatient basis under local anesthesia.
The most modern method is laser surgery to remove varicose veins. The operation is performed under local anesthesia; if the patient wishes, general anesthesia is performed. The essence of the operation is as follows: through a puncture in the shin area, a thin laser probe is inserted through a catheter into the lumen of the great saphenous vein to the point where it flows into the femoral vein. This procedure is performed under ultrasound guidance. After this, a hydraulic cushion is created around the vein, along its entire length, with a novocaine solution. The point of the pillow is that when laser exposure is applied to the wall of a vessel, the temperature in the surrounding tissues rises, the layer of liquid around the vein reduces the temperature effect on the tissues adjacent to it, in addition, novocaine acts as an anesthetic. Therefore, the purpose of the hydrocushion is to protect the tissue around the vein from burns that can result from laser energy, and at the same time anesthetize the surgical field.
After this, the laser is turned on and the inner walls of the vessel are treated with it. The power, pulse frequency and laser exposure time are calculated based on the data of each patient. As a result, the walls of the vein are deformed, stick together and form a dense cord. After 6-12 months, the vein resolves and the cord disappears. This laser operation for varicose veins of the lower extremities is called Endovasal Laser Coagulation (ablation), abbreviated as EVLT or EVLA.
Any operation, including laser surgery for varicose veins, requires preoperative examination and preparation. In terms of examination, it is necessary, in addition to duplex scanning of the veins, to take a test for infections and sugar, general and biochemical blood tests, conduct a study of the blood coagulation system, fluorography, and an electrocardiogram. People in the older age group are prescribed ultrasound examination of the heart (heart echo), ultrasound examination of the carotid arteries. Anyone planning laser surgery to remove varicose veins should be examined by a therapist and an anesthesiologist. On the eve of the operation, it is necessary to take a shower, shave the hair in the groin and along the inner surfaces of the legs and thighs, in the area of the intended surgical intervention. On the morning of the operation, you should not eat or drink water. You can only rinse in your mouth.
After the operation, compression garments of class 2 compression are put on everyone’s legs. We recommend leaving the stockings on for three days, and then putting them on only during the day and taking them off at night. In total, stockings need to be worn for 7 days. If the operation was performed under spinal anesthesia, then after 4-5 hours the sensitivity in the legs is completely restored, and the patient can go home on his own. If laser surgery for varicose veins in the legs was performed under local anesthesia, the patient can go home within an hour.
The essence of the procedure
The EVLT procedure involves the introduction of a laser light guide into the lumen of the altered vein, which ensures “welding” of its internal lining. After laser surgery on the veins in the lower limb, venous blood flow is normalized, the phenomena of venous stagnation disappear, the heaviness and swelling of the legs, and trophic disorders are eliminated.
Due to the direct effect on the altered vein wall, the surrounding tissues are not heated during the procedure, which ensures a minimal number of hematomas after EVLT and significant relief of the postoperative period.
The procedure is performed under ultrasound control and most often lasts no more than two hours. To perform endovasal laser coagulation, local anesthesia is used and no incisions are required. After the operation, it is necessary to apply a special compression bandage to the operated leg.
Technique for performing endovasal laser ablation of veins
Preparing the patient for the intervention
Laser endovasal obliteration of veins does not require any special preparation of the patient for manipulation. The preoperative stage includes only a set of standard tests and examinations that any clinic does before hospitalizing the patient. As preparation, the limb on which the procedure is to be performed is also shaved.
Actually, before EVLO, the patient is marked on the skin under ultrasound control - they mark the border of reflux (reverse flow) along the vein that is to be treated with the laser, as well as the places where the tributaries flow into it. If the tributaries are varicose, this is also noted.
Step-by-step technique for performing endovasal laser obliteration
Stage 1: puncture of the vein being treated, insertion of a laser light guide into it, placement of the working part of the light guide according to the markings made before the intervention.
Stage 2: anesthesia, which includes, in addition to long-acting anesthetics, vasoconstrictor drugs. This method of anesthesia reduces the likelihood of postoperative hemorrhages and increases the effectiveness of the intervention. If necessary (and at the request of the patient), pain relief can be supplemented with general intravenous anesthesia.
Stage 3: carrying out the actual EVLO - treatment of the vessel with a laser beam until coagulation of the inner wall is achieved.
Stage 4: providing compression of the limb on which the intervention was performed by bandaging with an elastic bandage or wearing compression stockings.
Advantages
This modern method of combating varicose veins, offered by phlebologists at the Yusupov Hospital Therapy Clinic, has a number of undeniable advantages:
- there is no inguinal incision or other incisions on the lower limb;
- there is no need to use general anesthesia;
- short recovery period;
- no need for bed rest;
- safety of EVLC – constant monitoring by ultrasound;
- absence of discomfort and pain - the procedure is carried out using local anesthesia;
- absence of postoperative scars and scars, excessive pigmentation;
- complete obliteration within 3 months and relief from varicose veins in almost 98% of cases after EVLT (relapses practically do not occur);
- minimal risk of developing postoperative complications;
- easy and fast rehabilitation period.
To achieve a higher aesthetic result, patients at the Yusupov Hospital Therapy Clinic are offered to combine EVLT and microphlebectomy, which helps solve the problem of dilated veins even with large varicose veins.
The rehabilitation period after EVLT is quite easy. Patients are recommended to use compression stockings - thin, elastic knitwear that maintains a given degree of pressure. Thanks to laser treatment of varicose veins, patients retain their ability to work and their quality of life does not deteriorate.
THERE ARE 3 TYPES OF VARICOSE VEINS:
1. Intradermal varicose veins (telangiectasias, also known as “spider veins”)
2. Subcutaneous varicose veins (reticular veins, “webs”)
3. Varicose veins in the system of the great and/or small saphenous veins
Possible complications
A relatively common complication after EVLT is relapses, the occurrence of which is most often recorded in patients predisposed to the development of varicose veins.
Intraoperative mechanical nerve damage occurs extremely rarely during EVLT. However, thanks to the high qualifications and professional skills of the surgeons at the Yusupov Hospital and the innovative medical equipment of the clinic, such complications are practically excluded.
Sometimes it happens that the vein remains swollen after EVLT. This complication occurs if the technique of the procedure was not followed: the laser beam did not influence the vein sufficiently. However, cases where a vein swells after EVLT are very rare.
As a rule, complications develop in patients who ignore compliance with postoperative recommendations.
Physiotherapy
Recommended for almost all forms and stages of varicose veins. Below is an example set of exercises:
| Initial position | Exercises | Number of repetitions |
| Lying on your back, the foot end of the couch is raised 20-25 cm + arms along the body, legs apart | Simultaneous flexion and extension of the feet and fingers | 10-12 |
| The same + legs straightened | Alternate flexion and extension of the legs at the knee joints | 3-6 times with each leg |
| Same | Bend your left leg, pull it to your chest, straighten it up, hold it and slowly lower it. Same with the right foot. | Same |
| Same + legs apart | Toes and knees in and out | 8-10 |
| The same + hands to shoulders | Circular movements in the shoulder joints | 4-5 times each way |
| The same + legs bent, hands on stomach | Tilts of bent legs to the right and left | 6-8 |
| The same + legs straightened | Alternate flexion and extension of the feet with reinforcement - “pressing the pedals” | 6-12 |
| Same + hands behind head | Bicycle leg movement | 6-8 movements 2-3 times |
| The same + legs bent, arms along the body | Alternately raise your legs up with a delay at the top - movements of the toes and active circular movements of the foot | Repeat 2-3 times |
| Lying on your left side, the foot end of the couch is lowered to a horizontal level, your left hand under your cheek, your right hand on your thigh, your legs are bent | Raise your right arm and leg up | 4-5 |
| Lying on your left side, hold onto the couch with your right hand | Swinging the right leg back and forth | 6-8 |
| The same Repeat the last 3 exercises lying on your right side | Flexion and extension of the feet | 8-12 |
| Standing facing the wall and holding onto the bar | Rise onto your toes, roll onto your heels and back onto your toes. | 5-6 |
Cones
The most common post-operative disorder is lumps after laser surgery for varicose veins. Their appearance is associated with excessively intense physical activity.
To prevent the development of lumps, the patient must temporarily stop moving and wear compression garments for the first two days after surgery.
In addition, blood flow can also increase under the influence of heat - while taking a bath or in a sauna or bathhouse. For this reason, it is not recommended to visit baths and saunas for two to three weeks after EVLT.
Preparing for EVLT
Before the operation, the patient is prescribed an examination. A duplex scan of the blood vessels in the legs is required. The procedure makes it possible to assess the condition of varicose veins and determine the amount of work to be done.
Standard preparation required before surgery:
- urine and blood tests;
- ECG;
- chest x-ray
- Examination by a therapist and other specialists as indicated.
A few days before laser coagulation, it is necessary to stop taking anticoagulants (blood thinners) and hormonal drugs. You should first consult your doctor about this.
On the day of EVLT, you should not eat food 4 hours before the procedure. Compression stockings should be prepared to wear after surgery.
What to do if your leg hurts after the intervention?
Some patients may experience discomfort when attempting to fully extend the leg. They disappear on their own within one to two months after EVLT.
Since the essence of the procedure is that the vein is heated by a laser, after the end of anesthesia at the site of exposure, patients often feel pain caused by overheating of the muscles surrounding the blood vessel. Such pain usually disappears after 10-14 days.
If pain in the lower extremity continues to bother the patient for more than two weeks, it is recommended to visit a doctor, which will help to promptly prevent a rare but dangerous complication of EVLT - thrombosis or thromboembolism.
Why do varicose veins occur?
Varicose veins occur when the functioning of the vein valves is impaired. This leads to disruption of venous outflow and dilation of veins. It cannot be said that only women are susceptible to such disorders; men also experience this disease. According to statistics, 67% of women and 50% of men have chronic diseases of the veins of the lower extremities. These disappointing statistics show that, regardless of gender, more than half of the population of our country is susceptible to varicose veins.
So how can you prevent the appearance of varicose veins? Diagnose it and treat it?
First things first. The first and most important thing to know is that there is no prevention for varicose veins. You need to be prepared for the fact that varicose veins may appear regardless of how you live, what your lifestyle is, nutrition and other behavioral factors. There is no prevention, but there are symptoms and factors that can affect the premature appearance and manifestation of varicose veins.
Symptoms:
- Constantly painful and swollen legs (heaviness in the legs and increased fatigue of the legs)
- By the end of the day, shoes become tight and uncomfortable
- The “pattern” of socks on the feet becomes very clearly visible
- A blue-red “web” of vessels on the legs began to appear (spider veins on the legs)
- Night leg cramps
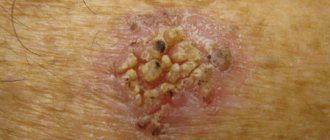
- Itching, redness, dermatitis, eczema on the legs, trophic ulcers
- Tendency to varicose veins (you have already been/are being seen by a phlebologist)
All these symptoms are signals from the body and you urgently need to visit a phlebologist. If for various reasons you do not hear your body, this can lead to varicose veins and manifest themselves more clearly. When varicose veins appear, unfortunately, you will have to forget about skirts and clothes that allow you to show off your legs, which is very unpleasant for most women. The varicose veins themselves, if they do appear, should under no circumstances be neglected and ignored. As soon as the first symptoms appear, you must immediately make an appointment with a doctor. It is important to understand that varicose veins are a disease and it has complications that can cause serious harm to the patient’s health. For example, dermatitis, ulcers and bleeding can not only deprive a person of his ability to work for a long time, but also lead to disability. The formation of blood clots in varicose veins is also a serious complication. As many years of practice have shown, varicose veins cannot be cured with massage, tablets or ointments. A reduction in symptoms is possible, but not a complete recovery! And the external manifestations of varicose veins will not allow you to feel confident when wearing skirts or undressing on the beach. Those. In addition to external inconveniences, the patient also feels psychological discomfort from this disease and limits himself when choosing clothes and lifestyle.
If you have any suspicions about the appearance and development of varicose veins, do not delay, visit a doctor. In our clinic, you can undergo a full examination (diagnostics) - examination of the veins, which will help to accurately identify problems and make a diagnosis, or dispel your doubts. If suspicions are confirmed, our specialists will help you choose an individual course of treatment and get rid of varicose veins.
Thromboembolic complications
The main danger after laser treatment of varicose veins is the development of thromboembolic complications. In order to minimize the likelihood of this complication, phlebologists at the Yusupov Hospital recommend observing the following preventive measures:
- during the postoperative period, apply and wear an elastic bandage;
- use elastic bandages on the legs of patients with deep vein valve insufficiency;
- in the early postoperative period, limit physical activity;
- use anticoagulant drugs in patients with high blood clotting.
The above recommendations should be followed for at least two weeks after EVLT, which is the key to effective treatment and prevention of the development of postoperative complications.
Indications and contraindications
Laser coagulation of varicose veins on the legs is indicated in the following cases:
- Varicose veins of an uncomplicated course. Laser exposure will be effective for any diameter of dilated venous trunks. This is evidenced by our more than 10-year surgical practice and experience in treating over 5,000 patients.
- Trophic ulcers of the leg. The use of a laser (EVLK) makes it possible to achieve accelerated closure of the ulcerative wound surface - in most cases, without resorting to autodermoplasty;
- Venous malformations and developmental anomalies of the subcutaneous venous network. Dilatation of large diameter vessels, the treatment of which is combined with other operations. Often in such situations, laser coagulation is carried out in conjunction with classical phlebectomy - surgical removal of varicose veins.
Contraindications for endovascular laser coagulation of veins:
- the diameter of the affected vein is more than 40 mm (!), when we are talking about venous aneurysms;
- purulent inflammation of the skin at the site of surgery;
- inability to walk due to other diseases (problems with the musculoskeletal system, previous stroke, etc.);
- arterial stenosis in the legs;
- increased blood clotting;
- thrombosis of the main veins;
- acute and chronic diseases of internal organs in the acute stage;
- infectious diseases;
- obesity in the last stages, as it prevents postoperative adequate compression;
- pregnancy;
- lactation period.